Abstract
Background
Arsenic is a natural element which exists in the environment in inorganic and organic forms. In humans, the main reason for the toxicity of arsenic is its uptake via water sources. As polluted water and the problems associated with it can be found in many countries. Therefore, considering all these positive effects of melatonin, this review is aimed at melatonin supplementation therapy on arsenic toxicity which seems to be a suitable therapeutic agent to eliminate the adverse effects of arsenic.
Methods and Results
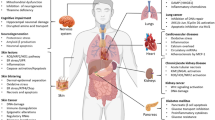
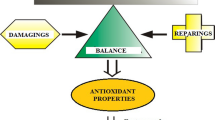
It is seen in previous studies that chronic exposure to arsenic could cause serious dys functions of organs and induce different degrees of toxicities that is one of the first hazardous materials in the classification of substances by the United States Environmental Protection Agency so leads to costly cleanup operations burdening the economy. Arsenic harmfulness degree depends on the bioavailability, chemical form, valence state, detoxification, and metabolism of human body. The oxidative stress has a major role in arsenic-induced toxicity; on the other hand, it was discovered that melatonin is a powerful scavenger for free radical and it’s an extensive-spectrum antioxidant.
Conclusion
Due to its highly lipophilic and small size properties, melatonin accesses all intracellular organs by easily passing via the cell membrane and prevents protein, DNA damage, and lipid peroxidation. In particular, melatonin, by protecting and reducing oxidative stress in mitochondria, can normalize homeostasis and mitochondrial function and ultimately prevent apoptosis and cell death.



Similar content being viewed by others
Abbreviations
- ROS:
-
Reactive oxygen species
- AS:
-
Arsenic
- H2O2:
-
Hydrogen peroxide
- NO:
-
Nitric oxide
- HO− :
-
Hydroxyl radical’s species
- O2:
-
Superoxide anion
- (CH3)2As:
-
Dimethyl arsenic radical
- (CH3)2Asoo:
-
Dimethyl arsenic peroxyl radical
- OhdG:
-
8-Hydroxy-2′-deoxyguanosine
- SCE:
-
Sister chromatid exchanges
- SCEs:
-
Sister chromatid exchanges
- Cas:
-
Chromosomal aberrations
- COX-2:
-
Cyclooxygenase-2
- MAPK:
-
Mitogen-activated protein kinases
- IL-6:
-
Interleukin 6
- TNF-α:
-
Tumor necrosis factor
- ATO:
-
Arsenic trioxide
- CAT:
-
Catalase
- GPx:
-
Glutathione peroxidase
- UROШ-s:
-
Uroporphyrinogen III synthetase
- PBG-D:
-
Porphobilinogen deaminase
- Aβ:
-
Amyloid-β
- NMDA:
-
N-methyl-d-aspartate receptor
- CKD:
-
Chronic kidney disease
- COPD:
-
Chronic obstructive pulmonary disease
- AR:
-
Androgen receptor
- MTBS:
-
Mean testicular biopsy score
- MSTD:
-
Mean seminiferous tubular diameter
- VSMCs:
-
Vascular smooth muscle cells
- MLCK:
-
Myosin light chain kinase
- IRI:
-
Ischemia/reperfusion injury
- GERD:
-
Gastroesophageal reflux disease
- MMP-2:
-
Matrix metalloproteinase-2
- GHS:
-
Global hepatitis summit
References
Jomova K, Jenisova Z, Feszterova M, Baros S, Liska J, Hudecova D et al (2011) Arsenic: toxicity, oxidative stress and human disease. J Appl Toxicol 31(2):95–107
Xu M, Niu Q, Hu Y, Feng G, Wang H, Li S (2019) Proanthocyanidins antagonize arsenic-induced oxidative damage and promote arsenic methylation through activation of the Nrf2 signaling pathway. Oxid Med Cell Longev 2019:8549035
WHO (2017) Global status report on water safety plans: a review of proactive risk assessment and risk management practices to ensure the safety of drinking-water. World Health Organization
Uygur R, Aktas C, Caglar V, Uygur E, Erdogan H, Ozen OA (2016) Protective effects of melatonin against arsenic-induced apoptosis and oxidative stress in rat testes. Toxicol Ind Health 32(5):848–859
Ali SS, Medda N, Dutta SM, Patra R, Maiti S (2020) Protection against mitochondrial oxidative-stress by flesh-extract of edible freshwater snail bellamya bengalensis prevents arsenic induced DNA and tissue damage. Anti Cancer Agents Med 20(10):1266–1273
Flora S, Bhadauria S, Kannan G, Singh N (2007) Arsenic induced oxidative stress and the role of antioxidant supplementation during chelation: a review. J Environ Biol 28(2):333
