Abstract
Cardiac amyloidosis, a form of infiltrative cardiomyopathy, is associated with poor prognosis in untreated patients. Early diagnosis is important for timely initiation of effective therapies. Despite advances in diagnostic modalities, it remains a challenging diagnosis, requiring high index of clinical suspicion. Echocardiography represents the first-line cardiac imaging modality for evaluation of heart failure and suspected cardiac amyloidosis. In this review, we discuss echocardiographic findings in cardiac amyloidosis.






Similar content being viewed by others
Abbreviations
- EFSR:
-
Ratio of left ventricular ejection fraction to global longitudinal strain
- LV:
-
Left ventricle
- RV:
-
Right ventricle
- TDI:
-
Tissue Doppler imaging
- ST:
-
Speckle tracking
References
Sipe JD, Benson MD, Buxbaum JN et al (2014) Nomenclature 2014: amyloid fibril proteins and clinical classification of the amyloidosis. Amyloid 21(4):221–224. https://doi.org/10.3109/13506129.2014.964858
Smith TJ, Kyle RA, Lie JT (1984) Clinical significance of histopathologic patterns of cardiac amyloidosis. Mayo Clin Proc 59(8):547–555. https://doi.org/10.1016/s0025-6196(12)61493-1
Ladefoged B, Dybro A, Povlsen JA, Vase H, Clemmensen TS, Poulsen SH (2020) Diagnostic delay in wild type transthyretin cardiac amyloidosis - a clinical challenge. Int J Cardiol 304:138–143. https://doi.org/10.1016/j.ijcard.2019.12.063
Adams D, Gonzalez-Duarte A, O’Riordan WD et al (2018) Patisiran, an RNAi therapeutic, for hereditary transthyretin amyloidosis. N Engl J Med 379(1):11–21. https://doi.org/10.1056/NEJMoa1716153
Benson MD, Waddington-Cruz M, Berk JL et al (2018) Inotersen treatment for patients with hereditary transthyretin amyloidosis. N Engl J Med 379(1):22–31. https://doi.org/10.1056/NEJMoa1716793
Maurer MS, Schwartz JH, Gundapaneni B et al (2018) Tafamidis treatment for patients with transthyretin amyloid cardiomyopathy. N Engl J Med 379(11):1007–1016. https://doi.org/10.1056/NEJMoa1805689
Sanchorawala V, Wright DG, Seldin DC et al (2004) High-dose intravenous melphalan and autologous stem cell transplantation as initial therapy or following two cycles of oral chemotherapy for the treatment of AL amyloidosis: results of a prospective randomized trial. Bone Marrow Transplant 33(4):381–388. https://doi.org/10.1038/sj.bmt.1704346
Kyle RA, Linos A, Beard CM et al (1992) Incidence and natural history of primary systemic amyloidosis in Olmsted County, Minnesota, 1950 through 1989. Blood 79(7):1817–1822
Dubrey SW, Cha K, Anderson J et al (1998) The clinical features of immunoglobulin light-chain (AL) amyloidosis with heart involvement. QJM 91(2):141–157. https://doi.org/10.1093/qjmed/91.2.141
Kyle RA, Gertz MA (1995) Primary systemic amyloidosis: clinical and laboratory features in 474 cases. Semin Hematol 32(1):45–59
González-López E, Gallego-Delgado M, Guzzo-Merello G et al (2015) Wild-type transthyretin amyloidosis as a cause of heart failure with preserved ejection fraction. Eur Heart J 36(38):2585–2594. https://doi.org/10.1093/eurheartj/ehv338
Castaño A, Narotsky DL, Hamid N et al (2017) Unveiling transthyretin cardiac amyloidosis and its predictors among elderly patients with severe aortic stenosis undergoing transcatheter aortic valve replacement. Eur Heart J 38(38):2879–2887. https://doi.org/10.1093/eurheartj/ehx350
Ihse E, Ybo A, Suhr O, Lindqvist P, Backman C, Westermark P (2008) Amyloid fibril composition is related to the phenotype of hereditary transthyretin V30M amyloidosis. J Pathol 216(2):253–261. https://doi.org/10.1002/path.2411
Ng B, Connors LH, Davidoff R, Skinner M, Falk RH (2005) Senile systemic amyloidosis presenting with heart failure: a comparison with light chain-associated amyloidosis. Arch Intern Med 165(12):1425–1429. https://doi.org/10.1001/archinte.165.12.1425
