Abstract
Introduction
We have experienced a pandemic induced by the interaction of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) structural proteins with innate structures. These interactions are especially prevalent for patients with underlying pathologies, such as cardiovascular diseases. However, there has been limited work to uncover the range of responses induced by SARS-CoV-2 structural proteins. Thus, our objective was to investigate how endothelial cell pro-thrombotic and pro-inflammatory responses are altered after exposure to SARS-CoV-2 spike, nucleocapsid, and membrane-envelope proteins. We hypothesized that after a short duration exposure, endothelial cells would have a heightened thrombotic and inflammatory potential. With longer exposures, this may lead to altered disease progression and the observed increased mortality and morbidity rates in patients with underlying vascular pathologies.
Methods
To test this hypothesis, human endothelial cells were exposed to SARS-CoV-2 structural proteins. After the exposure, the expression of thrombomodulin, PECAM-1, connexin-43, and gC1qR were assessed. In parallel, standard cell culture readouts were assessed to determine if these incubations altered cell growth and metabolism.
Results and Conclusions
We observed significant increases in thrombotic and inflammatory marker expression, with no change to the cell culture parameters (with the exception of a reduction in cell density in response to one SARS-CoV-2 structural protein). Importantly, these observations were dependent on the viral structural protein the cells were exposed to, suggesting that the interactions of SARS-CoV-2 with innate cells is complex and must be uncovered. Combined, this suggests that SARS-CoV-2 structural proteins can regulate inflammatory and thrombotic responses that underlie common pathologies observed during COVID-19.
Similar content being viewed by others
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a novel coronavirus, responsible for the worldwide pandemic and has been shown to target multiple organs resulting in a cytokine storm and altered thrombosis.39,46 Enhancements of the inflammatory and thrombotic systems can lead to significant pathologies, especially for those patients who present with underlying medical conditions. Reports have documented that patients with pre-existing and/or underlying vascular pathologies have significantly higher mortality and morbidity rates as compared to patients without these pathologies.47 However, even with these significant observations, there has been limited work aimed to elucidate the underlying biological responses that can lead to enhancements of the inflammatory and thrombotic systems. Thus, the major goal of this work was to begin to uncover vascular cell responses that may be responsible for the observed increase in inflammatory and thrombotic responses during SARS-CoV-2 infection.
SARS-CoV-2, and other SARS-CoVs, can be characterized by the structural proteins that present on the intact virus. These structural proteins are responsible for effective and stable viral transmission by ensuring a formed viral capsid and interacting with host proteins. Four structural proteins have been characterized for the SARS-CoVs: namely, the Spike (S) Protein, Nucleocapsid (N) Protein, the Membrane Protein and the Envelope Protein.32 S-protein has been observed to interact with the ACE2 receptor.43 N-protein interferes with NF-κB signaling and can alter the production of interferons.26 Finally, a fusion of the Membrane and Envelope Proteins (termed M-protein) reduces inflammasome activity.52 Each of these examples illustrates the ability of distinct SARS-CoV-2 structural proteins to independently alter host inflammatory reactions. Viral proteins have also been shown to interact with the innate immune system through gC1qR (the receptor for the globular head of C1q),10,19,45 which is ubiquitously expressed. We have recently shown that SARS-CoV-2 structural proteins can interact with gC1qR expressed on fibroblasts during altered inflammatory and thrombotic responses.11 Further, due to the identified role of gC1qR on regulating inflammatory and thrombotic responses observed during vascular pathologies, we chose to investigate how SARS-CoV-2 structural proteins interact with endothelial cell gC1qR.14,15,35,36
Endothelial cells participate in many inflammatory and thrombotic processes in vivo, which relate to cardiovascular disease pathogenesis. Further, vascular pathologies have been correlated with increased mortality and morbidity rates in patients that present with COVID-19.3,17 gC1qR has been shown to link inflammatory reactions to thrombotic reactions by having binding sites for complement component C1q and high-molecular weight kininogen (HK).21 The interactions of C1q with gC1qR instigates many innate immune reactions, including promoting the progression/completion of the classical complement cascade, oxidative stress production and production of cytokines.5,41,51 Enhanced HK activity, associated with HK docking to receptors, is linked to increased bradykinin activity and the activation of Factor XII, C3 and C5.8,24 Therefore, enhanced vascular inflammatory and thrombotic responses, which are observed during vascular disease progression, can possibly be linked to alterations in gC1qR activity. Since a wide range of viral structural proteins can alter gC1qR function, it is possible that many of the vascular pathologies observed during COVID-19 are regulated by changes to gC1qR signaling.
In order to extend the role of gC1qR in vascular pathologies, we chose to monitor the expression of endothelial cell thrombomodulin, PECAM-1, connexin 43 and gC1qR after exposure to SARS-CoV-2 structural proteins. Thrombomodulin can interact with thrombin to activate Protein C or inhibit thrombin-activatable fibrinolysis inhibitor and thrombomodulin can also alter the activity of C3b.48 Thus, thrombomodulin has roles within inflammation and thrombosis. PECAM-1 is an adhesion molecule that plays a role in inflammation and angiogenesis.49 Connexin 43 is a gap junction protein that allows for endothelial cells to communicate along the blood vessel wall with neighboring endothelial cells and has been shown to play a role in angiogenesis and vascular disease progression.12,28 As described above, gC1qR has a role in innate immunity and thrombosis.
In the present study, we chose to investigate if specific SARS-CoV-2 structural proteins can alter endothelial cell inflammatory and thrombotic functions that have been associated with vascular disease progression. These alterations may provide insight into the mechanisms by which patients with COVID-19 and underlying vascular complications have higher mortality and morbidity rates as compared with patients without underlying complications. We hypothesized that a short duration exposure (1 h) to SARS-CoV-2 structural proteins would initiate endothelial cell pro-inflammatory and pro-thrombotic reactions as compared with endothelial cells not exposed to SARS-CoV-2 proteins. Additionally, by characterizing the vascular response, we may be able to identify new markers for disease progression potentially for the development of targeted therapy.