Yun S-M, Woo SH, Oh ST, Hong S-E, Choe T-B, Ye S-K et al (2016) Melatonin enhances arsenic trioxide-induced cell death via sustained upregulation of Redd1 expression in breast cancer cells. Mol Cell Endocrinol 422:64–73
Pal S, Pal PB, Das J, Sil PC (2011) Involvement of both intrinsic and extrinsic pathways in hepatoprotection of arjunolic acid against cadmium induced acute damage in vitro. Toxicology 283(2–3):129–139
Stehle JH, Saade A, Rawashdeh O, Ackermann K, Jilg A, Sebestény T et al (2011) A survey of molecular details in the human pineal gland in the light of phylogeny, structure, function and chronobiological diseases. J Pineal Res 51(1):17–43
Acuña-Castroviejo D, Escames G, Venegas C, Díaz-Casado ME, Lima-Cabello E, López LC et al (2014) Extrapineal melatonin: sources, regulation, and potential functions. Cell Mol Life Sci 71(16):2997–3025
Renzi A, DeMorrow S, Onori P, Carpino G, Mancinelli R, Meng F et al (2013) Modulation of the biliary expression of arylalkylamine N-acetyltransferase alters the autocrine proliferative responses of cholangiocytes in rats. Hepatology 57(3):1130–1141
Wu N, Meng F, Zhou T, Han Y, Kennedy L, Venter J et al (2017) Prolonged darkness reduces liver fibrosis in a mouse model of primary sclerosing cholangitis by miR-200b down-regulation. FASEB J 31(10):4305–4324
Amaral FGD, Andrade-Silva J, Kuwabara WM, Cipolla-Neto J (2019) New insights into the function of melatonin and its role in metabolic disturbances. Expert Rev Endocrinol Metab 14(4):293–300
Xalxo R, Keshavkant S (2019) Melatonin, glutathione and thiourea attenuates lead and acid rain-induced deleterious responses by regulating gene expression of antioxidants in Trigonella foenum graecum L.. Chemosphere 221:1–10
Mohamed EA (2015) The protective effect of melatonin vs. vitamin e in the ischemic/reperfused skeletal muscle in the adult male rat model. J Cytol Histol 3(3):1
Shaker M, Houssen M, Abo-Hashem E, Ibrahim T (2009) Comparison of vitamin E, L-carnitine and melatonin in ameliorating carbon tetrachloride and diabetes induced hepatic oxidative stress. J Physiol Biochem 65(3):225–233
Claustrat B, Leston J (2015) Melatonin: physiological effects in humans. Neurochirurgie 61(2–3):77–84
Wang H, Xi S, Xu Y, Wang F, Zheng Y, Li B et al (2013) Sodium arsenite induces cyclooxygenase-2 expression in human uroepithelial cells through MAPK pathway activation and reactive oxygen species induction. Toxicol In Vitro 27(3):1043–1048
Noman ASM, Dilruba S, Mohanto NC, Rahman L, Khatun Z, Riad W et al (2015) Arsenic-induced histological alterations in various organs of mice. J Cytol Histol 6(3):323
Phaniendra A, Jestadi DB, Periyasamy L (2015) Free radicals: properties, sources, targets, and their implication in various diseases. Indian J Clin Biochem 30(1):11–26
Farkhondeh T, Samarghandian S, Azimi-Nezhad M (2019) The role of arsenic in obesity and diabetes. J Cell Physiol 234(8):12516–12529
Zaazaa AM (2014) Protective role of the nigella sativa oil against arsenic-induced neurotoxicity in male rats. World J Pharm Res 3(2):1624–1636
Greani S, Lourkisti R, Berti L, Marchand B, Giannettini J, Santini J et al (2017) Effect of chronic arsenic exposure under environmental conditions on bioaccumulation, oxidative stress, and antioxidant enzymatic defenses in wild trout Salmo trutta (Pisces, Teleostei). Ecotoxicology 26(7):930–941
Bau D-T, Wang T-S, Chung C-H, Wang AS, Wang AS, Jan K-Y (2002) Oxidative DNA adducts and DNA-protein cross-links are the major DNA lesions induced by arsenite. Environ Health Perspect 110(suppl 5):753–756
Wu C-Y, Wong C-S, Chung C-J, Wu M-Y, Huang Y-L, Ao P-L et al (2019) The association between plasma selenium and chronic kidney disease related to lead, cadmium and arsenic exposure in a Taiwanese population. J Hazard Mater 375:224–232
Mishra D, Flora S (2008) Differential oxidative stress and DNA damage in rat brain regions and blood following chronic arsenic exposure. Toxicol Ind Health 24(4):247–256
He Y, Zhang R, Chen J, Tan J, Wang M, Wu X (2020) The ability of arsenic metabolism affected the expression of lncRNA PANDAR, DNA damage, or DNA methylation in peripheral blood lymphocytes of laborers. Hum Exp Toxicol 39(5):605–613
