Abstract
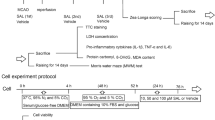
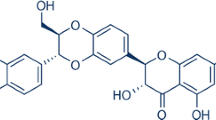
Exploring and repurposing a drug have become a lower risk alternative. Safinamide, approved for Parkinson’s disease, has shown neuroprotection in various animal models of neurological disorders. The present study aimed to explore the potential of safinamide in cerebral ischemia/reperfusion (I/R) in rats. Sprague–Dawley rats were used in middle cerebral artery occlusion model of stroke. The effective dose of safinamide was selected based on the results of neurobehavioral parameters and reduction in infarct size assessed 24 h post-reperfusion. For sub-acute study, the treatment with effective dose was extended for 3 days and effects on neurobehavioral parameters, infarct size (TTC staining and MRI), oxidative stress parameters (MDA, GSH, SOD, NOX-2), inflammatory cytokines (TNF-α, IL-1β, IL-10), apoptosis (Bax, Bcl-2, cleaved caspase-3 expression, and TUNEL staining), and autophagy (pAMPK, Beclin-1, LC3-II expression) were studied. The results of dose selection study showed significant reduction (p < 0.05) in infarct size and improvement in neurobehavioral parameters with safinamide (80 mg/kg). In sub-acute study, safinamide showed significant (p < 0.05) improvement in motor coordination and infarct size reduction. Additionally, safinamide treatment significantly normalized altered redox homeostasis and inflammatory cytokine levels. However, no change was observed in expression of NOX-2 in I/R or safinamide treatment group when compared with sham. I/R induced deranged expression of apoptotic markers and increased TUNEL positive cells in cortex were significantly normalized with safinamide treatment. Further, safinamide significantly (p < 0.05) induced the expressions of autophagic proteins (Beclin-1 and LC3-II) in cortex. Overall, the results demonstrated neuroprotective potential of safinamide via anti-oxidant, anti-inflammatory, anti-apoptotic, and autophagy inducing properties. Thus, safinamide can be explored for repurposing in ischemic stroke after further exploration.








Similar content being viewed by others
Data Availability
The datasets generated and analysed during the current study are available from the corresponding author upon request.
Code Availability
NA.
References
Saver JL (2006) Time is brain–quantified. Stroke 37:263–266. https://doi.org/10.1161/01.STR.0000196957.55928.ab
Campbell BCV, Khatri P (2020) Stroke. Lancet 396:129–142. https://doi.org/10.1016/S0140-6736(20)31179-X
Johnson CO, Nguyen M, Roth GA et al (2019) Global, regional, and national burden of stroke, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 18:439–458. https://doi.org/10.1016/S1474-4422(19)30034-1
Xing C, Arai K, Lo EH, Hommel M (2012) Pathophysiologic cascades in ischemic stroke. Int J Stroke 7(5):378–385. https://doi.org/10.1111/j.1747-4949.2012.00839.x
Dirnagl U, Iadecola C, Moskowitz MA (1999) Pathobiology of ischaemic stroke: an integrated view. Trends Neurosci 22:391–397. https://doi.org/10.1016/s0166-2236(99)01401-0
Goyal M, Menon BK, Van Zwam WH et al (2016) Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 387:1723–1731. https://doi.org/10.1016/S0140-6736(16)00163-X
Bette S, Shpiner DS, Singer C, Moore H (2018) Safinamide in the management of patients with Parkinson’s disease not stabilized on levodopa: a review of the current clinical evidence. Ther Clin Risk Manag 14:1737–1745. https://doi.org/10.2147/TCRM.S139545
Deeks ED (2015) Safinamide: First global approval. Drugs 75:705–711. https://doi.org/10.1007/s40265-015-0389-7
Fariello RG (2007) Safinamide. Neurotherapeutics 4:110–116. https://doi.org/10.1016/j.nurt.2006.11.011