Materials and Methods
Endothelial Cell Culture
Human umbilical vein endothelial cells (HUVECs) were purchased from ScienCell Research Laboratories (Carlsbad, CA) and maintained in endothelial cell medium, supplemented with 5% fetal bovine serum, antibiotics (penicillin/streptomycin), and growth supplement (as suggested by the manufacturer) at 37°C and 5% CO2. HUVECs were cultured on tissue culture plastic flasks and well-plates during the entire experimental time course. Passage of cells was accomplished via a trypsin digestion (for no more than 3 min) once the cultured cells reached a confluence of greater than 90%. For experimental conditions, HUVECs were incubated with SARS-CoV-2 structural proteins (S-protein, N-Protein or the fusion of the membrane and envelope proteins denoted as M-protein) at a final concentration of 3 μg mL−1 for 1 h (Virogen, Watertown, MA, purchased as recombinant proteins produced in E. coli). Note that initial dose response curves were obtained in response to SARS-CoV-2 structural proteins incubation. The EC50 for each protein was approximately 3μg mL−1 (range 2–5 μg mL−1). All daily experimental conditions included internal negative controls consisting of HUVECs incubated in normal cell media in the absence of SARS-CoV-2 structural proteins for 1 h. Note that initial experiments to elucidate the time effects of SARS-CoV-2 structural protein exposure on HUVECs were conducted using the same methods described herein, with the exception that the exposure duration varied between either 5 min, 1 h or 24 h (each of these experiments had its own internal negative control, as above). For statistical purposes, the initial seeding density for all experiments was maintained at approximately 95% confluence and cells were allowed to adhere to new plates for approximately 18 h prior to the addition of structural proteins. HUVECs were used between passage 2-5, defined at each passage of at least a doubling of cell area but no more than a tripling of cell area.
HUVEC Viability, Density and Metabolic Activity
We evaluated endothelial cell viability, density and metabolic activity after exposure to SARS-CoV-2 structural proteins to determine whether these conditions alter endothelial cell growth during the culture conditions. Further, when significant changes are observed, all data is normalized to this alteration. To quantify cell viability and density, a standard live/dead cell cytotoxicity assay is employed. The cytotoxicity assay consists of 2μM calcein and 4μM ethidium (ThermoFisher Scientific), as previously described by us.1 Briefly, after the particular exposure conditions, endothelial cells are washed twice with warmed PBS (37°C) and immediately incubated with approximately 50μL of the cytotoxicity assay for no more than 5 min (at 37°C). After this incubation, cells are imaged on an inverted microscope (Nikon TE-2000U). Each independent condition is imaged at 3 randomized locations within each culture well and this data is then averaged for a single data point.1,40 A minimum of 3 averaged data points are summarized and reported for each condition (note that all sample size numbers are reported in the figure captions). Cell viability and density are calculated directly from the recorded images. Cell viability is defined as the number of live cells divided by the total number of cells per imaging area.40 Cell density is defined as the total number of live cells per imaging area.40 The imaging area has been calibrated for each objective-camera pair. Cell density can be further normalized to the seeding density to provide us with information regarding the proliferation during the timed exposure conditions.
To quantify the metabolic activity of endothelial cells after exposure to SARS-CoV-2 structural proteins, we made use of a 3-[4,5-dimethylthiazol-2-yl]−2,5-diphenyl tetrazolium bromide (MTT) assay42, which quantifies the activity of mitochondrial dehydrogenase (note that all MTT reagents were purchased from Millipore Sigma, St. Louis, MO). HUVECs were washed with warm PBS (pH 7.4, 37°C) and then immediately incubated with MTT reagent reconstituted in basal HUVEC media for approximately 2-3 h. Formazan crystals were dissolved in 10% Triton-X and 0.1 M HCl in anhydrous isopropanol. The ensuing solution was gently mixed on an orbital shaker for 10-15 min. The absorbance of the solution resulting from the dissolving procedures was quantified at 690 nm. Duplicate 100μL samples were collected from each independent condition sample and transferred to a 96 well plate for absorbance measurements. All data was normalized to the metabolic activity of paired cells incubated without SARS-CoV-2 structural proteins.
HUVEC gC1qR Expression
The surface expression of HUVEC gC1qR was quantified after exposure to SARS-CoV-2 structural proteins using a solid-phase ELISA approach. Cells were washed (2x with warm PBS, 37°C, pH 7.4) and then immediately neutralized with 100mM glycine – 0.1% BSA (30 min, 37°C). To assess the ability for SARS-CoV-2 structural proteins to mitigate the activity of specific functional domains of gC1qR, we made use of 2 monoclonal antibodies that target either the C1q binding region of gC1qR (60.11 epitope) or the HK binding region on gC1qR (83.13 epitope).13,35 Primary antibodies were incubated with endothelial cells for 1 h at a final concentration of 1 μg mL−1. After this incubation period, cells were washed two times with PBS. An appropriate alkaline phosphatase conjugated secondary antibody was used to detect primary antibody binding. Secondary antibodies (Millipore Sigma) were incubated with cells for 1 h at a final concentration of 1 μg mL−1. Color development was achieved by addition of pNPP and the absorbance was read spectrophotometrically at 405nm. Note that all appropriate positive and negative controls were included within each independent experiment as described by us.41
HUVEC Thrombotic and Inflammatory Mediator Expression
The surface expression of HUVEC thrombomodulin, PECAM-1 and connexin 43 was quantified after the exposure to SARS-CoV-2 structural proteins using a solid-phase ELISA approach. Similar to the methods described for the assessment of gC1qR expression, after the exposure conditions, HUVECS were washed, fixed and neutralized. These procedures were followed by a 1 h incubation with specific monoclonal antibodies towards the specific inflammatory or thrombotic marker (thrombomodulin antibody was purchased from Biolegend (San Diego, CA); PECAM-1 antibody was purchased from Ancell Corporation (Stillwater, MN); connexin-43 antibody was purchased from Abcam Inc. (Cambridge, MA)). Primary antibodies were incubated with cells at the following final concentrations: thrombomodulin, 1 μg mL−1; PECAM-1, 1 μg mL−1 and Connexin-43, 1 μg mL−1. As above, detection of primary antibodies was accomplished via an appropriate alkaline phosphatase secondary antibody (Millipore Sigma) at a final concentration of 1 μg mL−1 for 1 h. Color development was achieved by the addition of pNPP and absorbance was read spectrophotometrically at 405nm.
