Abstract
Background
Laparoscopic surgery is commonly used in elderly patients over 80 years old. The purpose of this study was to compare the perioperative and oncologic outcomes between laparoscopic surgery and open surgery in elderly patients with colorectal cancer.
Methods
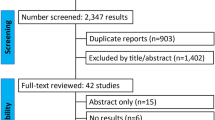
We retrospectively analyzed the medical records of patients aged ≥ 80 years who underwent curative resection of colorectal cancer at six Hallym University-affiliated hospitals. The perioperative outcomes and oncologic outcomes were compared between laparoscopic and open surgery
Results
Of 294 elderly patients, 104 (35.3%) underwent open surgery and 190 (64.7%) underwent laparoscopic surgery. The postoperative hospital stay (P = 0.019) and time to soft diet (P = 0.009) were shorter in the laparoscopic group than in the open group. Postoperative complications were less frequent in the laparoscopic group than in the open group (P < 0.001), including wound infection (P = 0.005), ileus (P = 0.005), and pneumonia (P = 0.001). The 3-year overall survival (OS) (P = 0.982) and recurrence-free survival rates (RFS) (P = 0.532) were similar in both groups. In multivariable analyses, positive lymph node status was the only independent factor associated with OS (P = 0.019) and RFS (P = 0.012). Laparoscopic surgery was not associated with OS (P = 0.874) and RFS (P = 0.772).
Conclusion
Laparoscopic surgery offers several perioperative advantages over open surgery and similar long-term oncological outcomes for elderly patients with colorectal cancer. Therefore, we suggest that laparoscopic surgery can be safely performed for the treatment of elderly patients (≥ 80 years old) with colorectal cancer.


Similar content being viewed by others
References
United Nations, Department of Economic and Social Affairs (2019) Population division. World Population Prospects, 2019
Tomimaru Y, Ide Y, Murata K (2011) Outcome of laparoscopic surgery for colon cancer in elderly patients. Asian J Endosc Surg 4(1):1–6
Senagore AJ, Madbouly KM, Fazio VW et al (2003) Advantages of laparoscopic colectomy in older patients. Arch Surg 138(3):252–256
Frasson M, Braga M, Vignali A et al (2008) Benefits of laparoscopic colorectal resection are more pronounced in elderly patients. Dis Colon Rectum 51(3):296–300
Vignali A, Di Palo S, Tamburini A et al (2005) Laparoscopic vs. open colectomies in octogenarians: a case-matched control study. Dis Colon Rectum 48(11):2070–2075
Turrentine FE, Wang H, Simpson VB et al (2006) Surgical risk factors, morbidity, and mortality in elderly patients. J Am Coll Surg 203(6):865–877
Biondi A, Vacante M, Ambrosino I et al (2016) Role of surgery for colorectal cancer in the elderly. World J Gastrointest Surg 8(9):606–613
Chang GJ, Skibber JM, Feig BW et al (2007) Are we undertreating rectal cancer in the elderly? An epidemiologic study. Ann Surg 246(2):215–221
Basili G, Lorenzetti L, Biondi G et al (2008) Colorectal cancer in the elderly. Is there a role for safe and curative surgery? ANZ J Surg 78(6):466–470
Colorectal Cancer Collaborative Group (2000) Surgery for colorectal cancer in elderly patients: a systematic review. Lancet 356(9234):968–974
Scott NA, Jeacock J, Kingston RD (1995) Risk factors in patients presenting as an emergency with colorectal cancer. Br J Surg 82(3):321–323
Bray F, Ferlay J, Soerjomataram I et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424
Nelson H, Sargent DJ, Wieand HS et al (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350(20):2050–2059
Guillou PJ, Quirke P, Thorpe H et al (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 365(9472):1718–1726
Veldkamp R, Kuhry E, Hop WC et al (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6(7):477–484
Jeong SY, Park JW, Nam BH et al (2014) Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 15(7):767–774
Russo A, Marana E, Viviani D et al (2009) Diastolic function: the influence of pneumoperitoneum and Trendelenburg positioning during laparoscopic hysterectomy. Eur J Anaesthesiol 26(11):923–927
van der Pas MH, Haglind E, Cuesta MA et al (2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 14(3):210–218
