Abstract
Introduction
The esophagogastric junction (EGJ) is a complex anti-reflux barrier whose integrity relies on both the intrinsic lower esophageal sphincter (LES) and extrinsic crural diaphragm. During hiatal hernia repair, it is unclear whether the crural closure or the fundoplication is more important to restore the anti-reflux barrier. The objective of this study is to analyze changes in LES minimum diameter (Dmin) and distensibility index (DI) using the endoluminal functional lumen imaging probe (FLIP) during hiatal hernia repair.
Methods
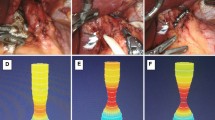
Following implementation of a standardized operative FLIP protocol, all data were collected prospectively and entered into a quality database. This data were reviewed retrospectively for all patients undergoing hiatal hernia repair. FLIP measurements were collected prior to hernia dissection, after hernia reduction, after cruroplasty, and after fundoplication. Additionally, subjective assessment of the tightness of crural closure was rated by the primary surgeon on a scale of 1 to 5, 1 being the loosest and 5 being the tightest.
Results
Between August 2018 and February 2020, 97 hiatal hernia repairs were performed by a single surgeon. FLIP measurements collected using a 40-mL volume fill without pneumoperitoneum demonstrated a significant decrease in LES Dmin (13.84 ± 2.59 to 10.27 ± 2.09) and DI (6.81 ± 3.03 to 2.85 ± 1.23 mm2/mmHg) after crural closure (both p < 0.0001). Following fundoplication, there was a small, but also statistically significant, increase in both Dmin and DI (both p < 0.0001). Additionally, subjective assessment of crural tightness after cruroplasty correlated well with DI (r = − 0.466, p < 0.001) and all patients with a crural tightness rating ≥ 4.5 (N = 13) had a DI < 2.0 mm2/mmHg.
Conclusion
Cruroplasty results in a significant decrease in LES distensibility and may be more important than fundoplication in restoring EGJ competency. Additionally, subjective estimation of crural tightness correlates well with objective FLIP evaluation, suggesting surgeon assessment of cruroplasty is reliable.




Similar content being viewed by others
References
Peery AF, Dellon ES, Lund J, Crockett SD, McGowan CE, Bulsiewicz WJ, Gangarosa LM, Thiny MT, Stizenberg K, Morgan DR, Ringel Y, Kim HP, DiBonaventura MD, Carroll CF, Allen JK, Cook SF, Sandler RS, Kappelman MD, Shaheen NJ (2012) Burden of gastrointestinal disease in the United States: 2012 Update. Gastroenterology 143:1179-1187.e3. https://doi.org/10.1053/j.gastro.2012.08.002
Richter JE (2007) The many manifestations of gastroesophageal reflux disease: presentation, evaluation, and treatment. Gastroenterol Clin North Am 36:577–599. https://doi.org/10.1016/j.gtc.2007.07.014
Mikami DJ, Murayama KM (2015) Physiology and pathogenesis of gastroesophageal reflux disease. Surg Clin North Am 95:515–525. https://doi.org/10.1016/j.suc.2015.02.006
Frazzoni M (2014) Laparoscopic fundoplication for gastroesophageal reflux disease. WJG 20:14272. https://doi.org/10.3748/wjg.v20.i39.14272
Broeders JA, Rijnhart-de Jong HG, Draaisma WA, Bredenoord AJ, Smout AJ, Gooszen HG (2009) Ten-year outcome of laparoscopic and conventional nissen fundoplication: randomized clinical trial. Ann Surg 250:698–706. https://doi.org/10.1097/SLA.0b013e3181bcdaa7
Ross SB, Gal S, Teta AF, Luberice K, Rosemurgy AS (2013) Late results after laparoscopic fundoplication denote durable symptomatic relief of gastroesophageal reflux disease. Am J Surg 206:47–51. https://doi.org/10.1016/j.amjsurg.2012.10.032
Dallemagne B, Weerts J, Markiewicz S, Dewandre J-M, Wahlen C, Monami B, Jehaes C (2006) Clinical results of laparoscopic fundoplication at ten years after surgery. Surg Endosc 20:159–165. https://doi.org/10.1007/s00464-005-0174-x
Engström C, Cai W, Irvine T, Devitt PG, Thompson SK, Game PA, Bessell JR, Jamieson GG, Watson DI (2012) Twenty years of experience with laparoscopic antireflux surgery: laparoscopic antireflux surgery. Br J Surg 99:1415–1421. https://doi.org/10.1002/bjs.8870
