Abstract
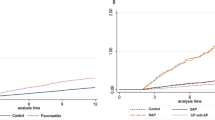
Incidences of pancreatic cancer and acute and chronic pancreatitis are rising globally, and often no curative treatment is available at the time of diagnosis. We tested the hypothesis that low and high plasma concentrations of pancreatic amylase are associated with increased risk of pancreatic cancer, acute pancreatitis, and chronic pancreatitis in the general population. We included 101,765 individuals (55% women) aged 20–100 years from the Copenhagen General Population Study with baseline measurements of plasma pancreatic amylase. After recruitment in 2004–2015 during a median 9 years of follow-up (range 0–15), we collected information about diagnoses of pancreatic cancer, acute pancreatitis, and chronic pancreatitis from the national Danish Patient Registry, the national Danish Cancer Registry, and the national Danish Causes of Death Registry. The median age was 58 years (interquartile range: 48–67) and the median plasma pancreatic amylase 32 U/L (26–40). During follow-up, 442 individuals were diagnosed with pancreatic cancer, 282 with chronic pancreatitis, and 401 with acute pancreatitis. Compared to individuals with pancreatic amylase levels in the 41st–60th percentiles, those with extreme low (1st–2.5th percentiles) and extreme high (97.5th–100th percentiles) pancreatic amylase had hazard ratios of 2.4 (95% confidence interval; 1.6–3.6) and 2.2 (1.4–3.7) for pancreatic cancer, of 1.8 (1.1–3.3) and 3.2 (1.8–5.6) for chronic pancreatitis, and of 1.1 (0.6–1.8) and 1.5 (0.8–2.7) for acute pancreatitis, respectively. In apparently healthy individuals from the general population, extreme low and extreme high plasma pancreatic amylase were associated with 2–threefold higher risk of both pancreatic cancer and chronic pancreatitis.




Similar content being viewed by others
Availability of data and material
Data will be made available upon reasonable request to corresponding author.
References
Xiao AY, Tan ML, Wu LM, et al. Global incidence and mortality of pancreatic diseases: a systematic review, meta-analysis, and meta-regression of population-based cohort studies. Lancet Gastroenterol Hepatol. 2016;1(1):45–55. https://doi.org/10.1016/s2468-1253(16)30004-8.
Rawla P, Sunkara T, Gaduputi V. Epidemiology of pancreatic cancer: global trends, etiology and risk factors. World J Oncol. 2019;10(1):10–27. https://doi.org/10.14740/wjon1166.
Boxhoorn L, Voermans RP, Bouwense SA, et al. Acute pancreatitis. Lancet (London, England). 2020;396(10252):726–34. https://doi.org/10.1016/s0140-6736(20)31310-6.
Beyer G, Habtezion A, Werner J, Lerch MM, Mayerle J. Chronic pancreatitis. Lancet (London, England). 2020;396(10249):499–512. https://doi.org/10.1016/s0140-6736(20)31318-0.
Khalaf N, El-Serag HB, Abrams HR, Thrift AP. Burden of Pancreatic Cancer: From Epidemiology to Practice. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2020; https://doi.org/10.1016/j.cgh.2020.02.054
Habtezion A. Inflammation in acute and chronic pancreatitis. Curr Opin Gastroenterol. 2015;31(5):395–9. https://doi.org/10.1097/mog.0000000000000195.
Machicado JD, Yadav D. Epidemiology of recurrent acute and chronic pancreatitis: similarities and differences. Dig Dis Sci. 2017;62(7):1683–91. https://doi.org/10.1007/s10620-017-4510-5.
Ahmed Ali U, Issa Y, Hagenaars JC, et al. Risk of recurrent pancreatitis and progression to chronic pancreatitis after a first episode of acute pancreatitis. Clinical gastroenterol hepatol: Off Clin Pract J Am Gastroenterol Assoc. 2016;14(5):738–46. https://doi.org/10.1016/j.cgh.2015.12.040.
Sankaran SJ, Xiao AY, Wu LM, Windsor JA, Forsmark CE, Petrov MS. Frequency of progression from acute to chronic pancreatitis and risk factors: a meta-analysis. Gastroenterology. 2015;149(6):1490-1500.e1. https://doi.org/10.1053/j.gastro.2015.07.066.
Hori Y, Vege SS, Chari ST, et al. Classic chronic pancreatitis is associated with prior acute pancreatitis in only 50% of patients in a large single-institution study. Pancreatology : official journal of the International Association of Pancreatology (IAP) [et al]. Mar 2019;19(2):224–229. doi:https://doi.org/10.1016/j.pan.2019.02.004
Raimondi S, Lowenfels AB, Morselli-Labate AM, Maisonneuve P, Pezzilli R. Pancreatic cancer in chronic pancreatitis; aetiology, incidence, and early detection. Best Pract Res Clin Gastroenterol. 2010;24(3):349–58. https://doi.org/10.1016/j.bpg.2010.02.007.
