Abstract
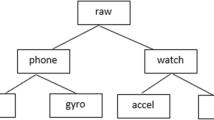
Wearable devices equipped with sensors popularly used for health monitoring are capable of accumulating motion data providing objective measures of various physical activity and sleep attributes. Also, smartphone usage has grown to an extent where phones have become an integral part of lifestyle contributing to users’ screen viewing time. Behavior and behavioral attributes of individuals’ personal characteristics are significant components of lifestyle of which sleep, physical activity and screen viewing correspond to the most occupied time throughout the day and among the major lifestyle patterns affecting overall health. This study aims to assess sleep quality and behavioral health from wearables and smartphones using an Adaptive Neuro-Fuzzy Inference System (ANFIS). Real time physical activity and sleep data have been collected from users’ smartwatches. A smartphone application is built to collect real time smartphone usage data. Sleep quality indicator (SleepQual) for assessment of daily sleep quality is calculated using sleep attributes collected from smartwatches. Correlation of SleepQual is evaluated with physical activity attributes and smartphone usage attributes using Pearson’s correlation. Highly correlated attributes along with sleep attributes are used to train the ANFIS model for sleep quality assessment. A novel behavioral health indicator (B. Health) is proposed which is evaluated using real time physical activity, sleep and screen time data. Attributes are ranked on the basis of Pearson’s correlation with B. Health to identify the most important contributors to behavioral health. Top ranked features are selected to train the ANFIS model for behavioral health assessment. Systematic Minority Oversampling Technique has been used for data augmentation. The ANFIS model achieves an accuracy of 91.69% for sleep quality assessment and 85.79% for behavioral health assessment.




















Similar content being viewed by others
References
Mak, Y.W.; Wu, C.S.T.; Hui, D.W.S.; Lam, S.P.; Tse, H.Y.; Yu, W.Y.; Wong, H.T.: Association between screen viewing duration and sleep duration, sleep quality, and excessive daytime sleepiness among adolescents in Hong Kong. Int. J. Environ. Res. Public Health 11(11), 11201–11219 (2014)
Holmberg, L.I.; Hellberg, D.: Behavioral and other characteristics of relevance for health in adolescents with self-perceived sleeping problems. Int. J. Adolesc. Med. Health 20(3), 353–365 (2008)
Reilly, J.J.; Penpraze, V.; Hislop, J.; Davies, G.; Grant, S.; Paton, J.Y.: Objective measurement of physical activity and sedentary behaviour: review with new data. Arch. Dis. Child. 93(7), 614–619 (2008)
Sylvia, L.G.; Bernstein, E.E.; Hubbard, J.L.; Keating, L.; Anderson, E.J.: Practical guide to measuring physical activity. J. Acad. Nutr. Diet. 114(2), 199–208 (2014)
Vallance, J.K.; Buman, M.P.; Stevinson, C.; Lynch, B.M.: Associations of overall sedentary time and screen time with sleep outcomes. Am. J. Health Behav. 39(1), 62–67 (2015)
Olds, T.S.; Maher, C.A.; Matricciani, L.: Sleep duration or bedtime? Exploring the relationship between sleep habits and weight status and activity patterns. Sleep 34(10), 1299–1307 (2011)
