Abstract
Background
The grading of urinary tract dilatation (UTD) on postnatal sonography is a fundamental step to establish rational management for infants with antenatal hydronephrosis (ANH). The aim of this study was to compare the prediction accuracy of UTD grading systems for relevant clinical outcomes. In addition, we propose a refinement of the UTD classification by adding quantitative measurements and evaluate its impact on accuracy.
Methods
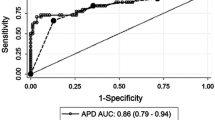
Between 1989 and 2019, 447 infants diagnosed with isolated AHN were prospectively followed. The events of interest were surgical interventions and kidney injury. Comparison of performance of the grading systems and the impact on the accuracy of a modified UTD classification (including the size of the kidney parenchyma) was assessed by the area under the receiver-operating characteristic curve (AUC).
Results
Of 447 infants, 131 (29%) underwent surgical intervention and 26 (5.8%) had developed kidney injury. The median follow-up time was 9 years (IQ range, 7–12 years). The performance for detecting the need for surgical intervention was excellent for all grading systems (AUC > 0.90). However, for predicting kidney injury, the modified UTD classification exhibited significant improvement in accuracy (AUC = 0.913, 95%CI, 0.883–0.937) as compared with UTD classification (AUC = 0.887, 95%CI, 0.854–0.915) (P = 0.027).
Conclusions
Our study confirms that the hydronephrosis grading systems provide excellent accuracy in discriminating patients who need surgical intervention among infants with AHN. Our findings suggest that the inclusion of kidney parenchymal thickness to UTD classification might increase the accuracy for predicting infants who may develop kidney injury.
Graphical abstract
A higher resolution version of the Graphical abstract is available as Supplementary information.




Similar content being viewed by others
References
Lee RS, Cendron M, Kinnamon DD, Nguyen HT (2006) Antenatal hydronephrosis as a predictor of postnatal outcome: a meta-analysis. Pediatrics 118:586–593
Oliveira EA, Oliveira MC, Mak RH (2016) Evaluation and management of hydronephrosis in the neonate. Curr Opin Pediatr 28:195–201
Chiodini B, Ghassemi M, Khelif K, Ismaili K (2019) Clinical outcome of children with antenatally diagnosed hydronephrosis. Front Pediatr 7:103
Dos Santos J, Parekh RS, Piscione TD, Hassouna T, Figueroa V, Gonima P, Vargas I, Farhat W, Rosenblum ND (2015) A new grading system for the management of antenatal hydronephrosis. Clin J Am Soc Nephrol 10:1783–1790
Costa FP, Simões e Silva AC, Mak RH, Ix JH, Vasconcelos MA, Dias CS, Fonseca CC, Oliveira MCL, Oliveira EA (2020) A clinical predictive model of renal injury in children with isolated antenatal hydronephrosis. Clin Kidney J 13:834–841
Fernbach SK, Maizels M, Conway JJ (1993) Ultrasound grading of hydronephrosis: introduction to the system used by the Society for Fetal Urology. Pediatr Radiol 23:478–480
Onen A (2007) An alternative grading system to refine the criteria for severity of hydronephrosis and optimal treatment guidelines in neonates with primary UPJ-type hydronephrosis. J Pediatr Urol 3:200–205
Nguyen HT, Benson CB, Bromley B, Campbell JB, Chow J, Coleman B, Cooper C, Crino J, Darge K, Herndon CD, Odibo AO, Somers MJ, Stein DR (2014) Multidisciplinary consensus on the classification of prenatal and postnatal urinary tract dilation (UTD classification system). J Pediatr Urol 10:982–998
Chow JS, Koning JL, Back SJ, Nguyen HT, Phelps A, Darge K (2017) Classification of pediatric urinary tract dilation: the new language. Pediatr Radiol 47:1109–1115