Roy JS, Chatterjee D, Das N, Giri AK (2018) Substantial evidences indicate that inorganic arsenic is a genotoxic carcinogen: a review. Toxicological research 34(4):311–324
Vijayakaran K, Kannan K, Kesavan M, Suresh S, Sankar P, Tandan SK et al (2014) Arsenic reduces the antipyretic activity of paracetamol in rats: modulation of brain COX-2 activity and CB1 receptor expression. Environ Toxicol Pharmacol 37(1):438–447
Gong X, Ivanov VN, Hei TK (2016) 2, 3, 5, 6-Tetramethylpyrazine (TMP) down-regulated arsenic-induced heme oxygenase-1 and ARS2 expression by inhibiting Nrf2, NF-κB, AP-1 and MAPK pathways in human proximal tubular cells. Arch Toxicol 90(9):2187–2200
Escudero-Lourdes C, Medeiros M, Cárdenas-González M, Wnek S, Gandolfi J (2010) Low level exposure to monomethyl arsonous acid-induced the over-production of inflammation-related cytokines and the activation of cell signals associated with tumor progression in a urothelial cell model. Toxicol Appl Pharmacol 244(2):162–173
Wadgaonkar P, Chen F (2021) Connections between endoplasmic reticulum stress-associated unfolded protein response, mitochondria, and autophagy in arsenic-induced carcinogenesis. Seminars in cancer biology. Elsevier
Kim Y-J, Chung J-Y, Lee SG, Kim JY, Park J-E, Kim WR et al (2011) Arsenic trioxide-induced apoptosis in TM4 Sertoli cells: the potential involvement of p21 expression and p53 phosphorylation. Toxicology 285(3):142–151
Das J, Ghosh J, Manna P, Sinha M, Sil PC (2009) Taurine protects rat testes against NaAsO2-induced oxidative stress and apoptosis via mitochondrial dependent and independent pathways. Toxicol Lett 187(3):201–210
Flora S, Mittal M, Mehta A (2008) Heavy metal induced oxidative stress and its possible reversal by chelation therapy. Indian J Med Res 128(4):501
Sayyadi M, Safaroghli-Azar A, Pourbagheri-Sigaroodi A, Abolghasemi H, Anoushirvani AA, Bashash D (2020) c-Myc inhibition using 10058–F4 increased the sensitivity of acute promyelocytic leukemia cells to arsenic trioxide via blunting PI3K/NF-κB axis. Arch Med Res 51(7):636–644
Alarifi S, Ali D, Alkahtani S, Siddiqui MA, Ali BA (2013) Arsenic trioxide-mediated oxidative stress and genotoxicity in human hepatocellular carcinoma cells. Onco Targets Ther 6:75
Kasukabe T, Okabe-Kado J, Haranosono Y, Kato N, Honma Y (2013) Inhibition of rapamycin-induced Akt phosphorylation by cotylenin A correlates with their synergistic growth inhibition of cancer cells. Int J Oncol 42(2):767–775
Chen C, Jiang X, Hu Y, Zhang Z (2013) The protective role of resveratrol in the sodium arsenite-induced oxidative damage via modulation of intracellular GSH homeostasis. Biol Trace Elem Res 155(1):119–131
Söderquist F, Hellström PM, Cunningham JL (2015) Human gastroenteropancreatic expression of melatonin and its receptors MT1 and MT2. PLoS ONE 10(3):e0120195
Valavanidis A, Vlachogianni T, Fiotakis K (2009) Tobacco smoke: involvement of reactive oxygen species and stable free radicals in mechanisms of oxidative damage, carcinogenesis and synergistic effects with other respirable particles. Int J Environ Res Public Health 6(2):445–462
Reiter RJ, Mayo JC, Tan DX, Sainz RM, Alatorre-Jimenez M, Qin L (2016) Melatonin as an antioxidant: under promises but over delivers. J Pineal Res 61(3):253–278
Farouk S, Al-Amri SM (2019) Exogenous melatonin-mediated modulation of arsenic tolerance with improved accretion of secondary metabolite production, activating antioxidant capacity and improved chloroplast ultrastructure in rosemary herb. Ecotoxicol Environ Saf 180:333–347
Kitchin KT, Conolly R (2009) Arsenic-induced carcinogenesis oxidative stress as a possible mode of action and future research needs for more biologically based risk assessment. Chem Res Toxicol 23(2):327–335
Zhang Y, Kim MS, Jia B, Yan J, Zuniga-Hertz JP, Han C et al (2017) Hypothalamic stem cells control ageing speed partly through exosomal miRNAs. Nature 548(7665):52
Khairul I, Wang QQ, Jiang YH, Wang C, Naranmandura H (2017) Metabolism, toxicity and anticancer activities of arsenic compounds. Oncotarget 8(14):23905
