Abstract
Purpose of Review
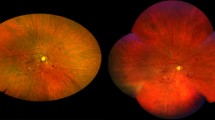
Early detection and treatment are important for preventing vision loss from diabetic retinopathy. Historically, the gold standard for grading diabetic retinopathy has been based on 7-field 30-degree color fundus photographs that capture roughly the central third of the retina. Our aim was to review recent literature on the role of ultra-widefield (allowing capture of up to 82% of the retina in one frame) fundus imaging in screening, prognostication, and treatment of diabetic retinopathy.
Recent Findings
Ultra-widefield fundus imaging can capture peripheral retinal lesions outside the traditional 7-field photographs that may correlate with increased risk of diabetic retinopathy progression. The speed and ability to image through undilated pupils make ultra-widefield imaging attractive for tele-ophthalmology screening. Ultra-widefield fluorescein angiography may help guide targeted laser treatment in eyes with proliferative diabetic retinopathy.
Summary
Ultra-widefield imaging has potential to help shape new diabetic retinopathy screening, staging, and treatment protocols.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as:•• Of major importance
Wong TY, Sun J, Kawasaki R, Ruamviboonsuk P, Gupta N, Lansingh VC, et al. Guidelines on diabetic eye care: the International Council of Ophthalmology recommendations for screening, follow-up, referral, and treatment based on resource settings. Ophthalmology. 2018;125:1608–22.
Cheung N, Mitchell P, Wong TY. Diabetic retinopathy. Lancet. 2010;376:124–36.
Feman SS. The natural history of the first clinically visible features of diabetic retinopathy. Trans Am Ophthalmol Soc. 1994;92:745–73.
Russell JF, Shi Y, Scott NL, Gregori G, Rosenfeld PJ. Longitudinal angiographic evidence that intraretinal microvascular abnormalities can evolve into neovascularization. Ophthalmol Retina. 2020;4:1146–50.
Yau JW, Rogers SL, Kawasaki R, Lamoureux EL, Kowalski JW, Bek T, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35:556–64.
Diabetic retinopathy study. Report Number 6. Design, methods, and baseline results. Report Number 7. A modification of the Airlie House classification of diabetic retinopathy. Prepared by the Diabetic Retinopathy. Invest Ophthalmol Vis Sci. 1981;21:1–226.
Grading diabetic retinopathy from stereoscopic color fundus photographs--an extension of the modified Airlie House classification. ETDRS report number 10. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology. 1991;98:786–806.
Silva PS, Cavallerano JD, Haddad NM, Kwak H, Dyer KH, Omar AF, et al. Peripheral lesions identified on ultrawide field imaging predict increased risk of diabetic retinopathy progression over 4 years. Ophthalmology. 2015;122:949–56.
Photocoagulation treatment of proliferative diabetic retinopathy. Clinical application of Diabetic Retinopathy Study (DRS) findings, DRS Report Number 8. The Diabetic Retinopathy Study Research Group. Ophthalmology. 1981;88:583–600.
Early photocoagulation for diabetic retinopathy. ETDRS report number 9. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology. 1991;98:766–85.
Choudhry N, Duker JS, Freund KB, Kiss S, Querques G, Rosen R, et al. Classification and guidelines for widefield imaging: recommendations from the International Widefield Imaging Study Group. Ophthalmol Retina. 2019;3:843–9.
Patel SN, Shi A, Wibbelsman TD, Klufas MA. Ultra-widefield retinal imaging: an update on recent advances. Ther Adv Ophthalmol. 2020;12:2515841419899495.
Kernt M, Hadi I, Pinter F, Seidensticker F, Hirneiss C, Haritoglou C, et al. Assessment of diabetic retinopathy using nonmydriatic ultra-widefield scanning laser ophthalmoscopy (Optomap) compared with ETDRS 7-field stereo photography. Diabetes Care. 2012;35:2459–63.
Hirano T, Imai A, Kasamatsu H, Kakihara S, Toriyama Y, Murata T. Assessment of diabetic retinopathy using two ultra-wide-field fundus imaging systems, the Clarus and Optos systems. BMC Ophthalmol. 2018;18:332.