Scalabre A, Demede D, Gaillard S, Pracros JP, Mouriquand P, Mure PY (2017) Prognostic value of ultrasound grading systems in prenatally diagnosed unilateral urinary tract dilatation. J Urol 197:1144–1149
Braga LH, McGrath M, Farrokhyar F, Jegatheeswaran K, Lorenzo AJ (2017) Associations of Initial Society for Fetal Urology Grades and Urinary Tract Dilatation Risk Groups with Clinical Outcomes in Patients with Isolated Prenatal Hydronephrosis. J Urol 197:831–837
Hodhod A, Capolicchio JP, Jednak R, El-Sherif E, El-Doray Ael A, El-Sherbiny M (2016) Evaluation of urinary tract dilation classification system for grading postnatal hydronephrosis. J Urol 195:725–730
Nguyen HT, Herndon CD, Cooper C, Gatti J, Kirsch A, Kokorowski P, Lee R, Perez-Brayfield M, Metcalfe P, Yerkes E, Cendron M, Campbell JB (2010) The Society for Fetal Urology consensus statement on the evaluation and management of antenatal hydronephrosis. J Pediatr Urol 6:212–231
Bouzada MC, Oliveira EA, Pereira AK, Leite HV, Rodrigues AM, Fagundes LA, Goncalves RP, Parreiras RL (2004) Diagnostic accuracy of fetal renal pelvis anteroposterior diameter as a predictor of uropathy: a prospective study. Ultrasound Obstet Gynecol 24:745–749
Coelho GM, Bouzada MC, Pereira AK, Figueiredo BF, Leite MR, Oliveira DS, Oliveira EA (2007) Outcome of isolated antenatal hydronephrosis: a prospective cohort study. Pediatr Nephrol 22:1727–1734
Dias CS, Silva JM, Pereira AK, Marino VS, Silva LA, Coelho AM, Costa FP, Quirino IG, Simoes ESAC, Oliveira EA (2013) Diagnostic accuracy of renal pelvic dilatation for detecting surgically managed ureteropelvic junction obstruction. J Urol 190:661–666
Schwartz GJ, Brion LP, Spitzer A (1987) The use of plasma creatinine concentration for estimating glomerular filtration rate in infants, children, and adolescents. Pediatr Clin North Am 34:571–590
Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637
Coelho GM, Bouzada MC, Lemos GS, Pereira AK, Lima BP, Oliveira EA (2008) Risk factors for urinary tract infection in children with prenatal renal pelvic dilatation. J Urol 179:284–289
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents (2004) The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114:555–576
Bouzada MC, Oliveira EA, Pereira AK, Leite HV, Rodrigues AM, Fagundes LA, Goncalves RP, Parreiras R (2004) Diagnostic accuracy of postnatal renal pelvic diameter as a predictor of uropathy: a prospective study. Pediatr Radiol 34:798–804
Gotoh H, Masuzaki H, Fukuda H, Yoshimura S, Ishimaru T (1998) Detection and assessment of pyelectasis in the fetus: relationship to postnatal renal function. Obstet Gynecol 92:226–231
Fuhrman DY, Schneider MF, Dell KM, Blydt-Hansen TD, Mak R, Saland JM, Furth SL, Warady BA, Moxey-Mims MM, Schwartz GJ (2017) Albuminuria, proteinuria, and renal disease progression in children with CKD. Clin J Am Soc Nephrol 12:912–920
Gomes RS, Quirino IG, Pereira RM, Vitor BM, Leite AF, Oliveira EA, Simões e Silva AC (2011) Primary versus secondary hypertension in children followed up at an outpatient tertiary unit. Pediatr Nephrol 26:441–447
Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, Hogg RJ, Perrone RD, Lau J, Eknoyan G (2003) National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med 139:137–147
Konda R, Sakai K, Ota S, Abe Y, Hatakeyama T, Orikasa S (2002) Ultrasound grade of hydronephrosis and severity of renal cortical damage on 99m technetium dimercaptosuccinic acid renal scan in infants with unilateral hydronephrosis during followup and after pyeloplasty. J Urol 167:2159–2163
Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig LM, Moher D, Rennie D, de Vet HC, Lijmer JG (2003) The STARD statement for reporting studies of diagnostic accuracy: explanation and elaboration. Ann Intern Med 138:W1–W12