Pellikka PA, Holmes DR Jr, Edwards WD, Nishimura RA, Tajik AJ, Kyle RA (1988) Endomyocardial biopsy in 30 patients with primary amyloidosis and suspected cardiac involvement. Arch Intern Med 148(3):662–666
Deckers JW, Hare JM, Baughman KL (1992) Complications of transvenous right ventricular endomyocardial biopsy in adult patients with cardiomyopathy: a seven-year survey of 546 consecutive diagnostic procedures in a tertiary referral center. J Am Coll Cardiol 19(1):43–47. https://doi.org/10.1016/0735-1097(92)90049-s
Roberts WC, Waller BF (1983) Cardiac amyloidosis causing cardiac dysfunction: analysis of 54 necropsy patients. Am J Cardiol 52(1):137–146. https://doi.org/10.1016/0002-9149(83)90084-x
Brenner DA, Jain M, Pimentel DR et al (2004) Human amyloidogenic light chains directly impair cardiomyocyte function through an increase in cellular oxidant stress. Circ Res 94(8):1008–1010. https://doi.org/10.1161/01.res.0000126569.75419.74
Buja LM, Khoi NB, Roberts WC (1970) Clinically significant cardiac amyloidosis. Clinicopathologic findings in 15 patients. Am J Cardiol 26(4):394–405. https://doi.org/10.1016/0002-9149(70)90736-8
Feng D, Edwards WD, Oh JK et al (2007) Intracardiac thrombosis and embolism in patients with cardiac amyloidosis. Circulation 116(21):2420–2426. https://doi.org/10.1161/circulationaha.107.697763
Plehn JF, Southworth J, Cornwell GG 3rd (1992) Brief report: atrial systolic failure in primary amyloidosis. N Engl J Med 327(22):1570–1573. https://doi.org/10.1056/nejm199211263272205
Gertz MA, Comenzo R, Falk RH et al (2005) Definition of organ involvement and treatment response in immunoglobulin light chain amyloidosis (AL): a consensus opinion from the 10th International Symposium on Amyloid and Amyloidosis, Tours, France, 18–22 April 2004. Am J Hematol 79(4):319–328. https://doi.org/10.1002/ajh.20381
Cueto-Garcia L, Reeder GS, Kyle RA et al (1985) Echocardiographic findings in systemic amyloidosis: spectrum of cardiac involvement and relation to survival. J Am Coll Cardiol 6(4):737–743. https://doi.org/10.1016/s0735-1097(85)80475-7
Lang RM, Badano LP, Mor-Avi V et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28(1):1-39.e14. https://doi.org/10.1016/j.echo.2014.10.003
Dinwoodey DL, Skinner M, Maron MS, Davidoff R, Ruberg FL (2008) Light-chain amyloidosis with echocardiographic features of hypertrophic cardiomyopathy. Am J Cardiol 101(5):674–676. https://doi.org/10.1016/j.amjcard.2007.10.031
Sedlis SP, Saffitz JE, Schwob VS, Jaffe AS (1984) Cardiac amyloidosis simulating hypertrophic cardiomyopathy. Am J Cardiol 53(7):969–970. https://doi.org/10.1016/0002-9149(84)90543-5
Falk RH, Plehn JF, Deering T et al (1987) Sensitivity and specificity of the echocardiographic features of cardiac amyloidosis. Am J Cardiol 59(5):418–422. https://doi.org/10.1016/0002-9149(87)90948-9
Bhandari AK, Nanda NC (1983) Myocardial texture characterization by two-dimensional echocardiography. Am J Cardiol 51(5):817–825. https://doi.org/10.1016/s0002-9149(83)80139-8
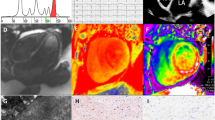
Dorbala S, Ando Y, Bokhari S et al (2019) ASNC/AHA/ASE/EANM/HFSA/ISA/SCMR/SNMMI expert consensus recommendations for multimodality imaging in cardiac amyloidosis: Part 1 of 2-evidence base and standardized methods of imaging. J Nucl Cardiol 2065–2123 vol 6
Carroll JD, Gaasch WH, McAdam KP (1982) Amyloid cardiomyopathy: characterization by a distinctive voltage/mass relation. Am J Cardiol 49(1):9–13. https://doi.org/10.1016/0002-9149(82)90270-3
Siqueira-Filho AG, Cunha CL, Tajik AJ, Seward JB, Schattenberg TT, Giuliani ER (1981) M-mode and two-dimensional echocardiographic features in cardiac amyloidosis. Circulation 63(1):188–196. https://doi.org/10.1161/01.cir.63.1.188
