Supporting and Protecting People with Dementia in the COVID-19 Pandemic
Abstract
We aimed to explore the awareness and preparedness of dementia caregivers and people with mild cognitive deficits on how to prevent COVID-19 infection and cope with the indirect consequences of the pandemic. A total of 139 patient-caregiver dyads received a telephone survey and 109 completed the survey. The majority of respondents reported having a moderate-to-good knowledge of the typical manifestations of COVID-19. Conversely, only few of them were informed of the atypical presentations and on how to recognize emergency warning signs. Filling the knowledge gaps on COVID-19 in the most vulnerable people may represent a significant resource to tackle the pandemic.
INTRODUCTION
People with dementia have been disproportionately affected by the COVID-19 pandemic, from multiple perspectives [1]. First of all, dementia has repeatedly been found to increase the risk of contracting severe infections and experiencing COVID-19-related adverse outcomes, including death. In several Western countries, about 20–25%of people who died with the evidence of SARS-CoV-2 infection had dementia [2]. Accordingly, a recent metanalysis documented that dementia is associated with a four-fold increase in mortality risk after contagion [3]. Such vulnerability of people with dementia to unfavorable courses has been attributed to various determinants including advanced age, comorbidities, reduced access to intensive care and advanced treatments, as well as to the residency in those care settings (i.e., nursing homes) that were initially unprepared to manage the outbreak [2, 4]. Furthermore, the tendency of COVID-19 to manifest with atypical presentations (e.g., delirium, absence of fever and cough, exacerbation of preexisting neuropsychiatric symptoms, falls) in older, cognitively impaired people may have contributed to late diagnosis and treatment and, therefore, to higher mortality [5].
In parallel, people with dementia who did not contract SARS-CoV-2 infection are also indirectly affected by the pandemic. Several studies, primarily based on telephone interviews with caregivers, have shown that a high proportion of patients exhibited a significant decline in their cognitive functioning and functional independence and a significant exacerbation of behavioral disorders during the different waves of the pandemic [6, 7]. Such clinical worsening is likely due to the changes in daily routines, the inability to rely on strategies for controlling behavioral manifestations (e.g., going out for a walk), the prolonged isolation, and the suspension of dedicated services (e.g., daycare centers) imposed by the adopted restrictive measures [5–7].
In October 2020, the Italian Dementia National Plan Working Group released an “Interim guidance for the appropriate support of people with dementia in the current COVID-19 pandemic scenario” [8]. The document was aimed at supporting healthcare professionals and caregivers with some practical information and recommendations to 1) prevent SARS-CoV-2 contagion, 2) limit the risk of mortality and severe infection, and 3) improve patients’ support at home and across the various outpatient, semi-residential, and residential settings. It has already been disseminated to all Italian dementia services and general practitioners. Its contents are being divulgated to a broader audience through supporting materials (e.g., video and infographics) and capillary interactions with patients and caregivers.
In the present study, we explore the awareness and preparedness of dementia caregivers and people with mild cognitive deficits on how they prevent COVID-19 infection and cope with the indirect consequences of the pandemic.
METHODS
Setting and participants
A telephone survey of a sample of patient-caregiver dyads referred to the Center for Cognitive Disturbances and Dementia, Department of Human Neuroscience, Sapienza University of Rome (Italy), was performed. All consecutive patients and caregivers attending our tertiary service in January and February 2020 and participating in a previous phone-based survey on COVID-19 [7] were contacted. The interviews were conducted by the medical staff from November 20, 2020, to December 31, 2020.
During the interview, the main sociodemographic characteristics of caregivers (i.e., age, sex, education, and role) were collected. Patients and caregivers then received practical information and recommendations about four main COVID-19-related issues: 1) adopting safeguard and hygienic measures to prevent SARS-CoV-2 infection; 2) recognizing typical COVID-19 manifestations; 3) recognizing atypical COVID-19 presentations; and 4) recognizing COVID-19 emergency warning signs.
