Abstract
Background
Basal cell carcinoma (BCC) is the most common human cancer. Facial BCCs most commonly occur on the nose and the management of these lesions is particularly complex, given the functional and complex implications of treatment. Multidisciplinary team (MDT) meetings are routinely held to integrate expertise from dermatologists, surgeons, oncologists, radiologists, pathologists and allied health professionals. The aim of this research was to develop a supervised machine-learning algorithm to predict MDT recommendations for nasal BCC to potentially reduce MDT caseload, provide automatic decision support and permit data audit in a health service context.
Methods
The study population included all consecutive patients who were discussed at skin cancer-specialised MDT (SSMDT) with a diagnosis of nasal BCC between January 1, 2015 and December 31, 2015. We conducted analyses for gender, age, anatomical location, histological subtype, tumour size, tumour recurrence, anticoagulation, pacemaker, immunosuppressants and therapeutic modalities (Mohs surgery, conventional excision or radiotherapy). We used S-statistic computing language to develop a supervised machine-learning algorithm.
Results
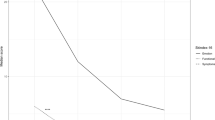
We found that 37.5% of patients could be reliably predicted to be triaged to Mohs micrographic surgery (MMS), based on tumour location and age. Similarly, the choice of conventional treatment (surgical excision or radiotherapy) by the MDT could be reliably predicted based on the patient’s age, tumour phenotype and lesion size. Accordingly, the algorithm reliably predicted the MDT decision outcome of 45.1% of nasal BCCs.
Conclusions
Our study suggests that the machine-learning approach is a potentially useful tool for predicting MDT decisions for MMS vs conventional surgery or radiotherapy for a significant group of patients. We suggest that utilising this algorithm gives the MDT more time to consider more complex patients, where multiple factors, including recurrence, financial costs and cosmetic outcome, contribute to the final decision, but cannot be reliably predicted to determine that outcome. This approach has the potential to reduce the burden and improve the efficiency of the specialist skin MDT and, in turn, improve patient care, reduce waiting times and reduce the financial burden. Such an algorithm would need to be updated regularly to take into account any changes in patient referral patterns, treatment options or local clinical expertise.
Clinical Trial Registration
lPLAS_20-21_A08.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Data cannot be shared publicly due to the violation of patient confidentiality and the absence of informed consent for public data sharing. Data are available to researchers who meet the criteria for access to confidential NHS data; requests should be made to T Andrew, Department of Plastic and Reconstructive Surgery, Norfolk and Norwich University Hospital (tom.andrew@nhs.net).
References
Bichakjian C, Armstrong A, Baum C, Bordeaux J, Brown M, Busam K, et al. Guidelines of care for the management of basal cell carcinoma. J Am Acad Dermatol. 2018. https://doi.org/10.1016/j.jaad.2017.10.006.
Cancer Research UK. Non-melanoma skin cancer incidence statistics. 2018. https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/non-melanoma-skin-cancer/incidence. Accessed10 Oct 2020.
Rubin AI, Chen EH, Ratner D. Basal-cell carcinoma. N Engl J Med. 2005. https://doi.org/10.1056/NEJMra044151.
Taylor C, Munro AJ, Glynne-Jones R, Griffith C, Trevatt P, Richards M, et al. Multidisciplinary team working in cancer: What is the evidence? BMJ. 2010. https://doi.org/10.1136/bmj.c951.
NHS England and NHS Improvement. Streamlining multi-disciplinary team meetings. 2020. https://www.england.nhs.uk/wp-content/uploads/2020/01/multi-disciplinary-team-streamlining-guidance.pdf. Accessed 13 Jan 2021.
Soukup T, Morbi A, Lamb BW, Gandamihardja T, Hogben K, Noyes K, et al. A measure of case complexity for streamlining workflow in multidisciplinary tumor boards: mixed methods development and early validation of the MeDiC tool. Cancer Med. 2020. https://doi.org/10.1002/cam4.3026.
NICE. Improving outcomes for people with skin tumours including melanoma: evidence update October 2011. NHS Evidence. National Institute for Health and Care Excellence; 2011. https://www.nice.org.uk/guidance/csg8/resources/improving-outcomes-for-people-with-skin-tumours-including-melanoma-2010-partial-update-pdf-773380189. Accessed 13 Jan 2021.
Soukup T, Lamb BW, Morbi A, Shah N, Bali A, Asher V, et al. A multicentre cross-sectional observational study of cancer multidisciplinary teams: analysis of team decision making. Cancer Med. 2020. https://doi.org/10.1002/cam4.3366.
Therneau T, Atkinson B, Ripley B. rpart: recursive partitioning. version 4.1-1. 2013.https://cran.r-project.org/web/packages/rpart/vignettes/longintro.pdf.
Esteva A, Kuprel B, Novoa RA, Ko J, Swetter S, Blau H, et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature. 2017. https://doi.org/10.1038/nature21056.
