Abstract
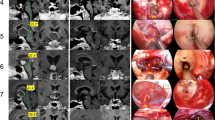
The strictly third ventricle craniopharyngioma topography (strictly 3V CP) defines the subgroup of lesions developed above an anatomically intact third ventricle floor (3VF). The true existence of this exceedingly rare topographical category is highly controversial owing to the presumed embryological CP origin from Rathke’s pouch, a structure developmentally situated outside the neural tube. This study thoroughly analyzes the largest series of strictly 3V CPs ever collected. From 5346 CP reports published between 1887 and 2021, we selected 245 cases with reliable pathological, surgical, and/or neuroradiological verification of an intact 3VF beneath the tumor. This specific topography occurs predominantly in adult (92.6%), male (64.4%) patients presenting with headache (69.2%), and psychiatric disturbances (59.2%). Neuroradiological features defining strictly 3V CPs are a tumor-free chiasmatic cistern (95.9%), an entirely visible pituitary stalk (86.4%), and the hypothalamus positioned around the tumor’s lower pole (92.6%). Most are squamous papillary (82%), showing low-risk severity adhesions to the hypothalamus (74.2%). The adamantinomatous variant, however, associates a higher risk of severe hypothalamic adhesion (p < .001). High-risk attachments are also associated with psychiatric symptoms (p = .013), which represented the major predictor for unfavorable prognoses (83.3% correctly predicted) among cases operated from 2006 onwards. CP recurrence is associated with infundibulo-tuberal symptoms (p = .036) and incomplete surgical removal (p = .02). The exclusive demographic, clinico-pathological and neuroradiological characteristics of strictly 3V CPs make them a separate, unique topographical category. Accurately distinguishing strictly 3V CPs preoperatively from those tumors replacing the infundibulum and/or tuber cinereum (infundibulo-tuberal or not strictly 3V CPs) is critical for proper, judicious surgical planning.







Similar content being viewed by others
Abbreviations
- ACP:
-
Adamantinomatous craniopharyngioma
- CP:
-
Craniopharyngioma
- EETS:
-
Endoscopic endonasal transsphenoidal
- FTV:
-
Frontal transventricular
- HICP:
-
High intracranial pressure
- MRI:
-
Magnetic resonance imaging
- PCP:
-
Papillary craniopharyngioma
- Tc:
-
Transcallosal
- TLT:
-
Translamina terminalis
- TS:
-
Transsphenoidal
- 3V:
-
Third ventricle
- 3VF:
-
Third ventricle floor
References
Burger PC, Scheithauer BW, Vogel FS (2002) Region of the sella turcica. Craniopharyngiomas. In: Surgical pathology of the nervous system and its coverings, 4th edn. Churchill Livingstone, New York, pp 475–483
Buslei R, Rushing EJ, Giangaspero F, Paulus W, Burger PC, Santagata S (2016) Craniopharyngioma. In: Louis DN, Ohgaki H, Wiestier OD, Cavenee W, Ellison DW, Figarella-Branger D, Perry A, Reifenberger, von Deimling A (eds) WHO classification of tumours of the central nervous system, 4th eds. International Agency for Research on Cancer, Lyon, pp 324–328
Pascual JM, González-Llanos F, Barrios L, Roda JM (2004) Intraventricular craniopharyngiomas: topographical classification and surgical approach selection based on an extensive overview. Acta Neurochir (Wien) 146:785–802. https://doi.org/10.1007/s00701-004-0295-3