Statistics
All statistical procedures were carried out in SAS (v. 9.4, SAS Institute, Cary, NC) using a one-way ANOVA, with the only factor being the exposure conditions (e.g. SARS-CoV-2 structural protein). We made use of the Duncan post-hoc test to assess which, if any, conditions were significantly different. All viability, density and metabolic activity data was normalized as described above and reported as such. ELISA data from independent experiments was normalized to the HUVEC control samples (e.g. cells incubated in the absence of SARS-CoV-2 structural proteins in a pairwise manner), with background subtraction (e.g. cells incubated in the absence of the primary antibody), as appropriate, using the following formula:
where \(OD\) is the averaged optical density from paired wells, ‘Sample’ represents each of our experimental conditions, ‘Negative Control’ represents the samples incubated in the absence of SARS-CoV-2 structural proteins and ‘Background’ represents the samples obtained in the absence of the primary antibody for the specific condition. When there were multiple dependent wells, this data was first averaged to obtain a single independent data point for the particular exposure condition. Normalized data from at least 3 independent experiments are shown and used for statistical analysis (all sample size numbers are reported in the Figure legends). Note that all experiments were compared to a ‘Negative Control,’ which was cells incubated for the appropriate duration in standard cell culture media. As reported in the figure legends, this data would have a value of ‘1’ on plots and is not shown for ease of viewing the structural protein data. Since there were no statistical differences in the observed metabolic activity of cells after 1 h of exposure to SARS-CoV-2 structural proteins, we did not normalize ELISA data by cell growth characteristics.
Results
Effects of Exposure Duration on HUVEC Responses
In order to determine (1) an appropriate exposure duration of SARS-CoV-2 structural proteins and (2) whether or not there is a time-dependent effect on response HUVEC response variables to SARS-CoV-2 structural proteins, we exposed HUVECs to SARS-CoV-2 structural proteins for 5 min, 1 h or 24 h. After these exposure durations, cell density and the exposure of PECAM-1, thrombomodulin and connexin-43 was investigated. Cell density (Table 1) was observed to decrease significantly as the exposure duration to SARS-CoV-2 structural proteins increased. Due to these changes, the expression of PECAM-1, thrombomodulin and connexin-43 were normalized by the relative change in cell density (not shown). We observed that in general, there was a small increase in response variable expression after a 5 min exposure to SARS-CoV-2 structural proteins, which was further increased after 1 h exposure, as compared with the negative control. After 24 h, the expression of these proteins was further increased or remained the same, as compared with the 1 h time point (not shown). However, due to the significant drop in cell density at 24 h and the relatively consistent expression data between 1 and 24 h experiments, we chose to conduct all future experiments with a 1 h exposure duration.
HUVEC Viability, Density and Metabolic Activity
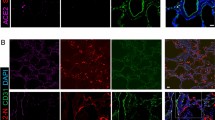
In order to determine whether or not a short-duration exposure (1 h) to SARS-CoV-2 structural proteins alters the growth characteristics of endothelial cells, we quantified cell viability and cell density at the end of the exposure conditions. There were no statistical differences in cell viability, which is a measure of the ability for the experimental conditions to cause cell apoptosis, after a 1 h exposure to SARS-CoV-2 structural proteins (Fig. 1a). In parallel, we quantified cell density, which is a measure of the ability to alter cell growth. While there were decreases in cell density after exposure to SARS-CoV-2 structural protein, it was only statistically significant for the exposure to N-protein (P < 0.05, Fig. 1b) as compared with cells incubated in the absence of SARS-CoV-2 structural proteins. To confirm that the exposure to SARS-CoV-2 structural proteins did not alter the metabolic activity of endothelial cells, we used a standard MTT assay to quantify the activity of mitochondrial dehydrogenase. After a 1 h exposure to SARS-CoV-2 structural proteins, there was no significant changes in the metabolic activity of endothelial cells (Fig. 1c). Since all of our standard cell culture monitoring experiments illustrated that there were no changes in cell viability and metabolic activity and only small reductions in cell density after a 1 h exposure to SARS-CoV-2 structural proteins, there was no need to further normalize our data based on growth characteristics.
Human umbilical vein endothelial cell viability (a), density (b) and metabolic activity (c) after a short duration exposure (1 h) to SARS-CoV-2 structural proteins; spike (S), nucleocapsid (N) protein and membrane-envelope (M) protein. All data are reported as the mean + standard error of the mean for 3 independent (viability and density) or 6 independent experiments (MTT). Viability (a) and metabolic activity (c) are normalized to our negative control, which would have a value of ‘1’ on these plots. *Significantly different than negative control (ANOVA, Duncan method, P < 0.05).