The information and advice provided during the phone call were adapted from the above-mentioned “Interim guidance for the appropriate support of people with dementia in the current COVID-19 pandemic scenario” (summarized in Table 1). Respondents were then asked to rate their level of awareness about the addressed issues and recommendations as “poor”, “moderate”, or “good”. They also had to provide information about their capacity to maintain a stable daily routine, get involved in physically and/or mentally stimulating activities, and provide adequate care to their assisted patients. Their awareness about the recommended directions to follow in suspicion of COVID-19 was also investigated (e.g., when to contact the general practitioner? when to immediately contact the emergency services?). Moreover, they were asked to indicate which sources they consulted to get informed and stay up to date on COVID-19.
Table 1
Information and recommendations provided to survey respondents
| Safeguard and hygienic measures to prevent SARS-CoV-2 infection | ||
| •Wear masks and make sure that others wear masks | ||
| •Wash hands often and make sure that others wash hands | ||
| •Avoid touching eyes, nose, and mouth with unwashed hands | ||
| •Cover mouth and nose with a flexed elbow or tissue when coughing or sneezing | ||
| •Clean and frequently disinfect the house and the touched surfaces | ||
| •Sanitize clothing | ||
| •Ventilate indoor environments | ||
| •Limit home visit by other persons | ||
| •Keep at least one meter away from other people when going out | ||
| •Avoid hugs and handshakes | ||
| •Regularly and gently remind the person with dementia to adhere to these measures | ||
| Recognizing COVID-19 manifestations | ||
| Typical manifestations* | Atypical manifestations* | Emergency warning signs# |
| •Fever or chills | •Agitation, restlessness | •Trouble breathing |
| •Cough | •Confusion | •Chest pain of pressure |
| •Shortness of breath | •Altered consciousness | •Inability to stay awake |
| •Fatigue | •Reduced responsivity | •Bluish lips of the face |
| •Muscle or body aches | •Drowsiness | |
| •Headache | •Worsening of NPS | |
| •Loss of taste and/or smell | •Anorexia | |
| •Nausea and/or vomiting | •Generalized weakness | *It is recommended to promptly contact the GP or other non-emergency services |
| •Diarrhea | •Functional worsening | #It is recommended to immediately contact emergency services |
| •Sore throat | •Falls | |
NPS, neuropsychiatric symptoms.
The interview was carried out by directly asking the caregiver in the case of patients with overt dementia or by involving also the patient experiencing mild cognitive disturbances. However, in this latter case, the answers provided by the patient had to be confirmed and validated by the caregiver to obtain reliable and consistent information.
At the end of the interview, respondents received additional information materials (i.e., videos and infographics) by email or social networks (Supplementary Figure 1).
The following information was abstracted from the clinical charts of patients to characterize their clinical conditions: age; sex; diagnosis; Mini-Mental State Examination score (on the occasion of the last visit); Activities of Daily Living and Instrumental ADL scores (on the occasion of the last visit); disease duration. The diagnosis of MCI and dementia was made by experienced neurologists in accordance with current international diagnostic criteria.
Patients and caregivers (or legal guardians when necessary) had already provided written informed consent for allowing the utilization of the collected data for research purposes (as required by the “Policlinico Umberto I” University Hospital of Rome).
Statistical analysis
The characteristics of patients and caregivers were reported as mean±standard deviation (SD) or as percentages. For statistical analysis, the following scores were assigned to the answers provided by respondents on how to recognize COVID-19 typical manifestations, atypical presentations, and emergency warning signs: “poor” awareness = 1; “moderate” awareness = 2; and “good” awareness = 3. An overall awareness score was then generated by summing up the scores obtained at the three sections of the interview, thus potentially ranging between 3 and 9. The median value of this score was adopted to categorize patient-caregiver dyads into two groups according to their overall awareness (i.e., “Low” versus “High”). Chi-square test (for categorical variables) and Mann-Whitney test (for continuous variables) were performed to compare the characteristics of these two groups. A multivariate logistic regression analysis was finally conducted to identify the variables that were associated with a high versus low level of awareness about COVID-19 (dichotomized dependent variable of interest). The level of statistical significance was set at p < 0.05. All analyses were performed using SPSS version 25 for Mac.