Pascual JM, Prieto R, Carrasco R, Barrios L (2013) Displacement of mammillary bodies by craniopharyngiomas involving the third ventricle: surgical-MRI correlation and use in topographical diagnosis. J Neurosurg 119:381–405. https://doi.org/10.3171/2013.1.JNS111722
Pascual JM, Prieto R, Carrasco R (2011) Infundibulo-tuberal or not strictly intraventricular craniopharyngioma: evidence for a major topographical category. Acta Neurochir (Wien) 153:2403–2426. https://doi.org/10.1007/s00701-011-1149-4
Qi S, Liu Y, Wang C, Fan J, Pan J, Zhang X, Lu Y (2020) Membrane structures between craniopharyngioma and the third ventricle floor based on the QST classification and its significance: a pathological study. J Neuropathol Exp Neurol 79:966–974. https://doi.org/10.1093/jnen/nlaa087
Pascual JM, Carrasco R, Prieto R, Gonzalez-Llanos F, Alvarez F, Roda JM (2008) Craniopharyngioma classification. J Neurosurg 109:1180–1182. https://doi.org/10.3171/JNS.2008.109.12.1180
Prieto R, Rosdolsky M, Hofecker V, Barrios L, Pascual JM (2020) Craniopharyngioma treatment: an updated summary of important clinicopathological concepts. Expert Rev Endocrinol Metab 15:261–282. https://doi.org/10.1080/17446651.2020.1770081
Pan J, Qi S, Lu Y, Fan J, Zhang X, Zhou J, Peng J (2011) Intraventricular craniopharyngioma: morphological analysis and outcome evaluation of 17 cases. Acta Neurochir (Wien) 153:773–784. https://doi.org/10.1007/s00701-010-0938-5
Pascual JM, Prieto R, Castro-Dufourny I, Carrasco R, Strauss S, Barrios L (2014) Development of intracranial approaches for craniopharyngiomas: an analysis of the first 160 historical procedures. Neurosurg Focus 36:E13. https://doi.org/10.3171/2014.2.FOCUS13567
Yu T, Sun X, Ren X, Cui X, Wang J, Lin S (2014) Intraventricular craniopharyngiomas: surgical management and outcome analysis in 24 cases. World Neurosurg 82:1209–1215. https://doi.org/10.1016/j.wneu.2014.06.015
Brastianos PK, Taylor-Weiner A, Manley PE et al (2014) Exome sequencing identifies BRAF mutations in papillary craniopharyngiomas. Nat Genet 46:161–165. https://doi.org/10.1038/ng.2868
Juratli TA, Jones PS, Wang N et al (2019) Targeted treatment of papillary craniopharygiomas harboring BRAF V600E mutations. Cancer 125:2910–2914. https://doi.org/10.1002/cncr.32197
Behari S, Banerji D, Mishra A, Sharma S, Sharma S, Chhabra DK, Jain VK (2003) Intrinsic third ventricular craniopharyngiomas: report on six cases and review of the literature. Surg Neurol 60:245–253. https://doi.org/10.1016/s0090-3019(03)00132-0
Forbes JA, Ordóñez-Rubiano EG, Tomasiewicz HC et al (2018) Endonasal endoscopic transsphenoidal resection of intrinsic third ventricular craniopharyngioma: surgical results. J Neurosurg. https://doi.org/10.3171/2018.5.JNS18198
Gu Y, Zhang X, Hu F, Yu Y, Xie T, Sun C, Li W (2015) Suprachiasmatic translaminar terminalis corridor used in endoscopic endonasal approach for resecting third ventricular craniopharyngioma. J Neurosurg 122:1166–1172. https://doi.org/10.3171/2015.1.JNS132842
Jung TY, Jung S, Jang WY, Moon KS, Kim IY, Kang SS (2012) Operative outcomes and adjuvant treatment of purely third ventricle craniopharyngioma after transcallosal approach. Br J Neurosurgery 26:355–360. https://doi.org/10.3109/02688697.2011.631615
Maira G, Anile C, Colosimo C, Cabezas D (2000) Craniopharyngiomas of the third ventricle: trans-lamina terminalis approach. Neurosurgery 47:857–865. https://doi.org/10.1097/00006123-200010000-00014