HUVEC gC1qR Expression
In order to determine whether or not a short duration exposure (1 h) to SARS-CoV-2 structural proteins can interact with innate inflammatory responses, we observed the expression of gC1qR on endothelial cell membranes (Fig. 2). In order to relate our measurements to possible functional responses, we made use of two different gC1qR antibodies, one that detects the C1q binding site of gC1qR (Fig. 2a) and the other that detects the HK binding site of gC1qR (Fig. 2b). The ability for the C1q binding site antibody to associate with gC1qR after a 1 h exposure to any SARS-CoV-2 structural protein was significantly reduced as compared with the negative control (ANOVA, P < 0.05). Further, there were no statistical differences observed between the different SARS-CoV-2 structural proteins. In regards to the gC1qR HK binding site, a short duration exposure to SARS-CoV-2 structural proteins significantly increased the antibody association with this site as compared with the negative control (AOVA, P < 0.05). Interestingly, the exposure to N-protein significantly increased the expression of the HK binding site as compared with the exposure to M-protein (ANOVA, P < 0.05)
Human umbilical vein endothelial cell gC1qR surface expression after a short duration exposure to SARS-CoV-2 structural proteins; spike (S), nucleocapsid (N) protein and membrane-envelope (M) protein. We observed different protein locations that are associated with different structural and functional locations of gC1qR: including 60.11 (a, the C1q globular head binding domain) and 83.13 (b, the HK binding domain). All data are reported as the mean + standard error of the mean for a minimum of 3 independent experiments (range 3–8), normalized to our negative control which would have a value of ‘1’ on all plots. *Significantly different than negative control (ANOVA, Duncan method, P < 0.05), + significantly different than marked structural protein (ANOVA, Duncan method, P < 0.05).
HUVEC Inflammatory and Thrombotic State
To determine whether or not a short duration exposure (1 h) to SARS-CoV-2 structural proteins can alter the inflammatory and thrombotic state of endothelial cells, we observed the surface expression of thrombomodulin, PECAM-1 and connexin-43 (Fig. 3). Thrombomodulin, which has pro-thrombotic, anti-thrombotic and inflammatory functions was observed to be significantly up-regulated after exposure to S-protein and N-protein, but not M-protein as compared with the negative control conditions (ANOVA, P < 0.05, Fig. 3a). The expression of thrombomodulin, however, was independent of SARS-CoV-2 structural protein exposure. PECAM-1 up-regulation is considered to be pro-inflammatory and after a 1 h exposure to SARS-CoV-2 structural proteins, we observed an increase in PECAM-1 expression in response to S-protein and N-protein, but not M-protein as compared to the negative control conditions (ANOVA, P < 0.05, Fig. 3b). Further, the exposure to S-protein and N-protein increased the expression of PECAM-1 significantly as compared with M-protein (ANOVA, P < 0.05). Finally, the expression of connexin 43, which plays a significant role in many endothelial cell functions related to inflammation and thrombosis, was significantly enhanced after exposure to S-protein and M-protein but not N-protein, as compared with the negative control conditions (ANOVA, P < 0.05, Fig. 3c). The exposure of connexin 43 after the exposure to S-protein was also enhanced as compared with N-protein (ANOVA, P < 0.05).
Human umbilical vein endothelial cell thrombomodulin (a), PECAM-1 (b) and connexin 43 (c) surface expression after a short duration exposure (1 h) to SARS-CoV-2 structural proteins; spike (S) protein, nucleocapsid (N) protein and membrane-envelope (M) protein. All data are reported as the mean + standard error of the mean for a minimum of 3 independent experiments (range 3–5 for thrombomodulin, 4–8 for PECAM-1 and 6–10 for connexin 43), normalized to our negative control which would have a value of ‘1’ on all plots. *Significantly different than negative control (ANOVA, Duncan method, P < 0.05), + significantly different than marked structural protein (ANOVA, Duncan method, P < 0.05).
Discussion
Effects of Exposure Duration on HUVEC Responses
To determine an appropriate exposure duration and whether or not the exposure to SARS-CoV-2 structural proteins was time dependent, we observed a sub-set of response variables (PECAM-1, thrombomodulin and connexin-43 expression) after a 5 min, 1 h or 24 h exposure duration (Table 1, reports density). Our data illustrates that there was a significant drop in cell density after a 24 h exposure and that there were minimal changes in the expression of the response variables measured after 24 h as compared with the 1 h time point. While there are no reports that we can directly compare with, these findings directed us to choose a 1 h exposure duration for all future experiments.
HUVEC Viability, Density and Metabolic Activity
Cell viability and cell density provide measures of the ability of the experimental conditions to alter the general culture conditions, by either accelerating or impairing cell growth and/or apoptosis. Our data suggests that a short duration exposure, for 1 h, to SARS-CoV-2 structural proteins does not alter cell viability (Fig. 1a) and only the exposure to N-protein altered cell density (Fig. 1b), as compared with cells that were not exposed to SARS-CoV-2 structural proteins. While there are no studies that we can directly compare with, previous work has shown that endothelial cells (HUVECs) are 99% viable after a 5 day exposure to Hanta virus.37 Similarly, after 10 days of exposure to Zika virus, brain endothelial cells (hCMECs) did not show a reduction in cell viability.34 After a 6 day exposure to the Coxsackie virus, HUVECs did not respond with a change in their cell density, morphology or any other culture parameters investigated.6 Overall, our data is generally in agreement with these prior reports and illustrates that a short duration exposure to SARS-CoV-2 structural proteins does not impair endothelial cell viability and density (with the exception of N-protein). It is possible that with a longer duration exposure to N-protein, HUVEC cell density would approach the density observed in our control conditions, agreeing with previous work. Also, it is important to note that in vivo, endothelial cells would not be exposed to a single purified structural protein and thus, the slight reduction in cell density observed here may not be representative of viral infection pathways.