Caccia C, Maj R, Calabresi M et al (2006) Safinamide: from molecular targets to a new anti-Parkinson drug. Neurology 67(7):S18–S23. https://doi.org/10.1212/wnl.67.7_suppl_2.s18
Morsali D, Bechtold D, Lee W et al (2013) Safinamide and flecainide protect axons and reduce microglial activation in models of multiple sclerosis. Brain 136:1067–1082. https://doi.org/10.1093/brain/awt041
Sadeghian M, Mullali G, Pocock JM et al (2016) Neuroprotection by safinamide in the 6-hydroxydopamine model of Parkinson’s disease. Neuropathol Appl Neurobiol 42:423–435. https://doi.org/10.1111/nan.12263
Desaphy JF, Farinato A, Altamura C et al (2020) Safinamide’s potential in treating nondystrophic myotonias: inhibition of skeletal muscle voltage-gated sodium channels and skeletal muscle hyperexcitability in vitro and in vivo. Exp Neurol 328:9–10. https://doi.org/10.1016/j.expneurol.2020.113287
Xu T, Sun R, Wei G, Kong S (2020) The protective effect of safinamide in ischemic stroke mice and a brain endothelial cell line. Neurotox Res 38(3):733–740. https://doi.org/10.1007/s12640-020-00246-5
Wasan H, Singh D, KH R, (2021) Safinamide in neurological disorders and beyond: evidence from preclinical and clinical studies. Brain Res Bull 168:165–177. https://doi.org/10.1016/j.brainresbull.2020.12.018
Curtis MJ, Alexander S, Cirino G et al (2018) Experimental design and analysis and their reporting II: updated and simplified guidance for authors and peer reviewers. Br J Pharmacol 175:987–993. https://doi.org/10.1111/bph.14153
Stocchi F, Vacca L, Grassini P et al (2006) Symptom relief in Parkinson disease by safinamide: biochemical and clinical evidence of efficacy beyond MAO-B inhibition. Neurology 67:S24–S29. https://doi.org/10.1212/wnl.67.7_suppl_2.s24
Longa EZ, Weinstein PR, Carlson S, Cummins R (1989) Reversible middle cerebral artery occlusion without craniectomy in rats. Stroke 20:84–91. https://doi.org/10.1161/01.STR.20.1.84
Rogers DC, Campbell CA, Stretton JL, Mackay KB (1997) Correlation between motor impairment and infarct volume after permanent and transient middle cerebral artery occlusion in the rat. Stroke 28:2060–2065. https://doi.org/10.1161/01.str.28.10.2060
Moran PM, Higginst LS, Cordellt B, Moser PC (1995) Age-related learning deficits in transgenic mice expressing the 751-amino acid isoform of human 18-amyloid precursor protein. Proc Natl Acad Sci U S A 92(12):5341–5345. https://doi.org/10.1073/pnas.92.12.5341
Bederson JB, Pitts LH, Germano SM et al (1986) Evaluation of 2, 3, 5-triphenyltetrazolium chloride as a stain for detection and quantification of experimental cerebral infarction in rats. Stroke 17:1304–1308. https://doi.org/10.1161/01.STR.17.6.1304
Glowinski J, Iversen LL (1966) Regional studies of catecholamines in the rat brain. I. The disposition of [3H]norepinephrine, [3H]dopamine and [3H]dopa in various regions of the brain. J Neurochem 13:655–669. https://doi.org/10.1111/j.1471-4159.1966.tb09873.x
Ohkawa H, Ohishi N, Yagi K (1979) Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 95(2):351–358. https://doi.org/10.1016/0003-2697(79)90738-3
Ellman GL (1959) Tissue sulfhydryl groups. Arch Biochem Biophys 82(1):70–77. https://doi.org/10.1016/0003-9861(59)90090-6
Marklund S, Marklund G (1974) Involvement of the superoxide anion radical in the autoxidation of pyrogallol and a convenient assay for superoxide dismutase. Eur J Biochem 47(3):469–474. https://doi.org/10.1111/j.1432-1033.1974.tb03714.x
Singh D, Reeta KH, Sharma U et al (2019) Neuro-protective effect of monomethyl fumarate on ischemia reperfusion injury in rats: role of Nrf2/HO1 pathway in peri-infarct region. Neurochem Int 126:96–108. https://doi.org/10.1016/j.neuint.2019.03.010