Hirano S, Cui X, Li S, Kanno S, Kobayashi Y, Hayakawa T et al (2003) Difference in uptake and toxicity of trivalent and pentavalent inorganic arsenic in rat heart microvessel endothelial cells. Arch Toxicol 77(6):305–312
Vahter M, Concha G (2001) Role of metabolism in arsenic toxicity. Pharmacol Toxicol Mini Rev 89(1):1–5
Aposhian HV, Zakharyan RA, Avram MD, Sampayo-Reyes A, Wollenberg ML (2004) A review of the enzymology of arsenic metabolism and a new potential role of hydrogen peroxide in the detoxication of the trivalent arsenic species. Toxicol Appl Pharmacol 198(3):327–335
Goering PL, Aposhian HV, Mass MJ, Cebrián M, Beck BD, Waalkes MP (1999) The enigma of arsenic carcinogenesis: role of metabolism. Toxicol Sci Off J Soc Toxicol 49(1):5–14
Hacışevki A, Baba B (2018) An overview of melatonin as an antioxidant molecule: a biochemical approach. Melatonin Mol Biol Clin Pharm Approach 2018:59–85
Galano A, Tan D-X, Reiter RJ (2018) Melatonin: a versatile protector against oxidative DNA damage. Molecules 23(3):530
Catala A (2007) The ability of melatonin to counteract lipid peroxidation in biological membranes. Curr Mol Med 7(7):638–649
Tomás-Zapico C, Coto-Montes A (2005) A proposed mechanism to explain the stimulatory effect of melatonin on antioxidative enzymes. J Pineal Res 39(2):99–104
Yin J, Liu YH, Xu YF, Zhang YJ, Chen JG, Shu BH et al (2006) Melatonin arrests peroxynitrite-induced tau hyperphosphorylation and the overactivation of protein kinases in rat brain. J Pineal Res 41(2):124–129
Manchester LC, Coto-Montes A, Boga JA, Andersen LPH, Zhou Z, Galano A et al (2015) Melatonin: an ancient molecule that makes oxygen metabolically tolerable. J Pineal Res 59(4):403–419
Xu S, Pi H, Zhang L, Zhang N, Li Y, Zhang H et al (2016) Melatonin prevents abnormal mitochondrial dynamics resulting from the neurotoxicity of cadmium by blocking calcium-dependent translocation of Drp1 to the mitochondria. J Pineal Res 60(3):291–302
Li M, Pi H, Yang Z, Reiter RJ, Xu S, Chen X et al (2016) Melatonin antagonizes cadmium-induced neurotoxicity by activating the transcription factor EB-dependent autophagy–lysosome machinery in mouse neuroblastoma cells. J Pineal Res 61(3):353–369
García JJ, López-Pingarrón L, Almeida-Souza P, Tres A, Escudero P, García-Gil FA et al (2014) Protective effects of melatonin in reducing oxidative stress and in preserving the fluidity of biological membranes: a review. J Pineal Res 56(3):225–237
Prado NJ, Ferder L, Manucha W, Diez ER (2018) Anti-inflammatory effects of melatonin in obesity and hypertension. Curr Hypertens Rep 20(5):1–12
Romero A, Ramos E, de Los RC, Egea J, Del Pino J, Reiter RJ (2014) A review of metal-catalyzed molecular damage: protection by melatonin. J Pineal Res 56(4):343–370
Majidinia M, Sadeghpour A, Mehrzadi S, Reiter RJ, Khatami N, Yousefi B (2017) Melatonin: a pleiotropic molecule that modulates DNA damage response and repair pathways. J Pineal Res 63(1):e012416
Hu Y, Li J, Lou B, Wu R, Wang G, Lu C et al (2020) The role of reactive oxygen species in arsenic toxicity. Biomolecules 10(2):240
Pant HH, Rao MV (2010) Evaluation of in vitro anti-genotoxic potential of melatonin against arsenic and fluoride in human blood cultures. Ecotoxicol Environ Saf 73(6):1333–1337
Carrascal L, Nunez-Abades P, Ayala A, Cano M (2018) Role of melatonin in the inflammatory process and its therapeutic potential. Curr Pharm Des 24(14):1563–1588
Jain A, Mehta VK, Chittora R, Mahdi A, Bhatnagar M (2015) Melatonin ameliorates fluoride induced neurotoxicity in young rats: an in vivo evidence. Asian J Pharm Clin Res 8(4):164–167
Xia MZ, Liang YL, Wang H, Chen X, Huang YY, Zhang ZH et al (2012) Melatonin modulates TLR4-mediated inflammatory genes through MyD88-and TRIF-dependent signaling pathways in lipopolysaccharide-stimulated RAW264. 7 cells. J Pineal Res 53(4):325–334
Liu X, Piao F, Li Y (2013) Protective effect of taurine on the decreased biogenic amine neurotransmitter levels in the brain of mice exposed to arsenic. Taurine 8:277–287
Bernardini L, Barbosa E, Charão MF, Goethel G, Muller D, Bau C et al (2020) Oxidative damage, inflammation, genotoxic effect, and global DNA methylation caused by inhalation of formaldehyde and the purpose of melatonin. Toxicol Res 9(6):778–789