RESULTS
The staff contacted a total of 139 dyads. Five patients were deceased (one with COVID-19), 25 patient-caregiver dyads refused to participate, whereas 109 completed the survey (response rate 78.4%). The sociodemographic and clinical characteristics of patients and caregivers are reported in Table 2. At the time of the survey, almost all the participating dyads lived in the Lazio region where the weekly incidence of COVID-19 amounted to 275.4 cases per 100,000 inhabitants (thus slightly lower than the national figure of 351.7 cases per 100,000 residents) [9]. None of the recruited patients was institutionalized in a nursing home.
Table 2
Characteristics of patient-caregiver dyads participating in the survey according to their overall level of awareness about how to prevent SARS-CoV-2 infection and recognize COVID-19. Data are shown as mean±standard deviations or n (%)
| Overall | Low awareness | High awareness | p | |
| Dyads (n) | 109 | 52 | 57 | |
| Patients | ||||
| Age (y) | 76.8±9.2 | 78.0±8.7 | 75.7±9.5 | 0.15a |
| Sex (women) | 67 (61.5) | 35 (67.3) | 32 (56.1) | 0.25b |
| Diagnosis | 0.46b | |||
| AD | 47 (43.1) | 24 (46.2) | 23 (40.4) | |
| MixDem | 21 (19.3) | 11 (21.2) | 10 (17.5) | |
| VaD | 6 (5.5) | 3 (5.8) | 3 (5.3) | |
| FTD | 2 (1.8) | 0 (0.0) | 2 (3.5) | |
| MCI | 27 (24.8) | 10 (19.2) | 17 (29.8) | |
| Other* | 6 (5.5) | 4 (7.6) | 2 (3.5) | |
| Disease duration (y) | 4.9±3.2 | 5.0±3.4 | 4.8±3.0 | 0.93a |
| MMSE | 20.8±7.9 | 20.3±8.3 | 21.2±7.6 | 0.58a |
| ADL | 4.6±1.8 | 4.7±1.7 | 4.6±1.9 | 0.59a |
| IADL | 4.1±3.1 | 4.0±3.1 | 4.2±3.2 | 0.79a |
| Caregivers | ||||
| Age (y) | 62.3±16.0 | 64.4±18.3 | 60.5±13.7 | 0.27a |
| Sex (women) | 80 (73.4) | 35 (67.3) | 45 (78.9) | 0.20b |
| Education (y) | 13.4±5.3 | 11.6±5.0 | 14.9±5.2 | 0.01a |
| Role | 0.80b | |||
| Spouse | 49 (45.0) | 25 (48.1) | 24 (42.1) | |
| Son/daughter | 51 (46.8) | 22 (42.3) | 29 (50.9) | |
| Other§ | 9 (8.2) | 5 (9.6) | 4 (7.0) | |
| Resources during the pandemic | ||||
| Information on COVID-19 (news media) | 85 (78.0) | 41 (78.8) | 44 (77.2) | 0.84b |
| Stable routine | 95 (87.2) | 46 (88.4) | 49 (86.0) | 0.80b |
| Regular physical activity | 66 (60.6) | 31 (59.6) | 35 (61.4) | 0.85b |
| Regular mental activities | 79 (72.5) | 37 (71.2) | 42 (73.7) | 0.77b |
| COVID-19 awareness score | 5.6±1.0 | 4.8±0.5 | 6.4±0.7 | <0.001a |
aMann-Whitney test; bChi-square test. *Lewy Body dementia (n = 2), Parkinson dementia (n = 2), normal pressure hydrocephalus (n = 2). §Nephew (n = 6), professional caregiver (n = 3). AD, Alzheimer’s disease; ADL, activities of daily living; FTD, frontotemporal dementia; IADL, instrumental activities of daily living; MCI, mild cognitive impairment; MMSE, Mini-Mental State Examination. Low versus High awareness was defined based on the median value of an overall awareness score resulting from the answers provided by respondents on how to recognize COVID-19 typical manifestations, atypical presentations, and emergency warning signs.