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845
Youden WJ (1950) Index for rating diagnostic tests. Cancer 3:32–35
Grignon A, Filion R, Filiatrault D, Robitaille P, Homsy Y, Boutin H, Leblond R (1986) Urinary tract dilatation in utero: classification and clinical applications. Radiology 160:645–647
Swenson DW, Darge K, Ziniel SI, Chow JS (2015) Characterizing upper urinary tract dilation on ultrasound: a survey of North American pediatric radiologists’ practices. Pediatr Radiol 45:686–694
Onen A (2020) Grading of hydronephrosis: an ongoing challenge. Front Pediatr 8:458
Nelson CP, Lee RS, Trout AT, Servaes S, Kraft KH, Barnewolt CE, Logvinenko T, Chow JS (2019) Interobserver and intra-observer reliability of the urinary tract dilation classification system in neonates: a multicenter study. J Urol 201:1186–1192
Back SJ, Christopher Edgar J, Weiss DA, Oliver ER, Bellah RD, Darge K (2018) Rater reliability of postnatal urinary tract dilation consensus classification. Pediatr Radiol 48:1606–1611
Han M, Kim HG, Lee JD, Park SY, Sur YK (2017) Conversion and reliability of two urological grading systems in infants: the Society for Fetal Urology and the urinary tract dilatation classifications system. Pediatr Radiol 47:65–73
Rickard M, Easterbrook B, Kim S, Farrokhyar F, Stein N, Arora S, Belostotsky V, DeMaria J, Lorenzo AJ, Braga LH (2017) Six of one, half a dozen of the other: a measure of multidisciplinary inter/intra-rater reliability of the society for fetal urology and urinary tract dilation grading systems for hydronephrosis. J Pediatr Urol 13:80.e1-80.e5
Agard H, Massanyi E, Albertson M, Anderson M, Alam M, Lyden E, Del Rio CV (2020) The different elements of the Urinary Tract Dilation (UTD) Classification System and their capacity to predict findings on mercaptoacetyltriglycine (MAG3) diuretic renography. J Pediatr Urol 16:686.e1-686.e6
Nelson CP, Lee RS, Trout AT, Servaes S, Kraft KH, Barnewolt CE, Logvinenko T, Chow JS (2019) The association of postnatal urinary tract dilation risk score with clinical outcomes. J Pediatr Urol 15:341.e1-341.e6
Braga LH, McGrath M, Farrokhyar F, Jegatheeswaran K, Lorenzo AJ (2018) Society for Fetal Urology Classification vs Urinary Tract Dilation Grading System for prognostication in prenatal hydronephrosis: a time to resolution analysis. J Urol 199:1615–1621
Melo FF, Mak RH, Simões e Silva AC, Vasconcelos MA, Dias CS, Rosa LC, Shiomatsu GY, Storch C, C OM, Oliveira EA (2021) Evaluation of urinary tract dilation classification system for prediction of long-term outcomes in isolated antenatal hydronephrosis: A Cohort Study. J Urol. https://doi.org/10.1097/JU.0000000000001899
Funding
This study was partially supported by CNPq (Brazilian National Research Council, Grant 302258/2019–1, 430246/2018–8, 302154/2016–7) and FAPEMIG (Fundação de Amparo à Pesquisa do Estado de Minas Gerais, Grant PPM-00228–15, PPM-00435–18). R.H.M. is supported by NIH grants 2U01DK066143-16 and 1R01DK125811. E.A.O. is supported by grant CAPES 2746–15-8. ACSS is supported by CNPq Grant 302153/2019–5. Dr. E.A. Oliveira and Dr. A.C. Simões e Silva received a research grant from the Brazilian Research Council (CNPq).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Ethics Committee of UFMG and the parents or persons responsible for the children gave written informed consent to participate.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Melo, F.F., Vasconcelos, M.A., Mak, R.H. et al. Postnatal urinary tract dilatation classification: improvement of the accuracy in predicting kidney injury. Pediatr Nephrol 37, 613–623 (2022). https://doi.org/10.1007/s00467-021-05254-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-021-05254-x