Abstract
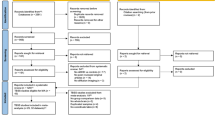
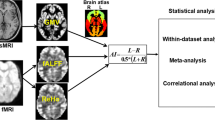
To investigate the quantitative profiles of brain grey matter (GM) in pediatric drug-naïve ADHD patients using synthetic magnetic resonance imaging (SyMRI). A total of 37 drug-naïve pediatric ADHD and 27 age- and gender-matched healthy controls (HC) were enrolled in this study. Each subject underwent both SyMRI and conventional 3D T1-FSPGR scans. Quantitative parameters, T1 and T2 maps, were extracted from the SyMRI data. Between-group quantitative maps were compared using a general linear model analysis. Pearson correlation analysis was conducted to assess the association between significantly altered MR indices and clinical measurements in ADHD. Compared with the HC group, altered T1 and T2 relaxometry times in the ADHD group were mainly distributed in GM regions of the cerebellum, attention and execution control network, default mode network, and limbic areas. Moreover, the T1 value of the right cerebellum 8 was negatively correlated with the attention concentration level in ADHD (R = 0.140, P = 0.0225). With regards to T2 map, the associations were observed between the attention level of ADHD patients and left fusiform gyrus (R = 0.251, P = 0.0016), and right cerebellum crus2 (R = 0.142, P = 0.0214). Altered T1, T2 values found in specific regions of GM, including cerebellum, attention and execution control network, default mode network, and limbic areas, may reveal widespread micromorphology changes, i.e., brain iron deficiency, low myelin content, and enlarged vascular interstitial space in ADHD patients. Thus, T1, T2 values might be promising imaging markers for future ADHD studies.


Similar content being viewed by others
Abbreviations
- ADHD:
-
Attention-deficit/hyperactivity disorder
- HC:
-
Healthy control
- GM:
-
Grey matter
- SyMRI:
-
Synthetic magnetic resonance imaging
- DMN:
-
Default mode network
- EAN:
-
Attention and execution control network
- QSM:
-
Quantitative susceptibility mapping
- VN:
-
Visual network
- SMN:
-
Sensorimotor network
References
Albajara Saenz, A., Villemonteix, T., & Massat, I. (2019). Structural and functional neuroimaging in attention-deficit/hyperactivity disorder. Development Medicine and Child Neurology, 61(4), 399–405.
Ambrosino, S., de Zeeuw, P., Wierenga, L. M., et al. (2017). What can cortical development in attention-deficit/hyperactivity disorder teach us about the early developmental mechanisms involved? Cerebral Cortex, 27(9), 4624–4634.
Andica, C., Hagiwara, A., Hori, M., et al. (2019). Review of synthetic MRI in pediatric brains: Basic principle of MR quantification, its features, clinical applications, and limitations. Journal of Neuroradiology 46(4), 268–275.
Bralten, J., Greven, C. U., Franke, B., et al. (2016). Voxel-based morphometry analysis reveals frontal brain differences in participants with ADHD and their unaffected siblings. Journal of Psychiatry & Neuroscience, 41(4), 272–279.
Cao, M., Shu, N., Cao, Q., et al. (2014). Imaging functional and structural brain connectomics in attention-deficit/hyperactivity disorder. Molecular Neurobiology, 50(3), 1111–1123.
Caye, A., Rocha, T. B., Anselmi, L., et al. (2016). Attention-deficit/hyperactivity disorder trajectories from childhood to young adulthood: Evidence from a birth cohort supporting a late-onset syndrome. JAMA Psychiatry, 73(7), 705–712.
Cheng, Q. Q., Huang, J. X., Liang, J. Y., et al. (2020). Evaluation of abnormal iron distribution in specific regions in the brains of patients with Parkinson’s disease using quantitative susceptibility mapping and R2*mapping. Experimental and Therapeutic Medicine, 19(6), 3778–3786.
Deoni, S. C., Zinkstok, J. R., Daly, E., et al. (2015). White-matter relaxation time and myelin water fraction differences in young adults with autism. Psychological Medicine, 45(4), 795–805.
Does, M. D. (2018). Inferring brain tissue composition and microstructure via MR relaxometry. NeuroImage, 182, 136–148.
Edwards, L. J., Kirilina, E., Mohammadi, S., et al. (2018). Microstructural imaging of human neocortex in vivo. NeuroImage, 182, 184–206.
Frodl, T., & Skokauskas, N. (2012). Meta-analysis of structural MRI studies in children and adults with attention deficit hyperactivity disorder indicates treatment effects. Acta Psychiatrica Scandinavica, 125(2), 114–126.
Hagiwara, A., Hori, M., Yokoyama, K., et al. (2017). Utility of a multiparametric quantitative MRI Model that assesses myelin and edema for evaluating plaques, periplaque white matter, and normal-appearing white matter in patients with multiple sclerosis: A feasibility study. American Journal of Neuroradiology, 38(2), 237–242.
Hoogman, M., Bralten, J., Hibar, D. P., et al. (2017). Subcortical brain volume differences in participants with attention deficit hyperactivity disorder in children and adults: A cross-sectional mega-analysis. Lancet Psychiatry, 4(4), 310–319.
Jiang, W. H., Duan, K. K., Chen, J. Y., et al. (2019). Structural brain alterations and their association with cognitive function and symptoms in attention-deficit/hyperactivity disorder families. European Neuropsychopharmacology, 29, 1189–1190.