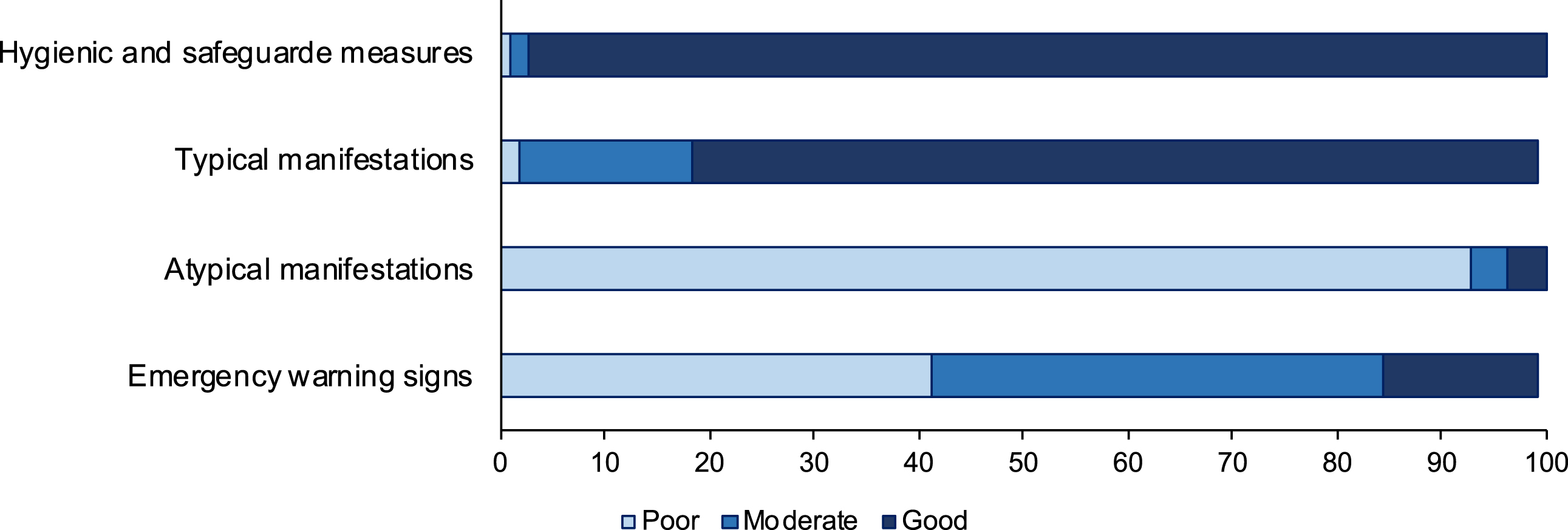
The overwhelming majority of respondents reported having a good level of awareness on the recommended safeguard and hygienic measures to prevent SARS-CoV-2 contagion and a moderate-to-good knowledge of the typical manifestations of COVID-19 (Fig. 1). Conversely, only a minority of them were informed of the atypical presentations of COVID-19 among older people with cognitive impairment, and on how to recognize emergency warning signs (Fig. 1). In most cases, the people interviewed had been able to maintain established routines during the pandemic period. Nearly 60%of patients performed daily physical activity (e.g., walking, light intensity exercises). The majority of patients (72.5%) were also regularly involved in mentally stimulating activities (e.g., reading, listening to music, gardening). Most of the respondents (78.0%) reported having access to updated information on COVID-19 through news media (e.g., television and newspapers) and contacts with relatives. Only a few respondents (i.e., 14.7%) said they were adequately prepared on what to do in the presence of suspected COVID-19. Almost all respondents said they were relieved and encouraged to receive this practical advice.
Fig. 1
Awareness of respondents about how to prevent SARS-CoV-2 infection and recognize COVID-19.
The overall awareness score had a median value of 6 (interquartile range 5-6). No significant differences were found between the dyads with High versus Low awareness concerning the clinical characteristics of patients (Table 2). Conversely, caregivers in the High awareness group exhibited higher mean educational levels relative to the Low awareness group (14.9, SD 5.2 years versus 11.6, SD 5.0 years; p = 0.01) (Table 2). In the multivariate logistic regression analysis, the educational level of the caregiver emerged as the only variable significantly associated with a high awareness of COVID-19 (OR 1.19, 95%CI 1.02–1.31; p = 0.02) (Supplementary Table 1).