Nishioka H, Fukuhara N, Yamaguchi-Okada M, Yamada S (2016) Endoscopic endonasal surgery for purely intra-third ventricle craniopharyngioma. World Neurosurg 91:266–271. https://doi.org/10.1016/j.wneu.2016.04.042
Fukushima T, Hirakawa K, Tomonaga M (1990) Intraventricular craniopharyngioma: its characteristics in magnetic resonance imaging and successful total removal. Surg Neurol 33:22–27. https://doi.org/10.1016/0090-3019(90)90220-j
Iwasaki K, Kondo A, Takahashi JB, Yamanobe K (1992) Intraventricular craniopharyngioma: report of two cases and review of the literature. Surg Neurol 38:294–301. https://doi.org/10.1016/0090-3019(92)90045-o
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med 21:e1000097. https://doi.org/10.1371/journal.pmed.1000097
Prieto R, Pascual JM, Rosdolsky M, Castro-Dufourny I, Carrasco R, Strauss S, Barrios L (2016) Craniopharyngioma adherence: a comprehensive topographical categorization and outcome-related risk stratification model based on the methodical examination of 500 tumors. Neurosurg Focus 41:E13. https://doi.org/10.3171/2016.9.FOCUS16304
Pascual JM, Prieto R, Castro-Dufourny I et al (2018) Craniopharyngiomas primarily involving the hypothalamus: a model of neurosurgical lesions to elucidate the neurobiological basis of psychiatric disorders. World Neurosurg 120:e1245–e1278. https://doi.org/10.1016/j.wneu.2018.09.053
Prieto R, Pascual JM, Rosdolsky M, Barrios L (2018) Preoperative assessment of craniopharyngioma adherence: magnetic resonance imaging findings correlated with the severity of tumor attachment to the hypothalamus. World Neurosurg 110:e404–e426. https://doi.org/10.1016/j.wneu.2017.11.012
Fahlbusch R, Honegger J, Paulus W, Huk W, Buchfelder M (1999) Surgical treatment of craniopharyngiomas: experience with 168 patients. J Neurosurg 90:237–250. https://doi.org/10.3171/jns.1999.90.2.0237
Prieto R, Pascual JM, Barrios L (2015) Optic chiasm distortions caused by craniopharyngiomas: clinical and magnetic resonance imaging correlation and influence on visual outcome. World Neurosurg 83:500–529. https://doi.org/10.1016/j.wneu.2014.10.002
Cashion EL, Young JM (1971) Intraventricular craniopharyngioma. report of two cases. J Neurosurg 34:84–87. https://doi.org/10.3171/jns.1971.34.1.0084
Dobos EI, Freed CG, Ashe SMP (1953) An intrinsic tumor of the third ventricle. J Neuropath Exp Neurol 12:232–243. https://doi.org/10.1097/00005072-195307000-00003
Lejeune J-P, Le Gars D, Haddad E (2000) Tumeurs du troisième ventricule: analyse d’une serie de 262 cas. Neurochirurgie 46:211–238
Mott FW, Barratt JOW (1899) Three cases of tumor of the third ventricle. Arch Neurol Path Lab London County Asyl Claybury 1:417–439
Schmidt B, Gherardi R, Poirier J, Caron JP (1984) Craniopharyngiome pédiculé du troisième ventricule. Rev Neurol 140:281–283
Selke W (1891) Über ein epitheliales Papillom des Gehirns. Inaugural-Dissertation. Königsberg I. Pr. Druck von M. Liedtke, Bergplatz 7. (Doctoral dissertation)
Pascual JM, Prieto R, Navas M, Carrasco R (2010) Conquest of third ventricle craniopharyngiomas. J Neurosurg 112:1156–1161. https://doi.org/10.3171/2009.8.JNS091094
Cushing H (1912) The Pituitary Body and its Disorders. Clinical states produced by disorders of the hypophysis cerebri. JB Lippincott company, Philadelphia & London