Quarta CC, Solomon SD, Uraizee I et al (2014) Left ventricular structure and function in transthyretin-related versus light-chain cardiac amyloidosis. Circulation 129(18):1840–1849. https://doi.org/10.1161/circulationaha.113.006242
Patel AR, Dubrey SW, Mendes LA et al (1997) Right ventricular dilation in primary amyloidosis: an independent predictor of survival. Am J Cardiol 80(4):486–492. https://doi.org/10.1016/s0002-9149(97)00400-1
Fitzgerald BT, Scalia GM, Cain PA, Garcia MJ, Thomas JD (2011) Left atrial size–another differentiator for cardiac amyloidosis. Heart Lung Circ 20(9):574–578. https://doi.org/10.1016/j.hlc.2011.06.002
Scully PR, Patel KP, Treibel TA et al (2020) Prevalence and outcome of dual aortic stenosis and cardiac amyloid pathology in patients referred for transcatheter aortic valve implantation. Eur Heart J 41(29):2759–2767. https://doi.org/10.1093/eurheartj/ehaa170
Treibel TA, Fontana M, Gilbertson JA et al (2016) Occult transthyretin cardiac amyloid in severe calcific aortic stenosis: prevalence and prognosis in patients undergoing surgical aortic valve replacement. Circ Cardiovasc Imaging 9(8). https://doi.org/10.1161/circimaging.116.005066
Nitsche C, Scully PR, Patel KP et al (2021) Prevalence and outcomes of concomitant aortic stenosis and cardiac amyloidosis. J Am Coll Cardiol 77(2):128–139. https://doi.org/10.1016/j.jacc.2020.11.006
Binder C, Duca F, Binder T et al (2021) Prognostic implications of pericardial and pleural effusion in patients with cardiac amyloidosis. Clin Res Cardiol 110(4):532–543. https://doi.org/10.1007/s00392-020-01698-7
Klein AL, Hatle LK, Burstow DJ et al (1989) Doppler characterization of left ventricular diastolic function in cardiac amyloidosis. J Am Coll Cardiol 13(5):1017–1026. https://doi.org/10.1016/0735-1097(89)90254-4
Nagueh SF, Smiseth OA, Appleton CP et al (2016) Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the american Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 29(4):277–314. https://doi.org/10.1016/j.echo.2016.01.011
Klein AL, Hatle LK, Burstow DJ et al (1990) Comprehensive doppler assessment of right ventricular diastolic function in cardiac amyloidosis. J Am Coll Cardiol 15(1):99–108. https://doi.org/10.1016/0735-1097(90)90183-p
Mohty D, Pibarot P, Dumesnil JG et al (2011) Left atrial size is an independent predictor of overall survival in patients with primary systemic amyloidosis. Arch Cardiovasc Dis 104(12):611–618. https://doi.org/10.1016/j.acvd.2011.10.004
Nochioka K, Quarta CC, Claggett B et al (2017) Left atrial structure and function in cardiac amyloidosis. Eur Heart J Cardiovasc Imaging 18(10):1128–1137. https://doi.org/10.1093/ehjci/jex097
Knight DS, Zumbo G, Barcella W et al (2019) Cardiac structural and functional consequences of amyloid deposition by cardiac magnetic resonance and echocardiography and their prognostic roles. JACC Cardiovasc Imaging 12(5):823–833. https://doi.org/10.1016/j.jcmg.2018.02.016
Tendler A, Helmke S, Teruya S, Alvarez J, Maurer MS (2015) The myocardial contraction fraction is superior to ejection fraction in predicting survival in patients with AL cardiac amyloidosis. Amyloid 22(1):61–66. https://doi.org/10.3109/13506129.2014.994202
Pagourelias ED, Mirea O, Duchenne J et al (2017) Echo parameters for differential diagnosis in cardiac amyloidosis: a head-to-head comparison of deformation and nondeformation parameters. Circ Cardiovasc Imaging 10(3):e005588. https://doi.org/10.1161/circimaging.116.005588
Milani P, Dispenzieri A, Scott CG et al (2018) Independent prognostic value of stroke volume index in patients with immunoglobulin light chain amyloidosis. Circ Cardiovasc Imaging 11(5):e006588. https://doi.org/10.1161/circimaging.117.006588