DISCUSSION
Increasing people’s knowledge and preparedness on how to prevent COVID-19 and promptly recognize its clinical manifestations is crucial for reducing the impact of the ongoing pandemic. At the same time, it is essential to inform people on how to limit the negative consequences produced by the restrictive measures adopted to deal with the outbreak [10, 11]. The identification of awareness and competence gaps, therefore, represents an essential target of public health research to plan and calibrate effective educational interventions. This objective should be pursued primarily in the most vulnerable groups, such as people with dementia and their families.
Based on the present survey, caregivers of people with dementia and individuals with mild cognitive deficits seem adequately informed on critical measures and behaviors aimed at reducing the risk of SARS-CoV-2 infection and on how to recognize the typical symptoms of COVID-19. The large amount of information disseminated through mass media, institutions [12], associations [13], and healthcare professionals during the pandemic has probably enhanced the preparedness of those who assist these vulnerable people. Moreover, it is encouraging that patients and caregivers had often been able to build and maintain a daily routine and keep active, updated, and purposeful, notwithstanding the restrictive measures. This is fundamental to mitigate the feelings of loneliness and isolation imposed by the pandemic, tackle the observed clinical worsening of patients, and ease the caregiver’s burden.
On the contrary, it appears imperative to inform caregivers of the possibility that COVID-19 may manifest with atypical signs and symptoms in people with dementia. The high lethality of COVID-19 in this population has been partly attributed to the late recognition of these misleading presentations, mainly consisting of delirium or exacerbations of pre-existing neuropsychiatric disorders. In particular, both hypoactive and hyperactive delirium have been frequently observed among older people with COVID-19 and have been associated with higher mortality [14–16]. Nevertheless, this clinical manifestation of COVID-19 is still poorly recognized (especially in non-experts) as compared with other peculiar onsets of the disease (e.g., hyposmia and hypogeusia) [17]. In parallel, clear messages about what to do in the suspicion of COVID-19 should be conveyed to these people, especially to those with a low educational level and health literacy. For instance, many of them still do not know when it is appropriate to contact the general practitioner or when to go directly to the emergency department. At the COVID-19 outbreak in Italy, the inadequate preparedness has likely prompted many people with mild symptoms to rush to the hospital, contributing to a rapid saturation of available resources. The ability of caregivers to access, understand, and use information and services to participate in health-related decisions (i.e., health literacy) is fundamental for the provision of care and support to older people. Previous studies had already shown that low education is adversely associated with the health literacy of caregivers of adult care recipients, thus potentially increasing the risk for poorer management and health outcomes [18, 19].
This study has some limitations to be acknowledged, namely the limited sample size, the monocentric design, and the essential reliance on the perceptions of respondents rather than on objective measures. Moreover, the degree of agreement between patients and caregivers when self-evaluating their competence about COVID-19 was not measured and deserves to be specifically assessed in future studies.
In conclusion, filling the knowledge gaps on COVID-19 in (or around) the most vulnerable people, like those living with dementia, through sustainable and targeted interventions, may represent a significant resource to tackle the pandemic and limit its consequences.
ACKNOWLEDGMENTS
We thank Pietro Maiozzi for the realization of Supplementary Figure 1.
Authors’ disclosures available online (https://www.j-alz.com/manuscript-disclosures/21-0264r2).
SUPPLEMENTARY MATERIAL
[1] The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/JAD-210264.