Verma A, Alagorie AR, Ramasamy K, van Hemert J, Yadav NK, Pappuru RR, et al. Distribution of peripheral lesions identified by mydriatic ultra-wide field fundus imaging in diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol. 2020;258:725–33.
Fundus photographic risk factors for progression of diabetic retinopathy. ETDRS report number 12. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology. 1991;98:823–33.
Aiello LP, Odia I, Glassman AR, Melia M, Jampol LM, Bressler NM, et al. Comparison of early treatment diabetic retinopathy study standard 7-field imaging with ultrawide-field imaging for determining severity of diabetic retinopathy. JAMA Ophthalmol. 2019;137:65–73 This is a prospective observational study intended to evaluate the role of ultra-widefield fundus imaging compared to ETDRS 7-field 30-degree color fundus photographs for diabetic retinopathy staging and prognostication.
Afshar AR, Oldenburg CE, Stewart JM. A novel hybrid fixed and mobile ultra-widefield imaging program for diabetic teleretinopathy screening. Ophthalmol Retina. 2019;3:576–9.
Hussain N, Edraki M, Tahhan R, Sanalkumar N, Kenz S, Akasha NK, et al. Telemedicine for diabetic retinopathy screening using an ultra-widefield fundus camera. Clin Ophthalmol. 2017;11:1477–82.
Lois N, Cook JA, Wang A, Aldington S, Mistry H, Maredza M, et al. Evaluation of a new model of care for people with complications of diabetic retinopathy: the EMERALD study. Ophthalmology. 2021;128:561–73 This is a prospective multicenter study showing that trained nonmedical graders can screen for proliferative diabetic retinopathy from ultra-widefield fundus images with high sensitivity compared to ophthalmologists.
Bhaskaranand M, Ramachandra C, Bhat S, Cuadros J, Nittala MG, Sadda SR, et al. The value of automated diabetic retinopathy screening with the EyeArt system: a study of more than 100,000 consecutive encounters from people with diabetes. Diabetes Technol Ther. 2019;21:635–43.
Wang K, Jayadev C, Nittala MG, Velaga SB, Ramachandra CA, Bhaskaranand M, et al. Automated detection of diabetic retinopathy lesions on ultrawidefield pseudocolour images. Acta Ophthalmol. 2018;96:e168–e73.
Tang F, Luenam P, Ran AR, Quadeer AA, Raman R, Sen P, et al. Detection of diabetic retinopathy from ultra-widefield scanning laser ophthalmoscope images: a multicenter deep learning analysis. Ophthalmol Retina. 2021 Feb 1;S2468-6530(21):00035-X. This is a multicenter study showing that a deep learning model can achieve high sensitivity and specificity in classifying diabetic retinopathy from ultra-widefield fundus images.
Ehlers JP, Jiang AC, Boss JD, Hu M, Figueiredo N, Babiuch A, et al. Quantitative ultra-widefield angiography and diabetic retinopathy severity: an assessment of panretinal leakage index, ischemic index and microaneurysm count. Ophthalmology. 2019;126:1527–32.
Antaki F, Coussa RG, Mikhail M, Archambault C, Lederer DE. The prognostic value of peripheral retinal nonperfusion in diabetic retinopathy using ultra-widefield fluorescein angiography. Graefes Arch Clin Exp Ophthalmol. 2020;258:2681–90.
Nicholson L, Ramu J, Chan EW, Bainbridge JW, Hykin PG, Talks SJ, et al. Retinal nonperfusion characteristics on ultra-widefield angiography in eyes with severe nonproliferative diabetic retinopathy and proliferative diabetic retinopathy. JAMA Ophthalmol. 2019;137:626–31 This is a post hoc analysis of randomized controlled trial data that identified a threshold amount of nonperfusion on ultra-widefield fluorescein angiography that can help distinguish between eyes with nonproliferative and proliferative diabetic retinopathy.
Yu G, Aaberg MT, Patel TP, Iyengar RS, Powell C, Tran A, et al. Quantification of retinal nonperfusion and neovascularization with ultrawidefield fluorescein angiography in patients with diabetes and associated characteristics of advanced disease. JAMA Ophthalmol. 2020;138:680–8.