Lowes D, Almawash A, Webster N, Reid V, Galley H (2011) Melatonin and structurally similar compounds have differing effects on inflammation and mitochondrial function in endothelial cells under conditions mimicking sepsis. Br J Anaesth 107(2):193–201
Hajam YA, Rai S (2019) Melatonin and insulin modulates the cellular biochemistry, histoarchitecture and receptor expression during hepatic injury in diabetic rats. Life Sci 239:117046
Bharti VK, Srivastava R, Sharma B, Malik J (2012) Buffalo (Bubalus bubalis) epiphyseal proteins counteract arsenic-induced oxidative stress in brain, heart, and liver of female rats. Biol Trace Elem Res 146(2):224–229
Song J, Kang SM, Lee KM, Lee JE (2015) The protective effect of melatonin on neural stem cell against LPS-induced inflammation. BioMed Res Inter. https://doi.org/10.1155/2015/854359
Abdul KSM, Jayasinghe SS, Chandana EP, Jayasumana C, De Silva PMC (2015) Arsenic and human health effects: a review. Environ Toxicol Pharmacol 40(3):828–846
Valles S, Hernández-Sánchez J, Dipp VR, Huerta-González D, Olivares-Bañuelos TN, González-Fraga J et al (2020) Exposure to low doses of inorganic arsenic induces transgenerational changes on behavioral and epigenetic markers in zebrafish (Danio rerio). Toxicol Appl Pharmacol 396:115002
Firdaus F, Zafeer MF, Ahmad M, Afzal M (2018) Anxiolytic and anti-inflammatory role of thymoquinone in arsenic-induced hippocampal toxicity in Wistar rats. Heliyon 4(6):e00650
Olson KR, Anderson IB, Benowitz NL, Blanc PD, Clark RF, Kearney TE et al (2007) Poisoning and drug overdose. McGraw-Hill, NewYork
Zhang Y, Wei Z, Liu W, Wang J, He X, Huang H et al (2017) Melatonin protects against arsenic trioxide-induced liver injury by the upregulation of Nrf2 expression through the activation of PI3K/AKT pathway. Oncotarget 8(3):3773
Dwivedi N, Mehta A, Yadav A, Binukumar B, Gill KD, Flora SJ (2011) MiADMSA reverses impaired mitochondrial energy metabolism and neuronal apoptotic cell death after arsenic exposure in rats. Toxicol Appl Pharmacol 256(3):241–248
Kim KB, Bedikian AY, Camacho LH, Papadopoulos NE, McCullough C (2005) A phase II trial of arsenic trioxide in patients with metastatic melanoma. Cancer 104(8):1687–1692
Rios R, Zarazúa S, Santoyo M, Sepúlveda-Saavedra J, Romero-Díaz V, Jimenez V et al (2009) Decreased nitric oxide markers and morphological changes in the brain of arsenic-exposed rats. Toxicology 261(1–2):68–75
Samad N, Rao T, Rehman MH, Bhatti SA, Imran I (2021) Inhibitory effects of selenium on arsenic-induced anxiety-/depression-like behavior and memory impairment. Biol Trace Element Res. https://doi.org/10.1007/s12011-021-02679-1
Vahidnia A, Romijn F, Van der Voet G, De Wolff F (2008) Arsenic-induced neurotoxicity in relation to toxicokinetics: effects on sciatic nerve proteins. Chem Biol Interact 176(2–3):188–195
Liu S, Piao F, Sun X, Bai L, Peng Y, Zhong Y et al (2012) Arsenic-induced inhibition of hippocampal neurogenesis and its reversibility. Neurotoxicology 33(5):1033–1039
Singh AP, Goel RK, Kaur T (2011) Mechanisms pertaining to arsenic toxicity. Toxicol Int 18(2):87
Chandravanshi LP, Gupta R, Shukla RK (2019) Arsenic-induced neurotoxicity by dysfunctioning cholinergic and dopaminergic system in brain of developing rats. Biol Trace Elem Res 189(1):118–133
Krüger K, Straub H, Hirner AV, Hippler J, Binding N, Muβhoff U (2009) Effects of monomethylarsonic and monomethylarsonous acid on evoked synaptic potentials in hippocampal slices of adult and young rats. Toxicol Appl Pharmacol 236(1):115–123
Felix K, Manna SK, Wise K, Barr J, Ramesh GT (2005) Low levels of arsenite activates nuclear factor-κB and activator protein-1 in immortalized mesencephalic cells. J Biochem Mol Toxicol 19(2):67–77
Flora SJ (2011) Arsenic-induced oxidative stress and its reversibility. Free Radical Biol Med 51(2):257–281
Durappanavar PN, Nadoor P, Waghe P, Pavithra B, Jayaramu G (2019) Melatonin ameliorates neuropharmacological and neurobiochemical alterations induced by subchronic exposure to arsenic in Wistar rats. Biol Trace Elem Res 190(1):124–139
Kalonia H, Kumar A (2007) Protective effect of melatonin on certain behavioral and biochemical alterations induced by sleep-deprivation in mice. Indian J Pharmacol 39(1):48
