Abstract
Background
Cardiomyopathy is the leading cause of death in Duchenne muscular dystrophy (DMD), but studies suggest heart failure biomarkers correlate poorly with cardiomyopathy severity. DMD clinical trials have used troponin I (cTnI) as a biomarker of toxicity, but it is unclear if asymptomatic DMD patients have elevated cTnI. We longitudinally evaluated cTnI, brain natriuretic peptide (BNP), and N-terminal pro-BNP (NT-proBNP) in a DMD cohort.
Methods
DMD patients were prospectively enrolled and followed for 3 years. Serum was drawn at the time of cardiac magnetic resonance (CMR). Normal biomarker values were derived from healthy subjects. Biomarkers were correlated with CMR markers.
Results
All subjects were asymptomatic at the time of enrollment. Several DMD subjects had transiently elevated cTnI. Those with elevated cTnI were more likely to have late gadolinium enhancement on baseline CMR. NT-proBNP correlated with indexed left ventricular end diastolic and maximum left atrial volumes. Otherwise, standard cardiac biomarkers did not correlate with CMR markers of cardiomyopathy.
Conclusions
CTnI, BNP, and NT-proBNP do not correlate with CMR assessment of cardiomyopathy progression. A subset of DMD patients have asymptomatic cTnI leak of uncertain clinical significance, though of critical importance if cTnI is used to assess for cardiac toxicity in future drug trials.
Impact
-
Asymptomatic patients with Duchenne muscular dystrophy (DMD) exhibit transient troponin I leak.
-
NT-proBNP correlated with indexed left ventricular end diastolic volume and indexed maximum left atrial volume.
-
Other cardiac biomarkers did not correlate with cardiac magnetic resonance (CMR) markers of cardiomyopathy.
Similar content being viewed by others
Introduction
Duchenne muscular dystrophy (DMD) affects 1 in 4700 live male births and leads to skeletal and cardiac myopathy.1 Patients with DMD are usually non-ambulatory by 10–13 years of age, but the development of overt cardiomyopathy is delayed, often occurring later in the second decade of life.2,3 Cardiomyopathy is the leading cause of death in the current era, and there has been an increased push to develop DMD-specific cardiac therapies.4,5,6,7 Due to their limited mobility, those with overt cardiomyopathy are usually asymptomatic until myocardial dysfunction is advanced.8 Symptoms often present as vague complaints of abdominal pain or general fatigue, but these symptoms often portend a poor prognosis.8 While imaging aids in the detection of left ventricular (LV) dysfunction and can guide therapy, disease progression can be variable, making it difficult to discern those most at risk of rapid advancement from those with a less rapidly progressive cardiomyopathic phenotype.
Pediatric and adult patients with other forms of dilated cardiomyopathy can pose the same dilemma in that patients with a similar degree of LV dysfunction may have vastly different symptoms and disease progression. In this situation, biomarkers such as brain natriuretic peptide (BNP) can help stratify degree of heart failure and predict mortality.9,10 Unfortunately, traditional biomarkers used in the assessment of DMD-associated heart failure have limited utility.11,12,13,14
Cardiac Troponin I (cTnI) is a basic protein of the troponin protein complex that plays an important role in diastolic relaxation through inhibition of actin–myosin-binding interaction.15 Cardiac myocyte damage leads to release of cTnI into the serum, allowing for measurement of serum cTnI concentrations as a surrogate for cardiac myocyte damage. The development of high-sensitivity troponin assays has improved detection thresholds for lower-level troponin leaks.16 cTnI has been shown to be elevated from baseline in a variety of disease states known to cause ischemic as well as non-ischemic mediated cardiac dysfunction.17,18,19,20,21 CTnI is not expressed in skeletal muscle in patients with DMD, negating the confounding factor of progressive skeletal muscle myositis that has affected the utility of other biomarkers.22
Given the increased emphasis on discovering new cardiac therapies in DMD, cTnI has been used in many studies to monitor for cardiotoxicity. While it is well established that patients with DMD can present with a myocarditis/dystrophinitis picture with cTnI elevation,23 there have also been limited reports of cTnI elevation in patients without clinical symptoms.24 The extent and severity of cTnI elevation in asymptomatic DMD patients is not fully understood, making interpretation of cTnI in drug toxicity studies difficult. A recent expert panel called for prospective, longitudinal evaluation of cTnI in the DMD population.25 The goal of this study was to longitudinally evaluate cTnI in an asymptomatic cohort of subjects with DMD. We also analyzed BNP, N-terminal proBNP (NT-proBNP), and creatine kinase-MB (CK-MB). We hypothesized that these biomarkers would not correlate well with cardiac function or mortality, but that some patients without clinical symptoms would exhibit a cTnI leak, reflecting ongoing myocardial damage related to disease progression.
Methods
Patient enrollment
The Vanderbilt Institutional Review Board approved this prospective study. Appropriate consents and assents were obtained as part of study enrollment. DMD subjects were enrolled from the Neuromuscular Cardiology Clinic. Inclusion criteria were: (1) diagnosis of DMD with clinical phenotype and confirmation with either genetic testing or muscle biopsy; (2) blood obtained at the time of cardiac magnetic resonance (CMR); (3) able to tolerate CMR without sedation or anesthesia. Exclusion criteria were: (1) additional cardiac diagnoses that could affect biomarkers, (2) renal dysfunction or other contraindication to magnetic resonance imaging (MRI) with contrast (3) inadequate volume of blood. Pertinent clinical data were collected from patients and from the electronic medical record. Enrolled DMD subjects underwent blood draw, CMR, and echocardiographic assessment.