Odeberg-Wernerman S (2000) Laparoscopic surgery–effects on circulatory and respiratory physiology: an overview. Eur J Surg Suppl 585:4–11
Fujii S, Ishibe A, Ota M et al (2014) Short-term results of a randomized study between laparoscopic and open surgery in elderly colorectal cancer patients. Surg Endosc 28(2):466–476
Zhou S, Wang X, Zhao C et al (2019) Laparoscopic vs open colorectal cancer surgery in elderly patients: short- and long-term outcomes and predictors for overall and disease-free survival. BMC Surg 19(1):137
Chan TY, Foo CC, Law WL et al (2019) Outcomes of colorectal cancer surgery in the nonagenarians: 20-year result from a tertiary center. BMC Surg 19(1):155
Miguchi M, Yoshimitsu M, Hakoda K et al (2018) Short-term outcomes of laparoscopic surgery in octogenarians with colorectal cancer: a single-institution analysis. Surg Today 48(3):292–299
Moon SY, Kim S, Lee SY et al (2016) Laparoscopic surgery for patients with colorectal cancer produces better short-term outcomes with similar survival outcomes in elderly patients compared to open surgery. Cancer Med 5(6):1047–1054
Nishikawa T, Ishihara S, Hata K et al (2016) Short-term outcomes of open versus laparoscopic surgery in elderly patients with colorectal cancer. Surg Endosc 30(12):5550–5557
Mukai T, Akiyoshi T, Ueno M et al (2014) Outcomes of laparoscopic surgery for colorectal cancer in oldest-old patients. Surg Laparosc Endosc Percutan Tech 24(4):366–369
Lian L, Kalady M, Geisler D et al (2010) Laparoscopic colectomy is safe and leads to a significantly shorter hospital stay for octogenarians. Surg Endosc 24(8):2039–2043
Hinoi T, Kawaguchi Y, Hattori M et al (2015) Laparoscopic versus open surgery for colorectal cancer in elderly patients: a multicenter matched case-control study. Ann Surg Oncol 22(6):2040–2050
Nakamura T, Sato T, Miura HT et al (2014) Feasibility and outcomes of surgical therapy in very elderly patients with colorectal cancer. Surg Laparosc Endosc Percutan Tech 24(1):85–88
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Chern YJ, Tsai WS, Hung HY et al (2018) The dark side of laparoscopic surgery for colorectal cancer patients aged 75 years or older. Int J Colorectal Dis 33(10):1367–1371
Tei M, Ikeda M, Haraguchi N et al (2009) Postoperative complications in elderly patients with colorectal cancer: comparison of open and laparoscopic surgical procedures. Surg Laparosc Endosc Percutan Tech 19(6):488–492
Braga M, Vignal A, Gianotti L et al (2002) Laparoscopic versus open colorectal surgery: a randomized trial on short-term outcome. Ann Surg 236(6):759–766 (discussion 767)
Chang GJ, Rodriguez-Bigas MA, Skibber JM et al (2007) Lymph node evaluation and survival after curative resection of colon cancer: systematic review. J Natl Cancer Inst 99(6):433–441
Morikawa E, Yasutomi M, Shindou K et al (1994) Distribution of metastatic lymph nodes in colorectal cancer by the modified clearing method. Dis Colon Rectum 37(3):219–223
Toyota S, Ohta H, Anazawa S (1995) Rationale for extent of lymph node dissection for right colon cancer. Dis Colon Rectum 38(7):705–711
Søndenaa K, Quirke P, Hohenberger W et al (2014) The rationale behind complete mesocolic excision (CME) and a central vascular ligation for colon cancer in open and laparoscopic surgery: proceedings of a consensus conference. Int J Colorectal Dis 29(4):419–428
Acknowledgements
This research was supported by Hallym University Research Fund, 2020 (HURF-2020-58).
Funding
Hallym University Research Fund, 2020 (HURF-2020-58).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by ITS, BMK, BCK and MJK. The first draft of the manuscript was written by JYK and JWK. And all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the Institutional Review Board of Dongtan Sacred Heart Hospital (IRB 2020-08-001-001). The Institutional Review Board waived the need to obtain informed consent in view of the retrospective nature of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Son, I.T., Kim, J.Y., Kim, M.J. et al. Clinical and oncologic outcomes of laparoscopic versus open surgery in elderly patients with colorectal cancer: a retrospective multicenter study. Int J Clin Oncol 26, 2237–2245 (2021). https://doi.org/10.1007/s10147-021-02009-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-021-02009-4