Fan SF, Chao PL, Lin AMY (2010) Arsenite induces oxidative injury in rat brain: synergistic effect of iron. Ann N Y Acad Sci 1199(1):27–35
Raju V, Bell JJ, Merlin N, Dharan SS (2017) Anxiety disorders-a review. Asian J Pharm Res 7(4):217
Rao MV, Purohit AR (2011) Neuroprotection by melatonin on mercury induced toxicity in the rat brain. Pharmacol Pharm 2(04):375
Huang C-C, Lai C-J, Tsai M-H, Wu Y-C, Chen K-T, Jou M-J et al (2015) Effects of melatonin on the nitric oxide system and protein nitration in the hypobaric hypoxic rat hippocampus. BMC Neurosci 16(1):61
Deng Y, Jiao C, Mi C, Xu B, Li Y, Wang F et al (2015) Melatonin inhibits manganese-induced motor dysfunction and neuronal loss in mice: involvement of oxidative stress and dopaminergic neurodegeneration. Mol Neurobiol 51(1):68–88
Meliker JR, Wahl RL, Cameron LL, Nriagu JO (2007) Arsenic in drinking water and cerebrovascular disease, diabetes mellitus, and kidney disease in Michigan: a standardized mortality ratio analysis. Environ Health 6(1):4
Kayankarnna W, Tangvarasittichai O, Tangvarasittichai S (2016) Association between elevated arsenic exposure with chronic kidney disease and oxidative stress in subjects of the contamination area. Int J Toxicol Pharm Res 8(3):173–178
Dutta S, Saha S, Mahalanobish S, Sadhukhan P, Sil PC (2018) Melatonin attenuates arsenic induced nephropathy via the regulation of oxidative stress and inflammatory signaling cascades in mice. Food Chem Toxicol 118:303–316
Yu M, Xue J, Li Y, Zhang W, Ma D, Liu L et al (2013) Resveratrol protects against arsenic trioxide-induced nephrotoxicity by facilitating arsenic metabolism and decreasing oxidative stress. Arch Toxicol 87(6):1025–1035
Mahalanobish S, Saha S, Dutta S, Sil PC (2019) Mangiferin alleviates arsenic induced oxidative lung injury via upregulation of the Nrf2-HO1 axis. Food Chem Toxicol 126:41–55
Singh SS, Deb A, Sutradhar S (2019) Effect of melatonin on arsenic-induced oxidative stress and expression of MT1 and MT2 receptors in the kidney of laboratory mice. Biol Rhythm Res 51:1216–1230
Sabir S, Akash MSH, Fiayyaz F, Saleem U, Mehmood MH, Rehman K (2019) Role of cadmium and arsenic as endocrine disruptors in the metabolism of carbohydrates: inserting the association into perspectives. Biomed Pharmacother 114:108802
Cifuentes F, Bravo J, Norambuena M, Stegen S, Ayavire A, Palacios J (2009) Chronic exposure to arsenic in tap water reduces acetylcholine-induced relaxation in the aorta and increases oxidative stress in female rats. Int J Toxicol 28(6):534–541
Huang C-F, Yang C-Y, Chan D-C, Wang C-C, Huang K-H, Wu C-C et al (2015) Arsenic exposure and glucose intolerance/insulin resistance in estrogen-deficient female mice. Environ Health Perspect 123(11):1138–1144
Das S, Santra A, Lahiri S, Mazumder DG (2005) Implications of oxidative stress and hepatic cytokine (TNF-α and IL-6) response in the pathogenesis of hepatic collagenesis in chronic arsenic toxicity. Toxicol Appl Pharmacol 204(1):18–26
Tao Y, Qiu T, Yao X, Jiang L, Wang N, Jia X et al (2020) Autophagic-CTSB-inflammasome axis modulates hepatic stellate cells activation in arsenic-induced liver fibrosis. Chemosphere 242:124959
Kokilavani V, Devi MA, Sivarajan K, Panneerselvam C (2005) Combined efficacies of dl-α-lipoic acid and meso 2, 3 dimercaptosuccinic acid against arsenic induced toxicity in antioxidant systems of rats. Toxicol Lett 160(1):1–7
Pal S, Chatterjee AK (2006) Possible beneficial effects of melatonin supplementation on arsenic-induced oxidative stress in Wistar rats. Drug Chem Toxicol 29(4):423–433
Mortezaee K (2018) Human hepatocellular carcinoma: protection by melatonin. J Cell Physiol 233(10):6486–6508
Hemmati AA, Alboghobeish S, Ahangarpour A (2018) Chronic exposure to high fat diet exacerbates arsenic-induced lung damages in male mice: possible role for oxidative stress. Monaldi Arch Chest Dis, 88(1)
Shin IS, Shin NR, Park JW, Jeon CM, Hong JM, Kwon OK et al (2015) Melatonin attenuates neutrophil inflammation and mucus secretion in cigarette smoke-induced chronic obstructive pulmonary diseases via the suppression of Erk-Sp1 signaling. J Pineal Res 58(1):50–60