Koyama J, Ray-Sequin PA, Davidoff R, Falk RH (2002) Usefulness of pulsed tissue Doppler imaging for evaluating systolic and diastolic left ventricular function in patients with AL (primary) amyloidosis. Am J Cardiol 89(9):1067–1071. https://doi.org/10.1016/s0002-9149(02)02277-4
Koyama J, Ray-Sequin PA, Falk RH (2003) Longitudinal myocardial function assessed by tissue velocity, strain, and strain rate tissue Doppler echocardiography in patients with AL (primary) cardiac amyloidosis. Circulation 107(19):2446–2452. https://doi.org/10.1161/01.cir.0000068313.67758.4f
Pagourelias ED, Duchenne J, Mirea O et al (2016) The relation of ejection fraction and global longitudinal strain in amyloidosis: implications for differential diagnosis. JACC Cardiovasc Imaging 9(11):1358–1359. https://doi.org/10.1016/j.jcmg.2015.11.013
Phelan D, Collier P, Thavendiranathan P et al (2012) Relative apical sparing of longitudinal strain using two-dimensional speckle-tracking echocardiography is both sensitive and specific for the diagnosis of cardiac amyloidosis. Heart 98(19):1442–1448. https://doi.org/10.1136/heartjnl-2012-302353
Liu D, Hu K, Niemann M et al (2013) Effect of combined systolic and diastolic functional parameter assessment for differentiation of cardiac amyloidosis from other causes of concentric left ventricular hypertrophy. Circ Cardiovasc Imaging 6(6):1066–1072. https://doi.org/10.1161/circimaging.113.000683
Bravo PE, Fujikura K, Kijewski MF et al (2019) Relative apical sparing of myocardial longitudinal strain is explained by regional differences in total amyloid mass rather than the proportion of amyloid deposits. JACC Cardiovasc Imaging 12(7 Pt 1):1165–1173. https://doi.org/10.1016/j.jcmg.2018.06.016
Sperry BW, Vranian MN, Tower-Rader A et al (2018) Regional variation in technetium pyrophosphate uptake in transthyretin cardiac amyloidosis and impact on mortality. JACC Cardiovasc Imaging 11(2 Pt 1):234–242. https://doi.org/10.1016/j.jcmg.2017.06.020
Bellavia D, Pellikka PA, Dispenzieri A et al (2012) Comparison of right ventricular longitudinal strain imaging, tricuspid annular plane systolic excursion, and cardiac biomarkers for early diagnosis of cardiac involvement and risk stratification in primary systematic (AL) amyloidosis: a 5-year cohort study. Eur Heart J Cardiovasc Imaging 13(8):680–689. https://doi.org/10.1093/ehjci/jes009
Boldrini M, Cappelli F, Chacko L et al (2020) Multiparametric echocardiography scores for the diagnosis of cardiac amyloidosis. JACC Cardiovasc Imaging 13(4):909–920. https://doi.org/10.1016/j.jcmg.2019.10.011
Huda A, Castaño A, Niyogi A et al (2021) A machine learning model for identifying patients at risk for wild-type transthyretin amyloid cardiomyopathy. Nat Commun 12(1):2725. https://doi.org/10.1038/s41467-021-22876-9
Goto S, Mahara K, Beussink-Nelson L et al (2021) Artificial intelligence-enabled fully automated detection of cardiac amyloidosis using electrocardiograms and echocardiograms. Nat Commun 12(1):2726. https://doi.org/10.1038/s41467-021-22877-8
Pozo E, Kanwar A, Deochand R et al (2014) Cardiac magnetic resonance evaluation of left ventricular remodelling distribution in cardiac amyloidosis. Heart 100(21):1688–1695. https://doi.org/10.1136/heartjnl-2014-305710
Kittleson MM, Maurer MS, Ambardekar AV et al (2020) Cardiac amyloidosis: evolving diagnosis and management: a scientific statement from the American Heart Association. Circulation 142(1):e7–e22. https://doi.org/10.1161/cir.0000000000000792
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Agrawal, T., Nagueh, S.F. Echocardiographic assessment of cardiac amyloidosis. Heart Fail Rev 27, 1505–1513 (2022). https://doi.org/10.1007/s10741-021-10165-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-021-10165-y