REFERENCES
[1] | Liu N , Sun J , Wang X , Zhao M , Huang Q , Li H ((2020) ) The impact of dementia on the clinical outcome of COVID-19: A systematic review and meta-analysis. J Alzheimers Dis 78: , 1775–1782. |
[2] | Suàrez-González A , Livingston G , Low LF , Cahill S , Hennelly N , Dawson WD , Weidner W , Bocchetta M , Ferri CP , Matias-Guiu JA , Alladi S , Musyimi CW , Comas-Herrera A (2020) Impact and mortality of COVID-19 on people living with dementia: Cross-country report – Resources to support community and institutional Long-Term Care responses to COVID-19. https://ltccovid.org/2020/08/19/impact-and-mortality-of-covid-19-on-people-living-with-dementia-cross-country-report/ |
[3] | Zuin M , Guasti P , Roncon L , Cervellati C , Zuliani G ((2021) ) Dementia and the risk of death in elderly patients with COVID-19 infection: Systematic review and meta-analysis. Int J Geriatr Psychiatry 36: , 697–703. |
[4] | Canevelli M , Palmieri L , Raparelli V , Lo Noce C , Colaizzo E , Tiple D , Vaianella L , Vanacore N , Brusaferro S , Onder G , Palmieri L , Bertinato L , Brambilla G , Calcagnini G , Censi F , Donfrancesco C , Facchiano F , Floridia M , Giuliano M , Grisetti T , Kodra Y , Langer M , Lega I , Albedi FM , Manno V , Mattei E , Meli P , Minelli G , Nebuloni M , Nisticò L , Nonis M , Palmisano L , Petrosillo N , Pricci F , Punzo O , Salerno P , DeBella MT , Taruscio D , Unim B , Vichi M , Villani ER , Zona A ((2020) ) Prevalence and clinical correlates of dementia among COVID-19-related deaths in Italy. Alzheimers Dement (Amst) 12: , e12114. |
[5] | Mok VCT , Pendlebury S , Wong A , Alladi S , Au L , Bath PM , Biessels GJ , Chen C , Cordonnier C , Dichgans M , Dominguez J , Gorelick PB , Kim SY , Kwok T , Greenberg SM , Jia J , Kalaria R , Kivipelto M , Naegandran K , Lam LCW , Lam BYK , Lee ATC , Markus HS , O’Brien J , Pai MC , Pantoni L , Sachdev P , Skoog I , Smith EE , Srikanth V , Suh GH , Wardlaw J , Ko H , Black SE , Scheltens P ((2020) ) Tackling challenges in care of Alzheimer’s disease and other dementias amid the COVID-19 pandemic, now and in the future. Alzheimers Dement 16: , 1571–1581. |
[6] | Cagnin A , Di Lorenzo R , Marra C , Bonanni L , Cupidi C , Laganà V , Rubino E , Vacca A , Provero P , Isella V , Vanacore N , Agosta F , Appollonio I , Caffarra P , Pettenuzzo I , Sambati R , Quaranta D , Guglielmi V , Logroscino G , Filippi M , Tedeschi G , Ferrarese C , Rainero I , Bruni AC , Gallo E , Grassini A , Marcinnò A , Roveta F , De Martino P , Frangipane F , Puccio G , Colao R , Mirabelli M , Martellacci N , Lino F , Mozzetta S , Bussè C , Camporese G , Sacco S , Lechiara MC , Carrarini C , Russo M , Casalena A , Sucapane P , Tiraboschi P , Caroppo P , Redaelli V , Di Fede G , Coppa D , Peluso L , Insarda P , De Bartolo M , Esposito S , Iavarone A , Orsini AVM , Salvatore E , Criscuolo C , Sambati L , Santoro R , Gragnaniello D , Pedriali I , Ludovico L , Chiari A , Fabbo A , Bevilacqua P , Galli C , Magarelli S , Perini M , Spalletta G , Banaj N , Porcari DE , Caruso G , Porcari DE , Cipollini V , Casini AR , Ursini F , Bruno G , Rozzini R , Brambilla M , Magnani G , Caso F , Spinelli EG , Ramusino MC , Perini G , Luzzi S , Cacchiò G , Angeloni R , Giuli C , Fabi K , Guidi M , Paci C , Castellano A , Carapelle E , Petrucci R , Accogli M , Calabrese G , Trevisi GN , Coluccia B , Giuliano AV , Caggiula M , Da Re F , Milia A , Pilia G , Mascia MG , Putzu V , Piccoli T , Cuffaro L , Monastero R , Battaglia A , Blandino V , Lupo F , Cumbo E , Antonina L , Caravaglios G , Vezzosi A , Bessi V , Tognoni G , Calsolaro V , Mossello E , Amici S , Trequattrini A , Pezzuto S , Mecocci P , Fichera G , Pradelli S , Formilan M , Coin A , Detogni L , Sala F , Sandri G , Gallucci M , Mazzarolo AP , Bergamelli C ((2020) ) Behavioral and psychological effects of coronavirus disease-19 quarantine in patients with dementia. Front Psychiatry 11: , 578015. |