Pascual JM, Prieto R (2018) Harvey Cushing’s craniopharyngioma treatment. Part 1. Identification and clinicopathological characterization of this challenging pituitary tumor. J Neurosurg 131:949–963. https://doi.org/10.3171/2018.5.JNS18153
Prieto R, Pascual JM (2018) Harvey Cushing’s craniopharyngioma treatment. Part 2. Surgical strategies and results of his pioneering series. J Neurosurg 131:964–978. https://doi.org/10.3171/2018.5.JNS18154
Steno J (1985) Microsurgical topography of craniopharyngiomas. Acta Neurochir Suppl 35:94–100
Erdheim J (1904) Über Hypophysengangsgeschwülste und Hirncholesteatome. Sitzungsb Kais Akad Wissen Math Naturw Klin 113:537–726
Pascual JM, Rosdolsky M, Prieto R, Strauss S, Winter E, Ulrich W (2015) Jakob Erdheim (1874–1937): father of hypophyseal-duct tumors (craniopharyngiomas). Virchows Arch 467:459–469. https://doi.org/10.1007/s00428-015-1798-4
Zhou L, You C (2009) Letter: Craniopharyngioma classification. J Neurosurg 111:197–199. https://doi.org/10.3171/2009.2.JNS081430
Qi S (2020) Atlas of craniopharyngioma. pathology, classification and surgery. Springer Nature Singapore Pte Ltd
Prieto R, Pascual JM (2019) Letter to the Editor. The craniopharyngioma-hypothalamus relationship. J Neurosurg. https://doi.org/10.3171/2019.7.JNS191780
Aydin S, Yilmazlar S, Aker S, Korfali E (2009) Anatomy of the floor of the third ventricle in relation to endoscopy ventriculostomy. Clin Anat 22:916–924. https://doi.org/10.1002/ca.20867
Iacarino C, Tedeschi E, Rapana A, Massarelli I, Belfiore G, Quarantelli M, Bellotti A (2009) Is the distance between mammillary bodies predictive of a thickened third ventricle floor? J Neurosurg 110:852–857. https://doi.org/10.3171/2008.4.17539
Attwell WJ (1926) The development of the hypophysis cerebri in man, with special reference to the pars tuberalis. Am J Anat 37:159–193. https://doi.org/10.1002/aja.1000370107
Kunishio K, Yamamoto Y, Sunami N, Asari S, Akagi T, Ohtsuki Y (1987) Craniopharyngioma in the third ventricle: necropsy findings and histogenesis. J Neurol Neurosurg Psychiatry 50:1053–1056. https://doi.org/10.1136/jnnp.50.8.1053
Tilney F (1936) The development and constituents of the human hypophysis. Bull Neur Inst New York 5:387–436
Ciric IS, Cozzens JW (1980) Craniopharyngiomas: transsphenoidal method of approach—for the virtuoso only? Clin Neurosurg 27:169–187
Prabhu VC, Brown HG (2005) The pathogenesis of craniopharyngiomas. Childs Nerv Syst 21:622–627. https://doi.org/10.1007/s00381-005-1190-9
Prieto R, Pascual JM (2018) Can tissue biomarkers reliably predict the biological behavior of craniopharyngiomas? A comprehensive overview. Pituitary 21:431–442. https://doi.org/10.1007/s11102-018-0890-6
Luse SA, Kernohan JW (1955) Squamous-cell nests of the pituitary gland. Cancer 8:623–638. https://doi.org/10.1002/1097-0142(1955)8:3%3c623::aid-cncr2820080328%3e3.0.co;2-d
Hunter IJ (1955) Squamous metaplasia of cells of the anterior pituitary gland. J Path Bact 69:141–145. https://doi.org/10.1002/path.1700690120
Martinez-Barbera JP, Andoniadou CL (2016) Concise review: Paracrine role of stem cells in pituitary tumors: a focus on adamantinomatous craniopharyngioma. Stem Cells 34:268–276. https://doi.org/10.1002/stem.2267
Yasargil MG (1996) Craniopharyngiomas. In: Microneurosurgery of CNS Tumors. Vol IV B. Georg Thieme Verlag, Stuttgart, Germany, pp 205–223