Pourgholamhossein F, Rasooli R, Pournamdari M, Pourgholi L, Samareh-Fekri M, Ghazi-Khansari M et al (2018) Pirfenidone protects against paraquat-induced lung injury and fibrosis in mice by modulation of inflammation, oxidative stress, and gene expression. Food Chem Toxicol 112:39–46
Ahmad I, Akthar KM, Hussain T (2008) Arsenic induced microscopic changes in rat testis. Prof Med J 15(02):287–291
Darbandi M, Darbandi S, Agarwal A, Sengupta P, Durairajanayagam D, Henkel R et al (2018) Reactive oxygen species and male reproductive hormones. Reprod Biol Endocrinol 16(1):1–14
Bustos-Obregón E, Poblete D, Catriao R, Fernandes FH (2013) Protective role of melatonin in mouse spermatogenesis induced by sodium arsenite. Inter J Morphol 2013:849–856
Ferreira M, Matos RC, Oliveira H, Nunes B, Pereira MDL (2012) Impairment of mice spermatogenesis by sodium arsenite. Human Exp Toxicol 31(3):290–302
da Silva RF, Borges CDS, de Almeida LC, Cagnon VHA, de Grava Kempinas W (2017) Arsenic trioxide exposure impairs testicular morphology in adult male mice and consequent fetus viability. J Toxicol Environ Health Part A 80(19–21):1166–1179
Orta Yilmaz B, Yildizbayrak N, Erkan M (2020) Sodium arsenite-induced detriment of cell function in Leydig and Sertoli cells: the potential relation of oxidative damage and antioxidant defense system. Drug Chem Toxicol 43(5):479–487
Tamura H, Takasaki A, Taketani T, Tanabe M, Lee L, Tamura I et al (2014) Melatonin and female reproduction. J Obstet Gynaecol Res 40(1):1–11
Reiter RJ, Tan D-X, Manchester LC, Paredes SD, Mayo JC, Sainz RM (2009) Melatonin and reproduction revisited. Biol Reprod 81(3):445–456
Cipolla-Neto J, Amaral FG, Soares-Jr JM, Gallo CC, Furtado A, Cavaco JE et al (2021) The crosstalk between melatonin and sex steroid hormones. Neuroendocrinology. https://doi.org/10.1159/000516148
Zhai M, Li B, Duan W, Jing L, Zhang B, Zhang M et al (2017) Melatonin ameliorates myocardial ischemia reperfusion injury through SIRT 3-dependent regulation of oxidative stress and apoptosis. J Pineal Res 63(2):e12419
Ferreira CS, Carvalho KC, Maganhin CC, Paiotti AP, Oshima CT, Simões MJ et al (2016) Does melatonin influence the apoptosis in rat uterus of animals exposed to continuous light? Apoptosis 21(2):155–162
Stea F, Bianchi F, Cori L, Sicari R (2014) Cardiovascular effects of arsenic: clinical and epidemiological findings. Environ Sci Pollut Res 21(1):244–251
Binu P, Gifty K, Vineetha R, Abhilash S, Arathi P, Nair RH (2018) Eugenol, a plant-derived phenolic nutraceutical, protects thiol (SH) group in myocardium from ROS-mediated oxidation under chemotherapeutic stress induced by arsenic trioxide–a in vivo model study. Drug Chem Toxicol 41(3):352–357
Lee P-C, Ho I-C, Lee T-C (2005) Oxidative stress mediates sodium arsenite-induced expression of heme oxygenase-1, monocyte chemoattractant protein-1, and interleukin-6 in vascular smooth muscle cells. Toxicol Sci 85(1):541–550
Pysher MD, Chen QM, Vaillancourt RR (2008) Arsenic alters vascular smooth muscle cell focal adhesion complexes leading to activation of FAK–src mediated pathways. Toxicol Appl Pharmacol 231(2):135–141
Balakumar P, Kaur J (2009) Arsenic exposure and cardiovascular disorders: an overview. Cardiovasc Toxicol 9(4):169–176
States JC, Srivastava S, Chen Y, Barchowsky A (2008) Arsenic and cardiovascular disease. Toxicol Sci 107(2):312–323
Vineetha VP, Raghu KG (2019) An overview on arsenic trioxide-induced cardiotoxicity. Cardiovasc Toxicol 19(2):105–119
Veenema R, Casin KM, Sinha P, Kabir R, Mackowski N, Taube N et al (2019) Signaling and stress response: inorganic arsenic exposure induces sex-disparate effects and exacerbates ischemia-reperfusion injury in the female heart. Am J Physiol Heart Circ Physiol 316(5):H1053
Ma Z, Xin Z, Di W, Yan X, Li X, Reiter RJ et al (2017) Melatonin and mitochondrial function during ischemia/reperfusion injury. Cell Mol Life Sci 74(21):3989–3998
Sun Y, Tokar EJ, Waalkes MP (2012) Overabundance of putative cancer stem cells in human skin keratinocyte cells malignantly transformed by arsenic. Toxicol Sci 125(1):20–29