McGuigan A, Kelly P, Turkington RC, Jones C, Coleman HG, McCain RS. Pancreatic cancer: a review of clinical diagnosis, epidemiology, treatment and outcomes. World J Gastroenterol. 2018;24(43):4846–61. https://doi.org/10.3748/wjg.v24.i43.4846.
Crockett SD, Wani S, Gardner TB, Falck-Ytter Y, Barkun AN. American gastroenterological association institute guideline on initial management of acute pancreatitis. Gastroenterology. 2018;154(4):1096–101. https://doi.org/10.1053/j.gastro.2018.01.032.
IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology : official journal of the International Association of Pancreatology (IAP) [et al]. 2013;13(4 Suppl 2):e1–15. doi:https://doi.org/10.1016/j.pan.2013.07.063
Ito T, Ishiguro H, Ohara H, et al. Evidence-based clinical practice guidelines for chronic pancreatitis 2015. J Gastroenterol. 2016;51(2):85–92. https://doi.org/10.1007/s00535-015-1149-x.
Gardner TB, Adler DG, Forsmark CE, Sauer BG, Taylor JR, Whitcomb DC. ACG Clinical Guideline: Chronic Pancreatitis. Official journal of the American College of Gastroenterology | ACG. 2020;115(3):322–339. doi:https://doi.org/10.14309/ajg.0000000000000535
Löhr JM, Dominguez-Munoz E, Rosendahl J, et al. United European Gastroenterology evidence-based guidelines for the diagnosis and therapy of chronic pancreatitis (HaPanEU). United Eur gastroenterol J. 2017;5(2):153–99. https://doi.org/10.1177/2050640616684695.
Sohal DPS, Kennedy EB, Cinar P, et al. Metastatic Pancreatic Cancer: ASCO Guideline Update. J Clin Oncol. 2020:Jco2001364. doi:https://doi.org/10.1200/jco.20.01364
Ducreux M, Cuhna AS, Caramella C, et al. Cancer of the pancreas: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015;26(Suppl 5):v56-68. https://doi.org/10.1093/annonc/mdv295.
Conwell DL, Lee LS, Yadav D, et al. American pancreatic association practice guidelines in chronic pancreatitis: evidence-based report on diagnostic guidelines. Pancreas. 2014;43(8):1143–62. https://doi.org/10.1097/mpa.0000000000000237.
Olesen SS, Krarup H, Poulsen JL, et al. Pancreas-specific plasma amylase for assessment and diagnosis of chronic pancreatitis: New insights on an old topic. United Eur gastroenterol J. 2019;7(7):955–64. https://doi.org/10.1177/2050640619846011.
Sonne DP, Vilsbøll T, Knop FK. Pancreatic amylase and lipase plasma concentrations are unaffected by increments in endogenous GLP-1 levels following liquid meal tests. Diabetes Care. 2015;38(5):e71–2. https://doi.org/10.2337/dc14-2751.
Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the management of blood cholesterol: a report of the American college of cardiology/american heart association task force on clinical practice guidelines. J Am Coll Cardiol. 2019;73(24):e285–350. https://doi.org/10.1016/j.jacc.2018.11.003.
Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41(1):111–88. https://doi.org/10.1093/eurheartj/ehz455.
Nordestgaard BG, Langsted A, Mora S, et al. Fasting is not routinely required for determination of a lipid profile: clinical and laboratory implications including flagging at desirable concentration cut-points-a joint consensus statement from the European atherosclerosis society and european federation of clinical chemistry and laboratory medicine. Eur Heart J. 2016;37(25):1944–58. https://doi.org/10.1093/eurheartj/ehw152.
Kim YS, Chang JH, Kim TH, Kim CW, Kim JK, Han SW. Prolonged hyperamylasemia in patients with acute pancreatitis is associated with recurrence of acute pancreatitis. Medicine (Baltimore). 2020;99(3): e18861. https://doi.org/10.1097/md.0000000000018861.
Acharya C, Cline RA, Jaligama D, et al. Fibrosis reduces severity of acute-on-chronic pancreatitis in humans. Gastroenterology. 2013;145(2):466–75. https://doi.org/10.1053/j.gastro.2013.05.012.
Sollie S, Michaud DS, Sarker D, et al. Chronic inflammation markers are associated with risk of pancreatic cancer in the Swedish AMORIS cohort study. BMC Cancer. 2019;19(1):858. https://doi.org/10.1186/s12885-019-6082-6.