Van Loo E, Mosterd K, Krekels GAM, Roozeboom M, Ostertag J, Dirksen C, et al. Surgical excision versus Mohs’ micrographic surgery for basal cell carcinoma of the face: a randomised clinical trial with 10 year follow-up. Eur J Cancer. 2014. https://doi.org/10.1016/j.ejca.2014.08.018.
Kesson EM, Allardice GM, George WD, Burns HJG, Morrison DS. Effects of multidisciplinary team working on breast cancer survival: retrospective, comparative, interventional cohort study of 13 722 women. BMJ. 2012. https://doi.org/10.1136/bmj.e2718.
Soukup T, Gandamihardja TAK, McInerney S, Green JSA, Sevdalis N. Do multidisciplinary cancer care teams suffer decision-making fatigue: an observational, longitudinal team improvement study. BMJ Open. 2019. https://doi.org/10.1136/bmjopen-2018-027303.
Camarero-Mulas C, Delgado Jiménez Y, Sanmartín-Jiménez O, Garces J, Rodriguez-Prieto M, Alonso-Alonso T, et al. Mohs micrographic surgery in the elderly: comparison of tumours, surgery and first-year follow-up in patients younger and older than 80 years old in REGESMOHS. J Eur Acad Dermatology Venereol. 2018. https://doi.org/10.1111/jdv.14586.
Charles AJ, Otley CC, Pond GR. Prognostic factors for life expectancy in nonagenarians with nonmelanoma skin cancer: implications for selecting surgical candidates. J Am Acad Dermatol. 2002. https://doi.org/10.1067/mjd.2002.122740.
Hoorens I, Batteauw A, Van Maele G, Lapiere K, Boone B, Ongenae K. Mohs micrographic surgery for basal cell carcinoma: evaluation of the indication criteria and predictive factors for extensive subclinical spread. Br J Dermatol. 2016. https://doi.org/10.1111/bjd.14308.
Mosterd K, Krekels GA, Nieman FH, Ostertag J, Essers B, Dirksen C, et al. Surgical excision versus Mohs’ micrographic surgery for primary and recurrent basal-cell carcinoma of the face: a prospective randomised controlled trial with 5-years’ follow-up. Lancet Oncol. 2008. https://doi.org/10.1016/S1470-2045(08)70260-2.
Masood A, Al-Jumaily AA. Computer aided diagnostic support system for skin cancer: a review of techniques and algorithms. Int J Biomed Imaging. 2013. https://doi.org/10.1155/2013/323268.
Dick V, Sinz C, Mittlböck M, Kittler H, Tschandl P. Accuracy of computer-aided diagnosis of melanoma: a meta-analysis. JAMA Dermatol. 2019. https://doi.org/10.1001/jamadermatol.2019.1375.
Binder M, Kittler H, Seeber A, Steiner A, Pehamberger H, Wolff K. Epiluminescence microscopy-based classification of pigmented skin lesions using computerized image analysis and an artificial neural network. Melanoma Res. 1998. https://doi.org/10.1097/00008390-199806000-00009.
Kalderstam J, Edén P, Ohlsson M. Finding risk groups by optimizing artificial neural networks on the area under the survival curve using genetic algorithms. PLoS ONE. 2015. https://doi.org/10.1371/journal.pone.0137597.
Lin FPY, Pokorny A, Teng C, Dear R, Epstein RJ. Computational prediction of multidisciplinary team decision-making for adjuvant breast cancer drug therapies: a machine learning approach. BMC Cancer. 2016. https://doi.org/10.1186/s12885-016-2972-z.
Somashekhar SP, Sepúlveda MJ, Puglielli S, Norden A, Shortliffe E, Rohit Kumar C, et al. Watson for oncology and breast cancer treatment recommendations: agreement with an expert multidisciplinary tumor board. Ann Oncol. 2018. https://doi.org/10.1093/annonc/mdx781.
Acknowledgements
Not applicable.
Funding
None of the authors has a financial interest in any of the products, devices or drugs mentioned in this paper.
Author information
Authors and Affiliations
Contributions
TWA: designed the study, gathered and analysed data and wrote the paper. NH: gathered data. IR: gathered data. JG: designed the study and analysed the data. JN: designed the study and analysed the data. MDM: designed the study, analysed the data and wrote the paper.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Patient electronic records, including the specialised skin MDT forms, were obtained with the approval of the Clinical Audit and Improvement Department at the Norfolk and Norwich University Hospital (approval code: lPLAS_20-21_A08). The study was performed in accordance with the Declaration of Helsinki.
Consent to publish
No individual person’s data in any form are included in this publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Andrew, T.W., Hamnett, N., Roy, I. et al. Machine-learning algorithm to predict multidisciplinary team treatment recommendations in the management of basal cell carcinoma. Br J Cancer 126, 562–568 (2022). https://doi.org/10.1038/s41416-021-01506-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-021-01506-7
This article is cited by
-
The Oesophageal Cancer Multidisciplinary Team: Can Machine Learning Assist Decision-Making?
Journal of Gastrointestinal Surgery (2023)
-
Clinical Application of Artificial Intelligence for Non-melanoma Skin Cancer
Current Treatment Options in Oncology (2023)