[7] | Canevelli M , Valletta M , Toccaceli Blasi M , Remoli G , Sarti G , Nuti F , Sciancalepore F , Ruberti E , Cesari M , Bruno G ((2020) ) Facing dementia during the COVID-19 outbreak. . J Am Geriatr Soc 68: , 1673–1676. |
[8] | Tavolo per il monitoraggio e implementazione del Piano Nazionale delle Demenze (2020) Indicazioni ad interim per un appropriato sostegno alle persone con demenza nell’attuale scenario della pandemia di COVID-19. https://www.iss.it/documents/20126/0/Rapporto+ISS+COVID-19+61_2020.pdf/c2f4f7b5-68e9-849b-0071-f36d4560d83f?t=1603878366209. Accessed on October 23, 2020. |
[9] | Task force COVID-19 del Dipartimento Malattie Infettive e Servizio di Informatica, Istituto Superiore di Sanità (2020) Epidemia COVID-19 https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_23-aprile-2020.pdf. Accessed on November 18, 2020. |
[10] | Parsons J , Waters DL , Binns E , Burholt V , Cheung G , Clare S , Duncan R , Fox C , Gibson R , Grant A , Guy G , Jackson T , Kerse N , Logan R , Peri K , Petagna C , Stephens F , Taylor D , Teh R , Wall C ((2021) ) Letter to the Editor: Healthy for life: An innovative and collaborative approach to COVID 19 lockdown in New Zealand. J Frailty Aging 10: , 72. |
[11] | Boreskie KF , Hay JL , Duhamel TA ((2020) ) Preventing frailty progression during the COVID-19 pandemic. . J Frailty Aging 9: , 130–131. |
[12] | CDC (2020) Caring for People Living with Dementia in Community Settings https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/caregivers-dementia.html. Accessed on February 7, 2021. |
[13] | Alzheimer Europe (2020) COVID-19 - Living with dementia. https://www.alzheimer-europe.org/Living-with-dementia/COVID-19. Accessed on February 7, 2021. |
[14] | Poloni TE , Carlos AF , Cairati M , Cutaia C , Medici V , Marelli E , Ferrari D , Galli A , Bognetti P , Davin A , Cirrincione A , Ceretti A , Cereda C , Ceroni M , Tronconi L , Vitali S , Guaita A ((2020) ) Prevalence and prognostic value of Delirium as the initial presentation of COVID-19 in the elderly with dementia: An Italian retrospective study. EClinicalMedicine 26: , 100490. |
[15] | Mendes A , Herrmann FR , Périvier S , Gold G , Graf CE , Zekry D (2021) Delirium in older patients with COVID-19: Prevalence, risk factors, and clinical relevance. J Gerontol A Biol Sci Med Sci, doi: 10.1093/gerona/glab039. |
[16] | Pun BT , Badenes R , Heras La Calle G , Orun OM , Chen W , Raman R , Simpson BGK , Wilson-Linville S , Hinojal Olmedillo B , Vallejo de la Cueva A , et al. ((2021) ) Prevalence and risk factors for delirium in critically ill patients with COVID-19 (COVID-D): A multicentre cohort study. Lancet Respir Med 9: , 239–250. |
[17] | Pierron D , Pereda-Loth V , Mantel M , Moranges M , Bignon E , Alva O , Kabous J , Heiske M , Pacalon J , David R , Dinnella C , Spinelli S , Monteleone E , Farruggia MC , Cooper KW , Sell EA , Thomas-Danguin T , Bakke AJ , Parma V , Hayes JE , Letellier T , Ferdenzi C , Golebiowski J , Bensafi M ((2020) ) Smell and taste changes are early indicators of the COVID-19 pandemic and political decision effectiveness. Nat Commun 11: , 5152. |
[18] | Bennett IM , Chen J , Soroui JS , White S ((2009) ) The contribution of health literacy to disparities in self-rated health status and preventive health behaviors in older adults. Ann Fam Med 7: , 204–211. |
[19] | Yuen EYN , Knight T , Ricciardelli LA , Burney S ((2018) ) Health literacy of caregivers of adult care recipients: A systematic scoping review. Heal Soc Care Community 26: , e191–e206. |