Dallemagne B, Perretta S (2011) Twenty years of laparoscopic fundoplication for GERD. World J Surg 35:1428–1435. https://doi.org/10.1007/s00268-011-1050-6
Galmiche J-P, Hatlebakk J, Attwood S, Ell C, Fiocca R, Eklund S, Långström G, Lind T, Lundell L, LOTUS Trial Collaborators for the (2011) Laparoscopic antireflux surgery vs esomeprazole treatment for chronic GERD: the LOTUS randomized clinical trial. JAMA. https://doi.org/10.1001/jama.2011.626
Rossetti G, Limongelli P, Cimmino M, Napoletano D, Bondanese MC, Romano G, Pratilas M, Guerriero L, Orlando F, Conzo G, Amato B, Docimo G, Tolone S, Brusciano L, Docimo L, Fei L (2014) Outcome of medical and surgical therapy of GERD: predictive role of quality of life scores and instrumental evaluation. Int J Surg 12:S112–S116. https://doi.org/10.1016/j.ijsu.2014.05.034
Louie BE, Kapur S, Blitz M, Farivar AS, Vallières E, Aye RW (2013) Length and pressure of the reconstructed lower esophageal sphincter is determined by both crural closure and Nissen fundoplication. J Gastrointest Surg 17:236–243. https://doi.org/10.1007/s11605-012-2074-4
Kahrilas PJ, Lee TJ (2005) Pathophysiology of gastroesophageal reflux disease. Thorac Cardiovasc Surg 15:323–333. https://doi.org/10.1016/j.thorsurg.2005.03.005
Morais DJ, Lopes LR, Andreollo NA (2014) Dysphagia after antireflux fundoplication: endoscopic, radiological and manometric evaluation. ABCD, Arq Bras Cir Dig 27:251–255. https://doi.org/10.1590/S0102-67202014000400006
Nikolic M, Schwameis K, Semmler G, Asari R, Semmler L, Steindl A, Mosleh BO, Schoppmann SF (2019) Persistent dysphagia is a rare problem after laparoscopic Nissen fundoplication. Surg Endosc 33:1196–1205. https://doi.org/10.1007/s00464-018-6396-5
Funch-Jensen P, Jacobsen B (2007) Dysphagia after laparoscopic Nissen fundoplication. Scand J Gastroenterol 42:428–431. https://doi.org/10.1080/00365520600955120
Humphries LA, Hernandez JM, Clark W, Luberice K, Ross SB, Rosemurgy AS (2013) Causes of dissatisfaction after laparoscopic fundoplication: the impact of new symptoms, recurrent symptoms, and the patient experience. Surg Endosc 27:1537–1545. https://doi.org/10.1007/s00464-012-2611-y
Walle KV, Funk LM, Xu Y, Davies KD, Greenberg J, Shada A, Lidor A (2019) Persistent dysphagia rate after antireflux surgery is similar for Nissen fundoplication and partial fundoplication. J Surg Res 235:52–57. https://doi.org/10.1016/j.jss.2018.09.036
Granderath FA, Schweiger UM, Kamolz T, Pointner R (2005) Dysphagia after laparoscopic antireflux surgery: a problem of hiatal closure more than a problem of the wrap. Surg Endosc 19:1439–1446. https://doi.org/10.1007/s00464-005-0034-8
McMahon BP, Frøkjær JB, Kunwald P, Liao D, Funch-Jensen P, Drewes AM, Gregersen H (2007) The functional lumen imaging probe (FLIP) for evaluation of the esophagogastric junction. Am J Physiol Gastrointest Liver Physiol 292:G377–G384. https://doi.org/10.1152/ajpgi.00311.2006
Kwiatek MA, Kahrilas PJ, Soper NJ, Bulsiewicz WJ, McMahon BP, Gregersen H, Pandolfino JE (2010) Esophagogastric junction distensibility after fundoplication assessed with a novel functional luminal imaging probe. J Gastrointest Surg 14:268–276. https://doi.org/10.1007/s11605-009-1086-1
Kwiatek MA, Pandolfino JE, Hirano I, Kahrilas PJ (2010) Esophagogastric junction distensibility assessed with an endoscopic functional luminal imaging probe (EndoFLIP). Gastrointest Endosc 72:272–278. https://doi.org/10.1016/j.gie.2010.01.069
Kahrilas PJ, Lin S, Manka M, Shi G, Joehl RJ (2000) Esophagogastric junction pressure topography after fundoplication. Surgery 127:200–208. https://doi.org/10.1067/msy.2000.102045
Su B, Callahan ZM, Kuchta K, Linn JG, Haggerty SP, Denham W, Ujiki MB (2020) Use of impedance planimetry (EndoFlip) in foregut surgery practice: experience of more than 400 cases. J Am Coll Surg 231:160–171. https://doi.org/10.1016/j.jamcollsurg.2020.02.017