We quantified the metabolic activity of endothelial cells after short duration exposure to SARS-CoV-2 structural proteins to further quantify whether or not these exposure conditions altered the growth of cells. Our data suggests that a 1 h exposure to SARS-CoV-2 structural proteins does not alter the metabolic activity of endothelial cells (Fig. 1c). While there are no studies that can directly be compared with, others have shown that short exposures to various viruses (including the Zika virus and mouse hepatitis virus type 3) do not alter endothelial cell metabolic activity as quantified by the MTT and MTS assays.4,44 However, with long-term exposures (greater than 48 h), alterations to endothelial cell metabolic activity have been observed after exposure to various viruses and this long-term inhibition of mitochondrial metabolism has been suggested as a mechanism that can lead to endothelial dysfunction, cytokine storms and altered thrombosis observed during viral infections.4,9,50 Overall our data suggests that impairment of endothelial cell growth characteristics and metabolic activity is a function of the duration of exposure. With shorter duration exposures, there is a limited viral induced effect that becomes magnified as the exposure duration increases.
HUVEC gC1qR Expression
The expression of gC1qR, a ubiquitous molecule that plays a central role in regulating innate immune reactions and thrombotic reactions, was assessed with two monoclonal antibodies after a short duration (1 h) exposure to SARS-CoV-2 structural proteins. These antibodies target different functional and structural domains within gC1qR, thus providing us with the ability to assess alterations to innate immune functions independent of thrombotic functions. Our data illustrate that the ability of our antibodies to detect the C1q binding site was reduced after exposure to SARS-CoV-2 structural proteins, with no statistical significance observed between the three structural proteins investigated (Fig. 2a). Moreover, the data show that the individual structural proteins are interacting with gC1qR, at the C1q binding site, preventing the antibody from associating with gC1qR. This conclusion is in agreement with previous work illustrating that viral exposures (including circovirus, HIV, HCV and adenovirus core proteins) can bind to and inhibit responses from gC1qR.10,25,31,33 Further, previous work from our lab has illustrated that SARS-CoV-2 structural proteins can interact directly with purified gC1qR (manuscript under review) and with adventitial fibroblast gC1qR11 (in cell culture) and that under both of these experimental conditions downstream inflammatory and thrombotic responses were enhanced.
We also examined the ability of a short duration exposure (1 h) to SARS-CoV-2 structural proteins to modulate the expression of the HK binding site of gC1qR. Our data illustrate that all of the structural proteins investigated can increase the detection of the gC1qR HK binding site (Fig. 2b). Further, there were significant differences observed between HK binding site detection after exposure to N-protein as compared with M-protein. gC1qR-HK association is currently thought to be the primary link between innate immune reaction activity and thrombotic activity, principally through the regulation of bradykinin production and signaling, and Factor XII association downstream of HK binding to gC1qR.14,15,16 We have observed an increase in HK binding to purified gC1qR after exposure to SARS-CoV-2 structural proteins (manuscript under review). Furthermore, Factor XII binding was also increased after exposure to SARS-CoV-2 structural proteins, which in turn may lead to enhanced bradykinin production (manuscript under review). Finally, adventitial fibroblast gC1qR HK binding site expression was enhanced after exposure to SARS-CoV-2 structural proteins.11Therefore, our data is in agreement with previous findings and suggests a link between enhanced inflammation and thrombosis during viral infections. Importantly, COVID-19 patients have been observed to have high incidences of cardiovascular complications, and those patients with underlying vascular complications have higher mortality and morbidity rates as compared with patients without underlying vascular conditions.30
HUVEC Inflammatory and Thrombotic State
In order to determine whether or not a short-duration exposure (1 h) to SARS-CoV-2 structural proteins can alter the expression of endothelial cell inflammatory and thrombotic markers, we monitored the expression of thrombomodulin, PECAM-1 and Connexin 43 (Fig. 3). Thrombomodulin has both pro-thrombotic and anti-thrombotic functions and has been associated with inflammatory functions. We observed that exposure to S-protein and N-protein but not M-protein significantly increased the exposure of thrombomodulin (Fig. 3a). Previous work has shown that exposure to dengue virus can increase the expression of thrombomodulin.7 Furthermore, children with chronic viral hepatitis, also exhibit an increase in thrombomodulin expression.27 In contrast, exposure to HSV has been shown to reduce the expression of thrombomodulin in endothelial cells.23 Combined, all of these data suggest that the expression of thrombomodulin is a function of the viral infection of the specific vascular bed investigated, but it is possible that SARS-CoV-2 structural proteins can interact with vascular endothelial cells to alter thrombotic functions during viral infection.
PECAM-1 is an adhesion molecule that is associated with vascular inflammatory functions. The expression of PECAM-1 after a 1 h exposure to SARS-CoV-2 was assessed and our data illustrate that S-protein and N-protein can instigate a significant increase in PECAM-1 expression as compared with both the negative control conditions and M-protein (Fig. 3b). In similar experiments, a 24 h exposure to dengue virus, reduced the expression of endothelial cell PECAM-1 and this was correlated to functional changes associated with the transendothelial migration of leukocytes and tight junction formation.20,22 Similarly, human cytomegalovirus induced the expression of multiple endothelial cell adhesion molecules, including PECAM-1 each of which was shown to relate to vascular inflammatory conditions.2 Thus, viral infections, including SARS-CoV-2 appear to be able to modulate vascular inflammatory processes through the enhanced expression of PECAM-1.
Connexin 43, a gap junction protein, plays a role in the formation of an endothelial sheet. We observed an increase in the expression of connexin 43 after a 1 h exposure to S-protein and M-protein but not N-protein (Fig. 3c). Similarly, Hsiao et al. show that a 48 h exposure to classical swine fever down-regulates connexin 43 gap junction expression.18 Although this is in contrast with our findings, it is important to point out that prior work illustrates that enhanced connexin 43 expression correlates with increased tumor cell metastasis and aggregation of glioma cells29,38 While the exact role of connexin 43 during viral infections remains to be determined, it is clear that altered expression of connexin 43 (both up- or down-regulation) can lead to severe pathologies.