Carter, B.; Rees, P.; Hale, L.; Bhattacharjee, D.; Paradkar, M.S.: Association between portable screen-based media device access or use and sleep outcomes: a systematic review and meta-analysis. JAMA Pediatr. 170(12), 1202–1208 (2016)
Anderson, M.; Jiang, J.: Teens, social media & technology 2018. Pew Research Center 31(2018), 1673–1689 (2018)
Arora, A.; Chakraborty, P.; Bhatia, M.P.S.: Problematic use of digital technologies and its impact on mental health during COVID-19 pandemic: assessment using machine learning. In: Arpaci, I., Al-Emran, M., Al-Sharafi, M.A., Marques, G. (eds.) Emerging Technologies During the Era of COVID-19 Pandemic (2020) (in press)
Arora, A.; Chakraborty, P.; Bhatia, M.P.S.: Analysis of data from wearable sensors for sleep quality estimation and prediction using deep learning. Arab. J. Sci. Eng. 45(12), 10793–10812 (2020)
Jacobs, D.R., Jr.; Ainsworth, B.E.; Hartman, T.J.; Leon, A.S.: A simultaneous evaluation of 10 commonly used physical activity questionnaires. Med. Sci. Sports Exerc. 25(1), 81–91 (1993)
Shephard, R.J.: Limits to the measurement of habitual physical activity by questionnaires. Br. J. Sports Med. 37(3), 197–206 (2003)
Smith, K.A.; Gallagher, M.; Hays, A.E.; Goss, F.L.; Robertson, R.: Development of the physical activity index as a measure of total activity load and total kilocalorie expenditure during submaximal walking. J. Phys. Act. Health 9(6), 757–764 (2012)
Corder, K.; Brage, S.; Ekelund, U.: Accelerometers and pedometers: methodology and clinical application. Curr. Opin. Clin. Nutr. Metab. Care 10(5), 597–603 (2007)
Tudor-Locke, C.; Brashear, M.M.; Johnson, W.D.; Katzmarzyk, P.T.: Accelerometer profiles of physical activity and inactivity in normal weight, overweight, and obese US men and women. Int. J. Behav. Nutr. Phys. Act. 7(1), 1–11 (2010)
Rachele, J.N.; McPhail, S.M.; Washington, T.L.; Cuddihy, T.F.: Practical physical activity measurement in youth: a review of contemporary approaches. World Journal of Pediatrics 8(3), 207–216 (2012)
de Arriba-Pérez, F.; Caeiro-Rodríguez, M.; Santos-Gago, J.M.: How do you sleep? Using off the shelf wrist wearables to estimate sleep quality, sleepiness level, chronotype and sleep regularity indicators. J. Ambient. Intell. Humaniz. Comput. 9(4), 897–917 (2018)
Montgomery-Downs, H.E.; Insana, S.P.; Bond, J.A.: Movement toward a novel activity monitoring device. Sleep Breath. 16(3), 913–917 (2012)
Poirier, J.; Bennett, W.L.; Jerome, G.J.; Shah, N.G.; Lazo, M.; Yeh, H.C.; Clark, J.M.; Cobb, N.K.: Effectiveness of an activity tracker-and internet-based adaptive walking program for adults: a randomized controlled trial. J. Med. Internet Res. 18(2), e34 (2016)
Lu, T.C.; Fu, C.M.; Ma, M.H.M.; Fang, C.C.; Turner, A.M.: Healthcare applications of smart watches: a systematic review. Appl. Clin. Inform. 7(3), 850 (2016)
Hawi, N.S.; Samaha, M.: To excel or not to excel: strong evidence on the adverse effect of smartphone addiction on academic performance. Comput. Educ. 98, 81–89 (2016)
LeBourgeois, M.K.; Hale, L.; Chang, A.M.; Akacem, L.D.; Montgomery-Downs, H.E.; Buxton, O.M.: Digital media and sleep in childhood and adolescence. Pediatrics 140(Supplement 2), S92–S96 (2017)
Thomée, S.; Härenstam, A.; Hagberg, M.: Mobile phone use and stress, sleep disturbances, and symptoms of depression among young adults-a prospective cohort study. BMC Public Health 11(1), 66 (2011)