Pascual JM, Prieto R, Rosdolsky M et al (2018) Cystic tumors of the pituitary infundibulum: seminal autopsy specimens (1899 to 1904) that allowed clinical-pathological craniopharyngioma characterization. Pituitary 21:393–405. https://doi.org/10.1007/s11102-018-0889-z
Momin AA, Recinos MA, Cioffi G et al (2021) Descriptive epidemiology of craniopharyngiomas in the United States. Pituitary 24:517–522. https://doi.org/10.1007/s11102-021-01127-6
Müller HL, Merchant T, Warmuth-Metz M, Martinez-Barbera JP, Pugest S (2019) Craniopharyngioma Nat Rev Dis Primers 5:75. https://doi.org/10.1038/s41572-019-0125-9
Cushing H (1913) Psychic disturbances associated with disorders of the ductless glands. Am J Insanity 69:965–990
Fulton JF, Bailey P (1929) Tumors in the region of the third ventricle: their diagnosis and relation to pathological sleep. J Nerv Mental Dis 69:1–25,145–164,261–277. https://doi.org/10.1097/00005053-192901000-00001
Prieto R, Pascual JM (2019) Percival S Bailey: eminent scholar of neurosciences who revealed the workings of the hypothalamus through clinicopathological research on craniopharyngiomas. J Neurosurg. https://doi.org/10.3171/2019.3.JNS183145
Alpers BJ (1937) Relation of the hypothalamus to disorders of personality. Arch Neurol Psychiatr 38:291–303. https://doi.org/10.1001/archneurpsyc.1937.02260200063005
Pascual JM, Prieto R, Rosdolsky M (2021) Craniopharyngiomas primarily affecting the hypothalamus. In: Swaab DF, Lucassen PJ, Kreier F, Buijs R, Salehi A (ed) The human hypothalamus, Vol 181: Neuroendocrine disorders. In: Aminoff MJ, Voller F, Swaab DF (ed) Handbook of Clinical Neurology. Third series. Elsevier, pp 75–115. https://doi.org/10.1016/B978-0-12-820683-6.00007-5
Reeves AG, Plum F (1969) Hyperphagia, rage and dementia accompanying a ventromedial hypothalamic neoplasm. Arch Neurol 20:616–624. https://doi.org/10.1001/archneur.1969.00480120062005
Vann SD, Aggleton JP (2004) The mammillary bodies: two memory systems in one? Nat Rev Neurosci 5:35–44. https://doi.org/10.1038/nrn1299
Williams M, Pennybacker J (1954) Memory disturbances in third ventricle tumours. J Neurol Neurosurg Psychiat 17:115–123. https://doi.org/10.1136/jnnp.17.2.115
Prieto R, Pascual JM, Barrios L (2017) Topographic diagnosis of craniopharyngiomas: the accuracy of MRI findings observed on conventional T1 and T2 images. AJNR Am J Neuroradiol 38:2073–2080. https://doi.org/10.3174/ajnr.A5361
Prieto R, Pascual JM (2020) Craniopharyngioma diagnosis: a rationale for accurate MRI assessment of tumor topography and adhesion to the hypothalamus. In: Jouanneau E, Raverot G (eds) Adult craniopharyngiomas. Differences and lessons from paediatrics. Springer, Cham, Switzerland, pp 55–77. https://doi.org/10.1007/978-3-030-41176-3_4
Du C, Feng CY, Yuan XR et al (2016) Microsurgical management of craniopharyngiomas via a unilateral subfrontal approach: a retrospective study of 177 continuous cases. World Neurosurg 90:454–468. https://doi.org/10.1016/j.wneu.2016.03.002
Shi X, Zhou Z, Wu B et al (2017) Outcome of radical surgical resection for craniopharyngioma with hypothalamic preservation: a single-center, retrospective study of 1054 patients. World Neurosurg 102:167–180. https://doi.org/10.1016/j.wneu.2017.02.095
Cavallo LM, Solari D, Esposito F, Cappabianca P (2013) The endoscopic endonasal approach for the management of craniopharyngiomas involving the third ventricle. Neurosurg Rev 36:27–37. https://doi.org/10.1007/s10143-012-0403-4