Jiang A, Srivastava S, Figueiredo N, Babiuch A, Hu M, Reese J, et al. Repeatability of automated leakage quantification and microaneurysm identification utilising an analysis platform for ultra-widefield fluorescein angiography. Br J Ophthalmol. 2020;104:500–3.
Babiuch AS, Wykoff CC, Srivastava SK, Talcott K, Zhou B, Hach J, et al. Retinal leakage index dynamics on ultra-widefield fluorescein angiography in eyes treated with intravitreal aflibercept for proliferative diabetic retinopathy in the recovery study. Retina. 2020;40:2175–83.
Gross JG, Glassman AR, Liu D, Sun JK, Antoszyk AN, Baker CW, et al. Five-year outcomes of panretinal photocoagulation vs intravitreous ranibizumab for proliferative diabetic retinopathy: a randomized clinical trial. JAMA Ophthalmol. 2018;136:1138–48.
Writing Committee for the Diabetic Retinopathy Clinical Research N, Gross JG, Glassman AR, Jampol LM, Inusah S, Aiello LP, et al. Panretinal photocoagulation vs intravitreous ranibizumab for proliferative diabetic retinopathy: a randomized clinical trial. JAMA. 2015;314:2137–46.
Hutton DW, Stein JD, Glassman AR, Bressler NM, Jampol LM, Sun JK, et al. Five-year cost-effectiveness of intravitreous ranibizumab therapy vs panretinal photocoagulation for treating proliferative diabetic retinopathy: a secondary analysis of a randomized clinical trial. JAMA Ophthalmol. 2019;137:1424–1432.
Obeid A, Su D, Patel SN, Uhr JH, Borkar D, Gao X, et al. Outcomes of eyes lost to follow-up with proliferative diabetic retinopathy that received panretinal photocoagulation versus intravitreal anti-vascular endothelial growth factor. Ophthalmology. 2019;126:407–13.
Pahor D. Visual field loss after argon laser panretinal photocoagulation in diabetic retinopathy: full- versus mild-scatter coagulation. Int Ophthalmol. 1998;22:313–9.
Muqit MM, Marcellino GR, Henson DB, Young LB, Patton N, Charles SJ, et al. Optos-guided pattern scan laser (Pascal)-targeted retinal photocoagulation in proliferative diabetic retinopathy. Acta Ophthalmol. 2013;91:251–8.
Nikkhah H, Ghazi H, Razzaghi MR, Karimi S, Ramezani A, Soheilian M. Extended targeted retinal photocoagulation versus conventional pan-retinal photocoagulation for proliferative diabetic retinopathy in a randomized clinical trial. Int Ophthalmol. 2018;38:313–21 This is a randomized controlled trial suggesting that targeted panretinal photocoagulation guided by areas of nonperfusion on ultra-widefield fluorescein angiography may be a viable alternative to conventional panretinal photocoagulation for treatment of proliferative diabetic retinopathy, with fewer laser spots and potentially less loss of visual field.
Liu J, Gibson E, Ramchal S, Shankar V, Piggott K, Sychev Y, et al. Diabetic retinopathy screening with automated retinal image analysis in a primary care setting improves adherence to ophthalmic care. Ophthalmol Retina. 2021;5:71–7.
Martinez JA, Parikh PD, Wong RW, Harper CA, Dooner JW, Levitan M, et al. Telemedicine for diabetic retinopathy screening in an urban, insured population using fundus cameras in a primary care office setting. Ophthalmic Surg Lasers Imaging Retina. 2019;50:e274–e7.
Funding
None
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical collection on Microvascular Complications—Retinopathy
Rights and permissions
About this article
Cite this article
Cai, S., Liu, T.Y.A. The Role of Ultra-Widefield Fundus Imaging and Fluorescein Angiography in Diagnosis and Treatment of Diabetic Retinopathy. Curr Diab Rep 21, 30 (2021). https://doi.org/10.1007/s11892-021-01398-0
Accepted:
Published:
DOI: https://doi.org/10.1007/s11892-021-01398-0