Armogida M, Nisticò R, Mercuri NB (2012) Therapeutic potential of targeting hydrogen peroxide metabolism in the treatment of brain ischaemia. Br J Pharmacol 166:1211–1224. https://doi.org/10.1111/j.1476-5381.2012.01912.x
Ogawa A, Yoshimoto T, Kikuchi H et al (1999) Ebselen in acute middle cerebral artery occlusion: a placebo-controlled, double-blind clinical trial. Cerebrovasc Dis 9:112–118. https://doi.org/10.1159/000015908
Kahles T, Brandes RP (2012) NADPH oxidases as therapeutic targets in ischemic stroke. Cell Mol Life Sci 69:2345–2363. https://doi.org/10.1007/s00018-012-1011-8
Kahles T, Brandes RP (2013) Which NADPH oxidase isoform is relevant for ischemic stroke? The case for Nox 2. Antioxid Redox Signal 18:1400–1417. https://doi.org/10.1089/ars.2012.4721
Yao H, Ago T, Kitazono T, Nabika T (2017) NADPH oxidase-related pathophysiology in experimental models of stroke. Int J Mol Sci 18(10):2123. https://doi.org/10.3390/IJMS18102123
Li H, Wang Y, Feng D et al (2014) Alterations in the time course of expression of the Nox family in the brain in a rat experimental cerebral ischemia and reperfusion model: effects of melatonin. J Pineal Res 57:110–119. https://doi.org/10.1111/jpi.12148
McCann SK, Dusting GJ, Roulston CL (2014) Nox2 knockout delays infarct progression and increases vascular recovery through angiogenesis in mice following ischaemic stroke with reperfusion. PLoS ONE 9:1–13. https://doi.org/10.1371/journal.pone.0110602
Nardai S, László M, Szabó A et al (2020) N, N-Dimethyltryptamine reduces infarct size and improves functional recovery following transient focal brain ischemia in rats. Exp Neurol 327:113245. https://doi.org/10.1016/j.expneurol.2020.113245
Pawluk H, Wozniak A, Grzesk G et al (2020) The role of selected pro-inflammatory cytokines in pathogenesis of ischemic stroke. Clin Interv Aging 15:469–484. https://doi.org/10.2147/CIA.S233909
Mizuma A, You JS, Yenari MA (2018) Targeting reperfusion injury in the age of mechanical thrombectomy. Stroke 49(7):1796–1802. https://doi.org/10.1161/STROKEAHA.117.017286
Emsley HCA, Smith CJ, Georgiou RF et al (2005) A randomised phase II study of interleukin-1 receptor antagonist in acute stroke patients. J Neurol Neurosurg Psychiatry 76:1366–1372. https://doi.org/10.1136/jnnp.2004.054882
Smith CJ, Hulme S, Vail A et al (2018) SCIL-STROKE (subcutaneous interleukin-1 receptor antagonist in ischemic stroke): a randomized controlled phase 2 trial. Stroke 49:1210–1216. https://doi.org/10.1161/STROKEAHA.118.020750
Hu X, Li P, Guo Y et al (2012) Microglia/macrophage polarization dynamics reveal novel mechanism of injury expansion after focal cerebral ischemia. Stroke 43:3063–3070. https://doi.org/10.1161/STROKEAHA.112.659656
Suenaga J, Hu X, Pu H et al (2015) White matter injury and microglia/macrophage polarization are strongly linked with age-related long-term deficits in neurological function after stroke. Exp Neurol 272:109–119. https://doi.org/10.1016/J.EXPNEUROL.2015.03.021
Chelluboina B, Klopfenstein JD, Gujrati M et al (2014) Temporal regulation of apoptotic and anti-apoptotic molecules after middle cerebral artery occlusion followed by reperfusion. Mol Neurobiol 49:50–65
Yuan J (2009) Neuroprotective strategies targeting apoptotic and necrotic cell death for stroke. Apoptosis 14:469–477. https://doi.org/10.1007/s10495-008-0304-8
Liu G, Wang TAO, Wang T et al (2013) Effects of apoptosis-related proteins caspase-3, Bax and Bcl-2 on cerebral ischemia rats. Biomed Rep 1(6):861–867. https://doi.org/10.3892/br.2013.153