Kupeli, A., Kocak, M., Goktepeli, M., et al. (2020). Role of T1 mapping to evaluate brain aging in a healthy population. Clinical Imaging, 59(1), 56–60.
Lei, X., Wang, Y., Yuan, H., et al. (2014). Neuronal oscillations and functional interactions between resting state networks. Human Brain Mapping, 35(7), 3517–3528.
Lorio, S., Kherif, F., Ruef, A., et al. (2016). Neurobiological origin of spurious brain morphological changes: A quantitative MRI study. Human Brain Mapping, 37(5), 1801–1815.
Megna, R., Alfano, B., Lanzillo, R., et al. (2019). Brain tissue volumes and relaxation rates in multiple sclerosis: Implications for cognitive impairment. Journal of Neurology, 266(2), 361–368.
Norman, L. J., Carlisi, C., Lukito, S., et al. (2016). Structural and functional brain abnormalities in attention-deficit/hyperactivity disorder and obsessive-compulsive disorder: A comparative meta-analysis. JAMA Psychiatry, 73(8), 815–825.
Posner, J., Park, C., & Wang, Z. (2014). Connecting the dots: A review of resting connectivity MRI studies in attention-deficit/hyperactivity disorder. Neuropsychology Review, 24(1), 3–15.
Qian, X., Castellanos, F. X., Uddin, L. Q., et al. (2019). Large-scale brain functional network topology disruptions underlie symptom heterogeneity in children with attention-deficit/hyperactivity disorder. Neuroimage Clinical, 21, 101600.
Samea, F., Soluki, S., Nejati, V., et al. (2019). Brain alterations in children/adolescents with ADHD revisited: A neuroimaging meta-analysis of 96 structural and functional studies. Neuroscience and Biobehavioral Reviews, 100, 1–8.
Stuber, C., Morawski, M., Schafer, A., et al. (2014). Myelin and iron concentration in the human brain: A quantitative study of MRI contrast. NeuroImage, 93(Pt 1), 95–106.
Sun, L., Cao, Q., Long, X., et al. (2012). Abnormal functional connectivity between the anterior cingulate and the default mode network in drug-naïve boys with attention deficit hyperactivity disorder. Psychiatry Research, 201(2), 120–127.
Thapar, A., & Cooper, M. (2016). Attention deficit hyperactivity disorder. The Lancet, 387(10024), 1240–1250.
Thomas, R., Sanders, S., Doust, J., et al. (2015). Prevalence of attention-deficit/hyperactivity disorder: A systematic review and meta-analysis. Pediatrics, 135(4), e994–1001.
Vogt, B. A. (2019). Cingulate impairments in ADHD: Comorbidities, connections, and treatment. Handbook of Clinical Neurology, 166, 297–314.
Wang, L. J., Li, S. C., Kuo, H. C., et al. (2020b). Gray matter volume and microRNA levels in patients with attention-deficit/hyperactivity disorder. European Archives of Psychiatry and Clinical Neuroscience, 270(8), 1037–1045.
Wang, Y., Sun, K., Liu, Z., et al. (2020a). Classification of unmedicated bipolar disorder using whole-brain functional activity and connectivity: A radiomics analysis. Cerebral Cortex, 30(3), 1117–1128.
Wardlaw, J. M., Benveniste, H., Nedergaard, M., et al. (2020). Perivascular spaces in the brain: Anatomy, physiology and pathology. Nature Reviews Neurology, 16(3), 137–153.
Warntjes, J. B., Leinhard, O. D., West, J., et al. (2008). Rapid magnetic resonance quantification on the brain: Optimization for clinical usage. Magnetic Resonance in Medicine, 60(2), 320–329.
Wu, Z. M., Llera, A., Hoogman, M., et al. (2019). Linked anatomical and functional brain alterations in children with attention-deficit/hyperactivity disorder. Neuroimage Clinical, 23, 101851.
Acknowledgements
We would like to thank the participants and their families, as well as the staff at the MRI at the First Affiliated Hospital of Sun Yat-sen University, for making this study possible.
Funding
This work was supported by the Natural Science Fund Youth Science Fund Project of China [Grant Number 82001439] and the Medical Scientific Research Foundation of Guangdong Province [Grant NumbersA2020327].
Author information
Authors and Affiliations
Contributions
Author contributions included: Conceptualization and study design, SS, YC; Methodology, SS, YD, LQ; Investigation, SS, LL, QZ, MZ, HZ, ML, XX; Formal Analysis, SS, LL; Writing—Original Draft, SS, YC; Writing—Review & Editing, SS, YC, ZY, LQ, QZ, MZ, HZ, ML, XX; Visualization, SS. and agreement to be accountable for the integrity and accuracy of all aspects of the work (All authors).
Corresponding authors
Ethics declarations
Conflict of interest
None. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the article's subject matter.
Ethics approval
This study was approved by the institutional review board of the First Affiliated Hospital of Sun Yat-sen University (No. [2019]328).
Informed consent
Written informed consent was obtained from the guardians of all the subjects (patients) in this study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Su, S., Chen, Y., Dai, Y. et al. Quantitative synthetic MRI reveals grey matter abnormalities in children with drug-naïve attention-deficit/hyperactivity disorder. Brain Imaging and Behavior 16, 406–414 (2022). https://doi.org/10.1007/s11682-021-00514-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11682-021-00514-8