Vernon, L.; Modecki, K.L.; Barber, B.L.: Mobile phones in the bedroom: trajectories of sleep habits and subsequent adolescent psychosocial development. Child Dev. 89(1), 66–77 (2018)
Chen, M.; Mao, S.; Liu, Y.: Big data: a survey. Mobile Netw. Appl. 19(2), 171–209 (2014)
Kumar, A.; Jaiswal, A.: Systematic literature review of sentiment analysis on Twitter using soft computing techniques. Concurrency Comput. Pract. Exp. 32(1), e5107 (2020)
Jordan, M.I.; Mitchell, T.M.: Machine learning: trends, perspectives, and prospects. Science 349(6245), 255–260 (2015)
Shatte, A.B.; Hutchinson, D.M.; Teague, S.J.: Machine learning in mental health: a scoping review of methods and applications. Psychol. Med. 49(9), 1426–1448 (2019)
Kumar, A.; Arora, A.: An ANFIS-based compatibility scorecard for IoT integration in websites. J. Supercomput. 1–29 (2019)
Foti, K.E.; Eaton, D.K.; Lowry, R.; McKnight-Ely, L.R.: Sufficient sleep, physical activity, and sedentary behaviors. Am. J. Prev. Med. 41(6), 596–602 (2011)
Stone, M.R.; Stevens, D.; Faulkner, G.E.: Maintaining recommended sleep throughout the week is associated with increased physical activity in children. Prev. Med. 56(2), 112–117 (2013)
Brand, S.; Gerber, M.; Beck, J.; Hatzinger, M.; Pühse, U.; Holsboer-Trachsler, E.: High exercise levels are related to favorable sleep patterns and psychological functioning in adolescents: a comparison of athletes and controls. J. Adolesc. Health 46(2), 133–141 (2010)
Wu, X.; Tao, S.; Zhang, Y.; Zhang, S.; Tao, F. Low physical activity and high screen time can increase the risks of mental health problems and poor sleep quality among Chinese college students. PLoS ONE 10(3), e0119607 (2015)
Xu, F.; Adams, S.K.; Cohen, S.A.; Earp, J.E.; Greaney, M.L.: Relationship between physical activity, screen time, and sleep quantity and quality in US adolescents aged 16–19. Int. J. Environ. Res. Public Health 16(9), 1524 (2019)
Kredlow, M.A.; Capozzoli, M.C.; Hearon, B.A.; Calkins, A.W.; Otto, M.W.: The effects of physical activity on sleep: a meta-analytic review. J. Behav. Med. 38(3), 427–449 (2015)
Feng, Q.; Du, Y.; Ye, Y.L.; He, Q.Q.: Associations of physical activity, screen time with depression, anxiety and sleep quality among Chinese college freshmen. PLoS ONE 9(6), e100914 (2014)
Infante, S.; Zapatero, L.; Zubeldia, J. 2020. 10. Anderson M, Jiang J. Teens, Social Media & Technology 2018. Pew Research Center; 2018. Available from: https://www.pewinternet.org/2018/05/31/teens-social-media-technology-2018/11. Curtis BL, Ashford RD, Magnuson KI, Ryan-Pettes SR. J. Investig. Allergol. Clin. Immunol. 30(2), 133–155 (2014)
Johansson, A.E.; Petrisko, M.A.; Chasens, E.R.: Adolescent sleep and the impact of technology use before sleep on daytime function. J. Pediatr. Nurs. 31(5), 498–504 (2016)
Christensen, M.A.; Bettencourt, L.; Kaye, L.; Moturu, S.T.; Nguyen, K.T.; Olgin, J.E.; Pletcher, M.J.; Marcus, G.M.: Direct measurements of smartphone screen-time: relationships with demographics and sleep. PLoS ONE 11(11), e0165331 (2016)
Lou, Z.; Wang, L.; Jiang, K.; Wei, Z.; Shen, G.: Reviews of wearable healthcare systems: Materials, devices and system integration. Mater. Sci. Eng. R Rep. 140, 100523 (2020)