Zeng Q, Zhang A (2020) Assessing potential mechanisms of arsenic-induced skin lesions and cancers: human and in vitro evidence. Environ Pollut 260:113919
Pathania YS (2020) Mottled pigmentation, palmar keratosis and chronic arsenic poisoning. QJM Inter J Med 114:265–266
Raman SKVRK, Bhowmick ATAKS, Bimal SKMSS, Mohanty P (2020) Clinico-epidemiological study of arsenicosis in arsenic endemic areas of West Bengal, India
Bjørklund G, Oliinyk P, Lysiuk R, Rahaman MS, Antonyak H, Lozynska I et al (2020) Arsenic intoxication: general aspects and chelating agents. Arch Toxicol 94:1879–1897
Yu H, Liao W, Chai C (2006) Arsenic carcinogenesis in the skin. J Biomed Sci 13(5):657–666
Tsai T-L, Kuo C-C, Hsu L-I, Tsai S-F, Chiou H-Y, Chen C-J et al (2021) Association between arsenic exposure, DNA damage, and urological cancers incidence: a long-term follow-up study of residents in an arseniasis endemic area of northeastern Taiwan. Chemosphere 266:129094
Mehrandish R, Rahimian A, Shahriary A (2019) Heavy metals detoxification: a review of herbal compounds for chelation therapy in heavy metals toxicity. J Herbmed Pharmacol 8(2):69–77
Bhattacharjee B, Pal PK, Ghosh AK, Mishra S, Chattopadhyay A, Bandyopadhyay D (2019) Aqueous bark extract of Terminalia arjuna protects against cadmium-induced hepatic and cardiac injuries in male Wistar rats through antioxidative mechanisms. Food Chem Toxicol 124:249–264
Dorier M, Béal D, Marie-Desvergne C, Dubosson M, Barreau F, Houdeau E et al (2017) Continuous in vitro exposure of intestinal epithelial cells to E171 food additive causes oxidative stress, inducing oxidation of DNA bases but no endoplasmic reticulum stress. Nanotoxicology 11(6):751–761
Bhattacharyya A, Chattopadhyay R, Mitra S, Crowe SE (2014) Oxidative stress: an essential factor in the pathogenesis of gastrointestinal mucosal diseases. Physiol Rev 94(2):329–354
Contreras-Zentella ML, Olguín-Martínez M, Sánchez-Sevilla L, Hernández-Muñoz R (2017) Gastric mucosal injury and oxidative stress. Gastrointestinal Tissue. Elsevier, Netherlands, pp 65–79
Mitra E, Bhattacharjee B, Pal PK, Ghosh AK, Mishra S, Chattopadhyay A et al (2019) Melatonin protects against cadmium-induced oxidative damage in different tissues of rat: a mechanistic insight. Melatonin Res 2(2):1–21
Pal PK, Sarkar S, Chattopadhyay A, Tan DX, Bandyopadhyay D (2019) Enterochromaffin cells as the source of melatonin: key findings and functional relevance in mammals. Melatonin Res 2(4):61–82
Pal PK, Bhattacharjee B, Ghosh AK, Chattopadhyay A, Bandyopadhyay D (2018) Adrenaline induced disruption of endogenous melatoninergic system, antioxidant and inflammatory responses in the gastrointestinal tissues of male Wistar rat: an in vitro study. Melatonin Res 1(1):109–131
Konturek PC, Konturek SJ, Burnat G, Brzozowski T, Brzozowska I, Reiter RJ (2008) Dynamic physiological and molecular changes in gastric ulcer healing achieved by melatonin and its precursor L-tryptophan in rats. J Pineal Res 45(2):180–190
Carrillo-Vico A, Lardone PJ, Álvarez-Sánchez N, Rodríguez-Rodríguez A, Guerrero JM (2013) Melatonin: buffering the immune system. Int J Mol Sci 14(4):8638–8683
Trivedi P, Jena G (2013) Melatonin reduces ulcerative colitis-associated local and systemic damage in mice: investigation on possible mechanisms. Dig Dis Sci 58(12):3460–3474
Ma N, Zhang J, Reiter RJ, Ma X (2020) Melatonin mediates mucosal immune cells, microbial metabolism, and rhythm crosstalk: a therapeutic target to reduce intestinal inflammation. Med Res Rev 40(2):606–632
Gil-Martín E, Egea J, Reiter RJ, Romero A (2019) The emergence of melatonin in oncology: focus on colorectal cancer. Med Res Rev 39(6):2239–2285
Acknowledgements
The abstract of this article is submitted to the Third National Conference on Biotechnology Innovation and Technology, Iranian Chemistry (Abstract code: BC031576159).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abdollahzade, N., Majidinia, M. & Babri, S. Melatonin: a pleiotropic hormone as a novel potent therapeutic candidate in arsenic toxicity. Mol Biol Rep 48, 6603–6618 (2021). https://doi.org/10.1007/s11033-021-06669-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-021-06669-3