S Rasch I Valantiene A Mickevicius et al 2016 Chronic pancreatitis: Do serum biomarkers provide an association with an inflammageing phenotype? Pancreatology : official journal of the International Association of Pancreatology (IAP) [et al] Sep-Oct 16 5 708 714 https://doi.org/10.1016/j.pan.2016.08.004
Hansen SEJ, Madsen CM, Varbo A, Nordestgaard BRG. Low-grade inflammation in the association between mild-to-moderate hypertriglyceridemia and risk of acute pancreatitis: a study of more than 115000 individuals from the general population. Clin Chem. 2018. https://doi.org/10.1373/clinchem.2018.294926.
Syed A, Babich O, Thakkar P, et al. Defining pancreatitis as a risk factor for pancreatic cancer: the role, incidence, and timeline of development. Pancreas. 2019;48(8):1098–101. https://doi.org/10.1097/mpa.0000000000001367.
Pereira SP, Oldfield L, Ney A, et al. Early detection of pancreatic cancer. Lancet Gastroenterol Hepatol. 2020;5(7):698–710. https://doi.org/10.1016/s2468-1253(19)30416-9.
Goggins M, Overbeek KA, Brand R, et al. Management of patients with increased risk for familial pancreatic cancer: updated recommendations from the international cancer of the pancreas screening (CAPS) consortium. Gut. 2020;69(1):7–17. https://doi.org/10.1136/gutjnl-2019-319352.
Kirkegård J, Mortensen FV, Cronin-Fenton D. chronic pancreatitis and pancreatic cancer risk: a systematic review and meta-analysis. Am J Gastroenterol. 2017;112(9):1366–72. https://doi.org/10.1038/ajg.2017.218.
Nakajima K. Low serum amylase and obesity, diabetes and metabolic syndrome: a novel interpretation. World J Diabetes. 2016;7(6):112–21. https://doi.org/10.4239/wjd.v7.i6.112.
Mössner J, Logsdon CD, Williams JA, Goldfine ID. Insulin, via its own receptor, regulates growth and amylase synthesis in pancreatic acinar AR42J cells. Diabetes. 1985;34(9):891–7. https://doi.org/10.2337/diab.34.9.891.
Seyama K, Nukiwa T, Takahashi K, Takahashi H, Kira S. Amylase mRNA transcripts in normal tissues and neoplasms: the implication of different expressions of amylase isogenes. J Cancer Res Clin Oncol. 1994;120(4):213–20. https://doi.org/10.1007/bf01372559.
Acknowledgements
We would like to thank staff and participants from the Copenhagen General Population Study for their valuable contributions.
Funding
This work was funded by the Novo Nordisk Foundation, Denmark, the Independent Research Fund Denmark, Herlev and Gentofte Hospital, Copenhagen University Hospital, Denmark, and Chief Physician Johan Boserup and Lise Boserup’s Fund, Denmark. The Copenhagen General Population Study was supported by Herlev and Gentofte Hospital, Copenhagen University Hospital, the Danish Heart Foundation, the Danish Medical Research Council, the Copenhagen County Foundation.
Author information
Authors and Affiliations
Contributions
SEJH, AL, and BGN had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analyses. Study concept and design: SEJH, AL, and BGN. Acquisition, analyses and interpretation of data: SEJH, AL, and BGN. Drafting of manuscript: SEJH. Critical revision of the manuscript for important intellectual content: AL, AV, CMM, ATH, and BGN. Statistical analyses: SEJH and AL. Study supervision: AL, AV, CMM, ATH, and BGN.
Corresponding author
Ethics declarations
Conflict of Interest
BGN reports consultancies or talks sponsored by AstraZeneca, Sanofi, Regeneron, Akcea, Amgen, Kowa, Denka, Amarin, Novartis, Novo Nordisk, Esperion, and Silence Therapeutics. ATH reports consultancies for AstraZeneca, Silence Therapeutics, Novartis, Sanofi, Akcea, and Draupnir Bio. AV and CMM are currently employed at Novo Nordisk. SEJH and AL have no conflicts of interest.
Code availability
Coding will be made available upon reasonable request to corresponding author.
Ethical approval
The study was conducted in accordance with the Declaration of Helsinki and approved by local institutional reviews boards and Danish ethical committees (H-KF-01–144/01). Consent to participate: Written informed consent was obtained from all individuals.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hansen, S.E.J., Langsted, A., Varbo, A. et al. Low and high pancreatic amylase is associated with pancreatic cancer and chronic pancreatitis. Eur J Epidemiol 36, 975–984 (2021). https://doi.org/10.1007/s10654-021-00801-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-021-00801-0