Papa, A.; Mital, M.; Pisano, P.; Del Giudice, M.: E-health and wellbeing monitoring using smart healthcare devices: an empirical investigation. Technol. Forecast. Soc. Change 153, 119226 (2020)
Sherratt, R.S.; Nilanjan, D.: Low-power wearable healthcare sensors 892 (2020)
Li, S.; Ma, Z.; Cao, Z.; Pan, L.; Shi, Y.: Advanced wearable microfluidic sensors for healthcare monitoring. Small 16(9), 1903822 (2020)
Wang, Y.; Chao, M.; Wan, P.; Zhang, L.: A wearable breathable pressure sensor from metal-organic framework derived nanocomposites for highly sensitive broad-range healthcare monitoring. Nano Energy 70 104560 (2020)
Pang, Y.; Yang, Z.; Yang, Y.; Ren, T.L.: Wearable electronics based on 2D materials for human physiological information detection. Small 16(15), 1901124 (2020)
Jin, J.; Gao, B.; Yang, S.; Zhao, B.; Luo, L.; Woo, W.L.: Attention-block deep learning based features fusion in wearable social sensor for mental wellbeing evaluations. IEEE Access 8, 89258–89268 (2020)
Tazawa, Y.; Liang, K.C.; Yoshimura, M.; Kitazawa, M.; Kaise, Y.; Takamiya, A.; Kishi, A.; Horigome, T.; Mitsukura, Y.; Mimura, M.; Kishimoto, T.: Evaluating depression with multimodal wristband-type wearable device: screening and assessing patient severity utilizing machine-learning. Heliyon 6(2), e03274 (2020)
Zhao, S.; Zhao, Q.; Zhang, X.; Peng, H.; Yao, Z.; Shen, J.; Yao, Y.; Jiang, H.; Hu, B.: Wearable EEG-based real-time system for depression monitoring. In: International Conference on Brain Informatics, pp. 190–201. Springer, Cham (2017, November)
Sandulescu, V.; Andrews, S.; Ellis, D.; Bellotto, N.; Mozos, O.M.: Stress detection using wearable physiological sensors. In: International Work-Conference on the Interplay Between Natural and Artificial Computation, pp. 526–532. Springer, Cham (2015)
Gjoreski, M.; Gjoreski, H.; Luštrek, M.; Gams, M.: Continuous stress detection using a wrist device: in laboratory and real life. In: Proceedings of the 2016 ACM International Joint Conference on Pervasive and Ubiquitous Computing: Adjunct, pp. 1185–1193 (2016, September)
Alharthi, R.; Alharthi, R.; Guthier, B.; El Saddik, A.: CASP: context-aware stress prediction system. Multimedia Tools and Applications 78(7), 9011–9031 (2019)
Rabbi, M.; Ali, S.; Choudhury, T.; Berke, E.: Passive and in-situ assessment of mental and physical well-being using mobile sensors. In: Proceedings of the 13th International Conference on Ubiquitous Computing, pp. 385–394 (2011, September)
Kamdar, M.R.; Wu, M.J.: PRISM: a data-driven platform for monitoring mental health. In: Biocomputing 2016: Proceedings of the Pacific Symposium, pp. 333–344 (2016)
Kumar, A.; Sharma, K.; Sharma, A.: Hierarchical deep neural network for mental stress state detection using IoT based biomarkers. Pattern Recognit. Lett. (2021)
Hossain, H.S.; Ramamurthy, S.R.; Khan, M.A.A.H.; Roy, N.: An active sleep monitoring framework using wearables. ACM Trans. Interact. Intell. Syst. (TiiS) 8(3), 1–30 (2018)
Sathyanarayana, A.; Joty, S.; Fernandez-Luque, L.; Ofli, F.; Srivastava, J.; Elmagarmid, A.; Arora, T.; Taheri, S.: Sleep quality prediction from wearable data using deep learning. JMIR mHealth and uHealth 4(4), e125 (2016)