Popp A, Jaenisch N, Witte OW, Frahm C (2009) Identification of ischemic regions in a rat model of stroke. PLoS ONE 4:e4764. https://doi.org/10.1371/journal.pone.0004764
Kiewert C, Mdzinarishvili A, Hartmann J et al (2010) Metabolic and transmitter changes in core and penumbra after middle cerebral artery occlusion in mice. Brain Res 1312:101–107. https://doi.org/10.1016/j.brainres.2009.11.068
Zhang P, Zhang Y, Zhang J et al (2013) Early exercise protects against cerebral ischemic injury through inhibiting neuron apoptosis in cortex in rats. Int J Mol Sci 14:6074–6089. https://doi.org/10.3390/ijms14036074
Wu M, Zhang H, Kai J et al (2018) Rapamycin prevents cerebral stroke by modulating apoptosis and autophagy in penumbra in rats. Ann Clin Transl Neurol 5:138–146. https://doi.org/10.1002/acn3.507
Yu J, Li X, Matei N et al (2018) Ezetimibe, a NPC1L1 inhibitor, attenuates neuronal apoptosis through AMPK dependent autophagy activation after MCAO in rats. Exp Neurol 307:12–23. https://doi.org/10.1016/j.expneurol.2018.05.022
Shen Z, Zheng Y, Wu J et al (2017) PARK2-dependent mitophagy induced by acidic postconditioning protects against focal cerebral ischemia and extends the reperfusion window. Autophagy 13:473–485. https://doi.org/10.1080/15548627.2016.1274596
Zhang Y, Fang M, Sun Y et al (2018) Curcumin attenuates cerebral ischemia injury in Sprague-Dawley rats and PC12 cells by suppressing overactivated autophagy. J Photochem Photobiol B Biol 184:1–6. https://doi.org/10.1016/j.jphotobiol.2018.05.010
Li Y, Zhang J, Chen L et al (2015) Ebselen reduces autophagic activation and cell death in the ipsilateral thalamus following focal cerebral infarction. Neurosci Lett 600:206–212. https://doi.org/10.1016/j.neulet.2015.06.024
Wang R, Liu YY, Liu XY et al (2014) Resveratrol protects neurons and the myocardium by reducing oxidative stress and ameliorating mitochondria damage in a cerebral ischemia rat model. Cell Physiol Biochem 34:854–864. https://doi.org/10.1159/000366304
Zhao G, Zhang W, Li L et al (2014) Pinocembrin protects the brain against ischemia-reperfusion injury and reverses the autophagy dysfunction in the penumbra area. Molecules 19:15786–15798. https://doi.org/10.3390/molecules191015786
Yu J, Wang WN, Matei N et al (2020) Ezetimibe attenuates oxidative stress and neuroinflammation via the AMPK/Nrf2/TXNIP pathway after MCAO in rats. Oxid Med Cell Longev 2020:14. https://doi.org/10.1155/2020/4717258
Funding
The authors are thankful to the Science and Engineering Research Board—Department of Science and Technology (SERB—DST), Government of India, for funding this experimental study on safinamide (EMR/2017/004167).
Author information
Authors and Affiliations
Contributions
HW and KHR conceptualized and designed the study. HW and DS prepared the manuscript. HW, DS, and BJ conducted all the experiments, reported, and analysed the results. US helped in conducting MRI experiments and AKD helped in immunofluorescence study. KHR supervised and guided in all experimental work from designing the study to analysis of results.
Corresponding author
Ethics declarations
Ethics Approval
This study was approved by Institutional Animal Ethics Committee of All India Institute of Medical Sciences, New Delhi, India (File No. 21/IAEC-1/2017).
Consent to Participate
NA.
Consent for Publication
NA.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wasan, H., Singh, D., Joshi, B. et al. Post Stroke Safinamide Treatment Attenuates Neurological Damage by Modulating Autophagy and Apoptosis in Experimental Model of Stroke in Rats. Mol Neurobiol 58, 6121–6135 (2021). https://doi.org/10.1007/s12035-021-02523-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-021-02523-6