Su B, Novak S, Callahan ZM, Kuchta K, Carbray J, Ujiki MB (2020) Using impedance planimetry (EndoFLIPTM) in the operating room to assess gastroesophageal junction distensibility and predict patient outcomes following fundoplication. Surg Endosc 34:1761–1768. https://doi.org/10.1007/s00464-019-06925-5
Watson DI, Jamieson GG, Devitt PG, Mitchell PC, Game PA (1995) Paraoesophageal hiatus hernia: an important complication of laparoscopic Nissen fundoplication. Br J Surg 82:521–523. https://doi.org/10.1002/bjs.1800820428
Kelly JJ, Watson DI, Chin KF, Devitt PG, Game PA, Jamieson GG (2007) Laparoscopic Nissen fundoplication: clinical outcomes at 10 years. J Am Coll Surg 205:570–575. https://doi.org/10.1016/j.jamcollsurg.2007.05.024
Cowgill SM, Gillman R, Kraemer E, Al-Saadi S, Villadolid D, Rosemurgy A (2007) Ten-year follow up after laparoscopic Nissen fundoplication for gastroesophageal reflux disease. Am Surg 73:748–753. https://doi.org/10.1177/000313480707300803
Sloan S, Rademaker AW, Kahrilas PJ (1992) Determinants of gastroesophageal junction incompetence: hiatal hernia, lower esophageal sphincter, or both? Ann Intern Med 117:977–982. https://doi.org/10.7326/0003-4819-117-12-977
Pandolfino J, Shi G, Manka M, Joehl R, Brasseur J, Kahrilas P (2000) EGJ opening with hiatal hernia: lower pressure threshold, wider diameter. Gastroenterology. https://doi.org/10.1016/S0016-5085(00)85581-X
Pandolfino JE, Kim H, Ghosh SK, Clarke JO, Zhang Q, Kahrilas PJ (2007) High-resolution manometry of the EGJ: an analysis of crural diaphragm function in GERD. Am J Gastroenterol 102:1056–1063. https://doi.org/10.1111/j.1572-0241.2007.01138.x
Irribarra MM, Blitz S, Wilshire CL, Jackson AS, Farivar AS, Aye RW, Dunst CM, Louie BE (2019) Does treatment of the hiatus influence the outcomes of magnetic sphincter augmentation for chronic GERD? J Gastrointest Surg 23:1104–1112. https://doi.org/10.1007/s11605-019-04180-6
Su B, Wong HJ, Attaar M, Kuchta K, Linn JG, Haggerty SP, Denham W, Ujiki MB (2020) Comparing short-term patient outcomes after fundoplication performed over a traditional bougie versus a functional lumen imaging probe. Surgery. https://doi.org/10.1016/j.surg.2020.07.027
Manzo CA, Asti E, Bonavina L (2020) Hiatal hernia, lower esophageal sphincter and their combined effect on the natural history of gastroesophageal reflux disease: implications for surgical therapy. Ann Laparosc Endosc Surg. https://doi.org/10.21037/ales-20-26
Pandolfino JE, Curry J, Shi G, Joehl RJ, Brasseur JG, Kahrilas PJ (2005) Restoration of normal distensive characteristics of the esophagogastric junction after fundoplication. Ann Surg 242:6
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Disclosure Information: Dr. Ujiki received speaker payments from Medtronic for instructional courses on the use of FLIP. Disclosures outside the scope of this work: Drs. Mikhail Attaar and Stephen P. Haggerty are supported by an institutional grant from Intuitive Foundation. Drs. John G. Linn, Stephen P. Haggerty, and Michael B. Ujiki receive payment for lectures from Gore. Dr. Michael B. Ujiki is a board member for Boston Scientific, is a paid consultant to Olympus and Cook, and receives payment for lectures from Medtronic, GORE, and Erbe. Dr. Stephen P. Haggerty received consultant and speaker fees from the renal division of Medtronic for work with peritoneal dialysis catheters and insertion techniques, development of educational materials, and serving as a lecturer and proctor for hands-on courses. Drs. Bailey Su, Harry Wong, Zachary Callahan, and Woody Denham, Ms. Kristine Kuchta, and Mr. Stephen Stearns have no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Attaar, M., Su, B., Wong, H. et al. Crural closure, not fundoplication, results in a significant decrease in lower esophageal sphincter distensibility. Surg Endosc 36, 3893–3901 (2022). https://doi.org/10.1007/s00464-021-08706-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08706-5