Patel, P.; Kim, J.Y.; Brooks, L.J.: Accuracy of a smartphone application in estimating sleep in children. Sleep Breath. 21(2), 505–511 (2017)
Toon, E.; Davey, M.J.; Hollis, S.L.; Nixon, G.M.; Horne, R.S.; Biggs, S.N.: Comparison of commercial wrist-based and smartphone accelerometers, actigraphy, and PSG in a clinical cohort of children and adolescents. J. Clin. Sleep Med. 12(3), 343–350 (2016)
Tal, A.; Shinar, Z.; Shaki, D.; Codish, S.; Goldbart, A.: Validation of contact-free sleep monitoring device with comparison to polysomnography. J. Clin. Sleep Med. 13(3), 517–522 (2017)
Bhat, S.; Ferraris, A.; Gupta, D.; Mozafarian, M.; DeBari, V.A.; Gushway-Henry, N.; Gowda, S.P.; Polos, P.G.; Rubinstein, M.; Seidu, H.; Chokroverty, S.: Is there a clinical role for smartphone sleep apps? Comparison of sleep cycle detection by a smartphone application to polysomnography. J. Clin. Sleep Med. 11(7), 709–715 (2015)
Behar, J.; Roebuck, A.; Shahid, M.; Daly, J.; Hallack, A.; Palmius, N.; Stradling, J.; Clifford, G.D.: SleepAp: an automated obstructive sleep apnoea screening application for smartphones. IEEE J. Biomed. Health Inform. 19(1), 325–331 (2014)
Nakano, H.; Hirayama, K.; Sadamitsu, Y.; Toshimitsu, A.; Fujita, H.; Shin, S.; Tanigawa, T.: Monitoring sound to quantify snoring and sleep apnea severity using a smartphone: proof of concept. J. Clin. Sleep Med. 10(1), 73–78 (2014)
Scott, H.; Lack, L.; Lovato, N.: A pilot study of a novel smartphone application for the estimation of sleep onset. J. Sleep Res. 27(1), 90–97 (2018)
Chen, Z.; Lin, M.; Chen, F.; Lane, N.D.; Cardone, G.; Wang, R.; Li, T.; Chen, Y.; Choudhury, T.; Campbell, A.T.: Unobtrusive sleep monitoring using smartphones. In: 2013 7th International Conference on Pervasive Computing Technologies for Healthcare and Workshops, pp. 145–152. IEEE (2013, May)
Farhan, A.A.; Lu, J.; Bi, J.; Russell, A.; Wang, B.; Bamis, A.: Multi-view bi-clustering to identify smartphone sensing features indicative of depression. In: 2016 IEEE First International Conference on Connected Health: Applications, Systems and Engineering Technologies (CHASE), pp. 264–273. IEEE (2016, June)
Stütz, T.; Kowar, T.; Kager, M.; Tiefengrabner, M.; Stuppner, M.; Blechert, J.; Wilhelm, F.H.; Ginzinger, S.: Smartphone based stress prediction. In: International Conference on User Modeling, Adaptation, and Personalization, pp. 240–251. Springer, Cham (2015, June)
Cao, B.; Zheng, L.; Zhang, C.; Yu, P.S.; Piscitello, A.; Zulueta, J.; Ajilore, O.; Ryan, K.; Leow, A.D.: Deepmood: modeling mobile phone typing dynamics for mood detection. In: Proceedings of the 23rd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, pp. 747–755 (2017, August)
Maxhuni, A.; Hernandez-Leal, P.; Morales, E.F.; Sucar, L.E.; Osmani, V.; Muńoz-Meléndez, A.; Mayora, O.: Using intermediate models and knowledge learning to improve stress prediction. In: Applications for Future Internet, pp. 140–151. Springer, Cham (2017)
Shin, C.; Dey, A.K.: Automatically detecting problematic use of smartphones. In: Proceedings of the 2013 ACM International Joint Conference on Pervasive and Ubiquitous Computing, pp. 335–344 (2013, September)
Lawanont, W.; Inoue, M.: A development of classification model for smartphone addiction recognition system based on smartphone usage data. In: International Conference on Intelligent Decision Technologies, pp. 3–12. Springer, Cham (2017, June)