Conclusions/Summary
It has become apparent that infections by SARS-CoV-2 can lead to significant pathologies. However, a basic understanding of the underlying molecular biology changes in response to SARS-CoV-2 structural proteins is missing. Thus, we aimed to determine the effects of a short duration exposure to SARS-CoV-2 structural proteins on endothelial cell culture parameters, gC1qR expression and inflammatory and thrombotic functions. Our data illustrate that SARS-CoV-2 structural proteins do not alter standard culture conditions over a 1 h time period, but that there are rapid and significant changes in the expression of molecules that are related to inflammatory and thrombotic progression. Our data also further supports the role of gC1qR, and specifically the C1q binding site on gC1qR, as a docking receptor for viral proteins. It is important to note that under physiological conditions, it would be possible for the various SARS-CoV-2 structural proteins to interact with different expressed gC1qR (and other endothelial cell receptors) at the same time, which may alter the observed response. However, our data illustrates that SARS-CoV-2 structural proteins can instigate vascular inflammatory and thrombotic responses in a complex manner that must be elucidated to understand the mechanisms of action of SARS-CoV-2.
References
Barber, K. E., B. Ghebrehiwet, W. Yin, and D. A. Rubenstein. Endothelial cell inflammatory reactions are altered in the presence of e-cigarette extracts of variable nicotine. Cell Mol. Bioeng. 10:124–133, 2017.
Bentz, G. L., M. Jarquin-Pardo, G. Chan, M. S. Smith, C. Sinzger, and A. D. Yurochko. Human cytomegalovirus (hcmv) infection of endothelial cells promotes naive monocyte extravasation and transfer of productive virus to enhance hematogenous dissemination of hcmv. J. Virol. 80:11539–11555, 2006.
Bermejo-Martin, J. F., R. Almansa, A. Torres, M. Gonzalez-Rivera, and D. J. Kelvin. Covid-19 as a cardiovascular disease: the potential role of chronic endothelial dysfunction. Cardiovasc. Res. 116:e132–e133, 2020.
Bleau, C., A. Filliol, M. Samson, and L. Lamontagne. Brain invasion by mouse hepatitis virus depends on impairment of tight junctions and beta interferon production in brain microvascular endothelial cells. J. Virol. 89:9896–9908, 2015.
Boackle, R. J., M. H. Connor, and J. Vesely. High molecular weight non-immunoglobulin salivary agglutinins (nia) bind c1q globular heads and have the potential to activate the first complement component. Mol. Immunol. 30:309–319, 1993.
Carson, S. D., J. T. Hobbs, S. M. Tracy, and N. M. Chapman. Expression of the coxsackievirus and adenovirus receptor in cultured human umbilical vein endothelial cells: regulation in response to cell density. J. Virol. 73:7077–7079, 1999.
Chen, L. C., H. W. Shyu, H. M. Lin, H. Y. Lei, Y. S. Lin, H. S. Liu, and T. M. Yeh. Dengue virus induces thrombomodulin expression in human endothelial cells and monocytes in vitro. J Infect. 58:368–374, 2009.
Didiasova, M., L. Wujak, L. Schaefer, and M. Wygrecka. Factor xii in coagulation, inflammation and beyond. Cell Signal. 51:257–265, 2018.
Doughan, A. K., D. G. Harrison, and S. I. Dikalov. Molecular mechanisms of angiotensin ii-mediated mitochondrial dysfunction: Linking mitochondrial oxidative damage and vascular endothelial dysfunction. Circ. Res. 102:488–496, 2008.
Du, Q., X. Wu, T. Wang, X. Yang, Z. Wang, Y. Niu, X. Zhao, S. L. Liu, D. Tong, and Y. Huang. Porcine circovirus type 2 suppresses il-12p40 induction via capsid/gc1qr-mediated micrornas and signalings. J. Immunol. 201:533–547, 2018.
Freda, C. T., W. Yin, B. Ghebrehiwet, and D. A. Rubenstein. Sars-cov-2 proteins regulate inflammatory, thrombotic and diabetic responses in human arterial fibroblasts. Clin. Immunol. 227:108733, 2021.
Gabriels, J. E., and D. L. Paul. Connexin43 is highly localized to sites of disturbed flow in rat aortic endothelium but connexin37 and connexin40 are more uniformly distributed. Circ. Res. 83:636–643, 1998.
Ghebrehiwet, B., J. Jesty, and E. I. Peerschke. Gc1q-r/p33: structure-function predictions from the crystal structure. Immunobiology. 205:421–432, 2002.
Ghebrehiwet, B., J. Jesty, S. Xu, R. Vinayagasundaram, U. Vinayagasundaram, Y. Ji, A. Valentino, K. K. Hosszu, S. Mathew, K. Joseph, A. P. Kaplan, and E. I. Peerschke. Structure-function studies using deletion mutants identify domains of gc1qr/p33 as potential therapeutic targets for vascular permeability and inflammation. Front. Immunol. 2:58, 2011.
Ghebrehiwet, B., Y. Ji, A. Valentino, L. Pednekar, M. Ramadass, D. Habiel, R. R. Kew, K. H. Hosszu, D. K. Galanakis, U. Kishore, and E. I. Peerschke. Soluble gc1qr is an autocrine signal that induces b1r expression on endothelial cells. J. Immunol. 192:377–384, 2014.
Ghebrehiwet, B., A. P. Kaplan, K. Joseph, and E. I. Peerschke. The complement and contact activation systems: partnership in pathogenesis beyond angioedema. Immunol. Rev. 274:281–289, 2016.
Guervilly, C., S. Burtey, F. Sabatier, R. Cauchois, G. Lano, E. Abdili, F. Daviet, L. Arnaud, P. Brunet, S. Hraiech, N. Jourde-Chiche, M. Koubi, R. Lacroix, L. Pietri, Y. Berda, T. Robert, C. Degioanni, M. Velier, L. Papazian, G. Kaplanski, and F. Dignat-George. Circulating endothelial cells as a marker of endothelial injury in severe covid -19. J. Infect. Dis. 222:1789–1793, 2020.