Yang L, Xie SH, Fang C, Zeng EM, Tang B, Hong T (2019) Preservation of hypothalamic function with endoscopic endonasal resection of hypothalamus-invaded craniopharyngiomas. World Neurosurg 132:e841–e851. https://doi.org/10.1016/j.wneu.2019.07.225
Honegger J, Grabenbauer GG, Paulus W, Fahlbusch R (1999) Regresion of a large solid papillary craniopharyngioma following fractionated external radiotherapy. J Neurooncol 41:161–266. https://doi.org/10.1023/a:1006112600805
Kobayashi T, Kida Y, Mori Y, Hasegawa T (2005) Long-term results of gamma knife surgery for the treatment of craniopharyngioma in 98 consecutive cases. J Neurosurg 103(6 Suppl):482–488. https://doi.org/10.3171/ped.2005.103.6.0482
Fujio S, Juratli TA, Arita K et al (2019) A clinical rule for preoperative prediction of BRAF mutation status in craniopharyngiomas. Neurosurgery 85:204–210. https://doi.org/10.1093/neuros/nyy569
Rao M, Bhattacharjee M, Shepard S, Hsu S (2019) Newly diagnosed papillary craniopharyngioma with BRAF V600E mutation treated with single-agent selective BRAF inhibitor dabrafenib: a case report. Oncotarget 10:6038–6042. https://doi.org/10.18632/oncotarget.27203
Prieto R, Castro-Dufourny I, Carrasco R, Barrios L, Pascual JM (2016) Craniopharyngioma recurrence: the impact of tumor topography. J Neurosurg 125:1043–1049. https://doi.org/10.3171/2016.3.JNS16630
Acknowledgements
The authors wish to especially thank Crystal Smith and Liliya Gusakova, Reference Librarians at the National Library of Medicine, National Institutes of Health (Bethesda, MD), Lucretia Maclure and Jack Eckert, Librarians at the Francis Countway Medical Library at Harvard Medical School (Boston, MA), as well as Melissa Grafe, John R. Bumstead Librarian for Medical History, Head of the Medical Library of the Cushing/Whitney Medical Library and Bill Landis of the Manuscript and Archives Department of the Sterling Memorial Library, Yale University (New Haven, CT) for their invaluable assistance during the process of searching and retrieving the original works used in this study. We are very grateful to Maria Rosdolsky for assisting with the translation of German works. We are also indebted to Eduard Winter and Verena Hofecker from the Pathologisch-anatomische Sammlung im Narrenturm-NHM, Vienna, Austria for allowing us access to the collection of brain tumor specimens. Finally, we are grateful to George Hamilton for his critical review of the language and style of the manuscript. This work is dedicated in loving memory to Ricardo Prieto (1948–2021).
Author information
Authors and Affiliations
Contributions
Ruth Prieto: conceived and designed the analysis, collected the data, performed the statistical analysis and interpretation of data, wrote the paper, and approved the final version of the manuscript; Laura Barrios: performed the statistical analysis and approved the final version of the manuscript; José M. Pascual: conceived and designed the analysis, collected the data, critically revised the article, and approved the final version of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Prieto, R., Barrios, L. & Pascual, J.M. Strictly third ventricle craniopharyngiomas: pathological verification, anatomo-clinical characterization and surgical results from a comprehensive overview of 245 cases. Neurosurg Rev 45, 375–394 (2022). https://doi.org/10.1007/s10143-021-01615-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-021-01615-0