Ellis, D.A.; Davidson, B.I.; Shaw, H.; Geyer, K.: Do smartphone usage scales predict behavior? Int. J. Hum Comput Stud. 130, 86–92 (2019)
Kim, S.K.; Kang, H.B.: An analysis of smartphone overuse recognition in terms of emotions using brainwaves and deep learning. Neurocomputing 275, 1393–1406 (2018)
de Arriba Pérez, F.; Gago, J.M.S.; Rodríguez, M.C.: Calculation of sleep indicators in students using smartphones and wearables. In: New Advances in Information Systems and Technologies, pp. 169–178. Springer, Cham (2016)
Sano, A.; Phillips, A.J.; Amy, Z.Y.; McHill, A.W.; Taylor, S.; Jaques, N.; Czeisler, C.A.; Klerman, E.B.; Picard, R.W.: Recognizing academic performance, sleep quality, stress level, and mental health using personality traits, wearable sensors and mobile phones. In: 2015 IEEE 12th International Conference on Wearable and Implantable Body Sensor Networks (BSN), pp. 1–6. IEEE (2015, June)
Cvetković, B.; Gjoreski, M.; Šorn, J.; Maslov, P.; Luštrek, M.: Monitoring physical activity and mental stress using wrist-worn device and a smartphone. In: Joint European Conference on Machine Learning and Knowledge Discovery in Databases, pp. 414–418. Springer, Cham (2017, September)
Buysse, D.J.; Reynolds, C.F., III.; Monk, T.H.; Berman, S.R.; Kupfer, D.J.: The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 28(2), 193–213 (1989)
Tudor-Locke, C.; Bassett, D.R.: How many steps/day are enough? Sports Med. 34(1), 1–8 (2004)
Bassett, D.R.; Toth, L.P.; LaMunion, S.R.; Crouter, S.E.: Step counting: a review of measurement considerations and health-related applications. Sports Med. 47(7), 1303–1315 (2017)
Council on Communications and Media. Children, adolescents, and the media. Pediatrics 132, 958–961 (2013). https://pediatrics.aappublications.org/content/132/5/958
Chawla, N.V.; Bowyer, K.W.; Hall, L.O.; Kegelmeyer, W.P.: SMOTE: synthetic minority over-sampling technique. J. Artif. Intell. Res. 16, 321–357 (2002)
Gnanambal, S.; Thangaraj, M.; Meenatchi, V.T.; Gayathri, V.: Classification algorithms with attribute selection: an evaluation study using WEKA. Int. J. Adv. Netw. Appl. 9(6), 3640–3644 (2018)
Kumar, A.; Arora, A.: A filter-wrapper based feature selection for optimized website quality prediction. In: 2019 Amity International Conference on Artificial Intelligence (AICAI), pp. 284–291. IEEE (2019, February)
Arora, A.: Soft Computing Techniques for Web Quality Analytics (Doctoral dissertation) (2019)
Han, P.; Li, L.; Zhang, H.; Guan, L.; Marques, C.; Savović, S.; Ortega, B.; Min, R.; Li, X.: Low-cost plastic optical fiber sensor embedded in mattress for sleep performance monitoring. Opt. Fiber Technol. 64, 102541 (2021)
Kumar, A.; Arora, A.: Website quality analytics using Metaheuristic based optimization. Recent Adv. Comput. Sci. Commun. 14(3), 901–921 (2021)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Arora, A., Chakraborty, P. & Bhatia, M.P.S. Intervention of Wearables and Smartphones in Real Time Monitoring of Sleep and Behavioral Health: An Assessment Using Adaptive Neuro-Fuzzy Technique. Arab J Sci Eng 47, 1999–2024 (2022). https://doi.org/10.1007/s13369-021-06078-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13369-021-06078-5