Hsiao, H. J., P. A. Liu, H. I. Yeh, and C. Y. Wang. Classical swine fever virus down-regulates endothelial connexin 43 gap junctions. Arch. Virol. 155:1107–1116, 2010.
Hu, M., H. M. Li, M. A. Bogoyevitch, and D. A. Jans. Mitochondrial protein p32/hapb1/gc1qr/c1qbp is required for efficient respiratory syncytial virus production. Biochem. Biophys. Res. Commun. 489:460–465, 2017.
Inyoo, S., A. Suttitheptumrong, and S. N. Pattanakitsakul. Synergistic effect of tnf-alpha and dengue virus infection on adhesion molecule reorganization in human endothelial cells. Jpn. J. Infect. Dis. 70:186–191, 2017.
Kaira, B. G., A. Slater, K. R. McCrae, I. Dreveny, U. Sumya, N. J. Mutch, M. Searle, and J. Emsley. Factor xii and kininogen asymmetric assembly with gc1qr/c1qbp/p32 is governed by allostery. Blood. 136:1685–1697, 2020.
Kanlaya, R., S. N. Pattanakitsakul, S. Sinchaikul, S. T. Chen, and V. Thongboonkerd. Alterations in actin cytoskeletal assembly and junctional protein complexes in human endothelial cells induced by dengue virus infection and mimicry of leukocyte transendothelial migration. J. Proteome Res. 8:2551–2562, 2009.
Key, N. S., G. M. Vercellotti, J. C. Winkelmann, C. F. Moldow, J. L. Goodman, N. L. Esmon, C. T. Esmon, and H. S. Jacob. Infection of vascular endothelial cells with herpes simplex virus enhances tissue factor activity and reduces thrombomodulin expression. Proc. Natl. Acad. Sci. U.S.A. 87:7095–7099, 1990.
Khan, M. M., H. N. Bradford, I. Isordia-Salas, Y. Liu, Y. Wu, R. G. Espinola, B. Ghebrehiwet, and R. W. Colman. High-molecular-weight kininogen fragments stimulate the secretion of cytokines and chemokines through upar, mac-1, and gc1qr in monocytes. Arterioscler. Thromb. Vasc. Biol. 26:2260–2266, 2006.
Kittlesen, D. J., K. A. Chianese-Bullock, Z. Q. Yao, T. J. Braciale, and Y. S. Hahn. Interaction between complement receptor gc1qr and hepatitis c virus core protein inhibits t-lymphocyte proliferation. J. Clin. Invest. 106:1239–1249, 2000.
Kopecky-Bromberg, S. A., L. Martinez-Sobrido, M. Frieman, R. A. Baric, and P. Palese. Severe acute respiratory syndrome coronavirus open reading frame (orf) 3b, orf 6, and nucleocapsid proteins function as interferon antagonists. J. Virol. 81:548–557, 2007.
Kulwas, A., A. Szaflarska-Szczepanik, M. Czerwionka-Szaflarska, and M. Kotschy. von willebrand factor and thrombomodulin as markers of endothelial cell functions in children with chronic viral hepatitis. Med. Wieku. Rozwoj. 8:107–114, 2004.
Liao, Y., K. H. Day, D. N. Damon, and B. R. Duling. Endothelial cell-specific knockout of connexin 43 causes hypotension and bradycardia in mice. Proc. Natl. Acad. Sci. U.S.A. 98:9989–9994, 2001.
Lin, J. H., T. Takano, M. L. Cotrina, G. Arcuino, J. Kang, S. Liu, Q. Gao, L. Jiang, F. Li, H. Lichtenberg-Frate, S. Haubrich, K. Willecke, S. A. Goldman, and M. Nedergaard. Connexin 43 enhances the adhesivity and mediates the invasion of malignant glioma cells. J. Neurosci. 22:4302–4311, 2002.
Loffi, M., R. Piccolo, V. Regazzoni, G. Di Tano, L. Moschini, D. Robba, F. Quinzani, G. Esposito, A. Franzone, G. B. Danzi, and Coronary artery disease in patients hospitalised with coronavirus disease. (covid-19) infection. Open Heart. 7:2020, 2019.
Luo, Y., H. Yu, and B. M. Peterlin. Cellular protein modulates effects of human immunodeficiency virus type 1 rev. J. Virol. 68:3850–3856, 1994.
Marra, M. A., S. J. Jones, C. R. Astell, R. A. Holt, A. Brooks-Wilson, Y. S. Butterfield, J. Khattra, J. K. Asano, S. A. Barber, S. Y. Chan, A. Cloutier, S. M. Coughlin, D. Freeman, N. Girn, O. L. Griffith, S. R. Leach, M. Mayo, H. McDonald, S. B. Montgomery, P. K. Pandoh, A. S. Petrescu, A. G. Robertson, J. E. Schein, A. Siddiqui, D. E. Smailus, J. M. Stott, G. S. Yang, F. Plummer, A. Andonov, H. Artsob, N. Bastien, K. Bernard, T. F. Booth, D. Bowness, M. Czub, M. Drebot, L. Fernando, R. Flick, M. Garbutt, M. Gray, A. Grolla, S. Jones, H. Feldmann, A. Meyers, A. Kabani, Y. Li, S. Normand, U. Stroher, G. A. Tipples, S. Tyler, R. Vogrig, D. Ward, B. Watson, R. C. Brunham, M. Krajden, M. Petric, D. M. Skowronski, C. Upton, and R. L. Roper. The genome sequence of the sars-associated coronavirus. Science. 300:1399–1404, 2003.
Matthews, D. A., and W. C. Russell. Adenovirus core protein v interacts with p32–a protein which is associated with both the mitochondria and the nucleus. J. Gen. Virol. 79(Pt 7):1677–1685, 1998.
Mutso, M., J. A. St John, Z. L. Ling, F. J. Burt, Y. S. Poo, X. Liu, E. Zusinaite, G. E. Grau, L. Hueston, A. Merits, N. J. C. King, J. A. K. Ekberg, and S. Mahalingam. Basic insights into zika virus infection of neuroglial and brain endothelial cells. J. Gen. Virol. 101:622–634, 2020.
Peerschke, E. I., A. S. Bayer, B. Ghebrehiwet, and Y. Q. Xiong. Gc1qr/p33 blockade reduces staphylococcus aureus colonization of target tissues in an animal model of infective endocarditis. Infect. Immunity. 74:4418–4423, 2006.
Peerschke, E. I., J. O. Minta, S. Z. Zhou, A. Bini, A. Gotlieb, R. W. Colman, and B. Ghebrehiwet. Expression of gc1q-r/p33 and its major ligands in human atherosclerotic lesions. Mol. Immunol. 41:759–766, 2004.
Pensiero, M. N., J. B. Sharefkin, C. W. Dieffenbach, and J. Hay. Hantaan virus infection of human endothelial cells. J. Virol. 66:5929–5936, 1992.
Pollmann, M. A., Q. Shao, D. W. Laird, and M. Sandig. Connexin 43 mediated gap junctional communication enhances breast tumor cell diapedesis in culture. Breast Cancer Res. 7:R522-534, 2005.
Risitano, A. M., D. C. Mastellos, M. Huber-Lang, D. Yancopoulou, C. Garlanda, F. Ciceri, and J. D. Lambris. Complement as a target in covid-19? Nat. Rev. Immunol. 20:343–344, 2020.
Rubenstein, D., D. Han, S. Goldgraben, H. El-Gendi, P. I. Gouma, and M. D. Frame. Bioassay chamber for angiogenesis with perfused explanted arteries and electrospun scaffolding. Microcirculation. 14:723–737, 2007.
Rubenstein, D. A., S. Hom, B. Ghebrehiwet, and W. Yin. Tobacco and e-cigarette products initiate kupffer cell inflammatory responses. Mol. Immunol. 67:652–660, 2015.
Rubenstein, D. A., Z. Maria, and W. Yin. Glycated albumin modulates endothelial cell thrombogenic and inflammatory responses. J. Diabetes Sci. Technol. 5:703–713, 2011.
Sainz, B., Jr., J. M. Rausch, W. R. Gallaher, R. F. Garry and W. C. Wimley. Identification and characterization of the putative fusion peptide of the severe acute respiratory syndrome-associated coronavirus spike protein. J. Virol. 79:7195–7206, 2005.
Singh, S., P. K. Singh, H. Suhail, V. Arumugaswami, P. E. Pellett, S. Giri, and A. Kumar. Amp-activated protein kinase restricts zika virus replication in endothelial cells by potentiating innate antiviral responses and inhibiting glycolysis. J. Immunol. 204:1810–1824, 2020.
Song, X., Z. Yao, J. Yang, Z. Zhang, Y. Deng, M. Li, C. Ma, L. Yang, X. Gao, W. Li, J. Liu, and L. Wei. Hcv core protein binds to gc1qr to induce a20 expression and inhibit cytokine production through mapks and nf-kappab signaling pathways. Oncotarget. 7:33796–33808, 2016.
Tang, N., D. Li, X. Wang, and Z. Sun. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 18:844–847, 2020.
Thondapu, V., D. Montes, R. Rosovsky, A. Dua, S. McDermott, M. T. Lu, B. Ghoshhajra, U. Hoffmann, M. D. Gerhard-Herman, and S. Hedgire. Venous thrombosis, thromboembolism, biomarkers of inflammation, and coagulation in coronavirus disease 2019. J. Vasc. Surg. Venous. Lymphat. Disord. 9(4):835–44, 2020.
Van de Wouwer, M., D. Collen, and E. M. Conway. Thrombomodulin-protein c-epcr system: integrated to regulate coagulation and inflammation. Arterioscler. Thromb. Vasc. Biol. 24:1374–1383, 2004.
Woodfin, A., M. B. Voisin, and S. Nourshargh. Pecam-1: A multi-functional molecule in inflammation and vascular biology. Arterioscler. Thromb. Vasc. Biol. 27:2514–2523, 2007.
Xu, J., S. Zhao, T. Teng, A. E. Abdalla, W. Zhu, L. Xie, Y. Wang and X. Guo. Systematic comparison of two animal-to-human transmitted human coronaviruses: Sars-cov-2 and sars-cov. Viruses 12:2020.
Yin, W., B. Ghebrehiwet, B. Weksler, and E. I. Peerschke. Classical pathway complement activation on human endothelial cells. Mol. Immunol. 44:2228–2234, 2007.
Zhang, K., Q. Hou, Z. Zhong, X. Li, H. Chen, W. Li, J. Wen, L. Wang, W. Liu, and F. Zhong. Porcine reproductive and respiratory syndrome virus activates inflammasomes of porcine alveolar macrophages via its small envelope protein e. Virology. 442:156–162, 2013.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Berhane Ghebrehiwet receives royalties from the sale of monoclonal antibodies against gC1qR clone 60.11. Berhane Ghebrehiwet holds a patent for the development of these antibodies for therapy against angioedema, respectively (US patent 8,883,153-B2, “Methods for Prevention and Treatment of Angioedema”) as well as against cancer. Christopher T. Freda, Wei Yin and David A. Rubenstein declare that they have no conflict of interest.
Research Involving Human Participants and/or Animals
No human studies were carried out by the authors for this article. No animal studies were carried out by the authors for this article.
Additional information
Associate Editor Michael R. King oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Freda, C.T., Yin, W., Ghebrehiwet, B. et al. SARS-CoV-2 Structural Proteins Exposure Alter Thrombotic and Inflammatory Responses in Human Endothelial Cells. Cel. Mol. Bioeng. 15, 43–53 (2022). https://doi.org/10.1007/s12195-021-00696-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12195-021-00696-7