Eighteen healthy males aged 8–18 years old with otherwise normal cardiac evaluation undergoing treadmill testing were enrolled as control subjects. Exclusion criteria were: (1) abnormal treadmill test, (2) presence or concern for structural or functional cardiovascular disease (congenital heart disease, cardiomyopathy, or any secondary cardiovascular disease), (3) abnormal echocardiogram, and (4) arrhythmia or clinical concern for arrhythmia. Reasons for treadmill testing included: chest pain, syncope, palpitations, and tachycardia. Control subjects only underwent biomarker analysis as part of this study. Control subjects were used to establish normal reference values for the specific biomarker assays.
Biomarker analysis
The Milliplex Map Human Cardiovascular Disease Panel 1 Magnetic Bead Kit (EMD Millipore Corporation, Billerica, MA, Cat # HCVD1MAG-67K) was used to detect plasma cTnI, BNP, NT-proBNP, and CK-MB according to the manufacturer’s instructions. Seven working standards were generated by serial dilution (1:3) of the reconstituted standard provided in the kit. Two QC (quality control) samples were included in each plate run. Assay plate was read on Luminex 200 with XPONENT software using the parameters outlined in the assay kit instructions. The Milliplex Analyst 5.0 software was used for data analysis. The correlation efficiency (R) for the standard curve was greater than 0.99 for each assay. All assays were run in duplicate, and the average %CV was less than 10%. Normal values were provided by Luminex; we also compared values to the mean and standard deviations of our control group. Enzyme-linked immunosorbent assay and Luminex samples were excluded if the coefficient of variation was greater than 25%. This resulted in exclusion of one cTnI and CK-MB value at the first visit, two cTnI values at the second visit, and one BNP value at the third visit.
Cardiac magnetic resonance
CMR was performed for DMD subjects using a 1.5 Tesla Siemens Avanto (Siemens Healthcare Sector, Erlangen, Germany). Balanced steady state free-precession (bSSFP) imaging was performed in a short axis stack for calculation of volumetrics. A peripheral intravenous line was used to administer Gd-DTPA contrast (gadopentate dimeglumine, Magnevist®; Bayer Healthcare Pharmaceuticals, Wayne, NJ) at a dose of 0.2 mmol/kg or gadobutrol (Gadavist, Bayer) at a dose of 0.15 mmol/kg. Late gadolinium enhancement (LGE) was assessed using single shot and segmented inversion recovery bSSFP with optimized inversion recovery to null the signal from the myocardium, and phase-sensitive inversion recovery bSSFP with an inversion time of 300 ms. Breath-held modified Look-Locker inversion recovery (MOLLI) sequences were performed prior to and 15 min after contrast administration at the mid-LV in the short axis plane.26,27 MOLLI sequences were motion-corrected, ECG-triggered images obtained in diastole with 5(3 s)3 pre-contrast and a 4(1)3(1)2 post-contrast.28 Motion correction as described by Xue et al.29 was performed and a T1 map was generated on the scanner.
LV and right ventricular (RV) volumetrics and function were calculated as previously described.30 Maximum and minimum LA volumes were calculated from four- and two-chamber cine imaging in QMass (Medis Medical Imaging Systems, Leiden, The Netherlands).31 The presence or absence of LGE, as well as location using the standard 17-segment model,32 was qualitatively assessed. Global severity score was reported as previously described.33 The score ranged from 0 (no LGE) to 4 (severe LGE). Semi-quantitative assessment of LGE was also performed using the full-width half-maximum technique in QMass (Medis). T1 and extracellular volume (ECV) maps were analyzed in QMaps (Medis). Regions of interest (ROIs) were manually drawn on T1 and ECV maps within the LV mesocardium, with ROIs carefully traced to avoid partial volume averaging.32 Based on the T1 mapping consensus statement, areas of LGE were included in the ROIs as these areas were felt to be the most focal areas in a continuum of diffuse ECM expansion.27,34 ECV was calculated using a hematocrit drawn the same day as the CMR as previously described.34 QStrain (Medis) was used to calculate feature tracking global longitudinal strain.
Statistical analysis
Demographic variables were compared using either a Wilcoxon rank-sum (continuous variables) or a Chi-square or Fisher’s exact test (categorical variables). Correlations between continuous variables were evaluated using Spearman’s rho. A Wilcoxon rank-sum was used to evaluate the difference in biomarker levels between control and DMD and to compare levels between DMD subjects with and without LGE. The Holm–Bonferroni method was used to correct for multiple comparisons and adjusted p values are reported. As the primary analyses were non-parametric, biomarker levels that were below or above detection levels were analyzed as half the lower level of detection or twice the upper level of detection. Analyses were performed using Stata, version 16.0 (College Station, TX: StataCorp). Study data were collected and managed using REDCap (Research Electronic Data Capture) electronic data capture tools hosted at Vanderbilt.35
Results
Demographics
Sixty-nine subjects with DMD and 18 controls were enrolled. Eight subjects with DMD were excluded due to inadequate sample volume to obtain biomarker levels. Fifty-eight patients had at least one cTnI level drawn, though only 55 had a cTnI level drawn at the initial visit. Patients had similar ages, race, and ethnicity. Subjects with DMD had significantly shorter stature and lower weight. Only 19 DMD subjects were ambulatory at the time of enrollment. The majority of DMD subjects were on a corticosteroid (57%) with additional medical therapies consisting of angiotensin-converting enzyme inhibitor (ACEi) (57%), angiotensin receptor blocker (ARB) (11%), and beta blockers (38%) (Table 1).
Baseline CMR characteristics
The mean left ventricular ejection fraction (LVEF) for DMD subjects by CMR was mildly decreased at 54%, with 38% of the population having an abnormal LVEF at baseline (defined as LVEF < 55%). LV volumes were normal with low LV mass. Myocardial LGE was present in 68% of the DMD subjects at baseline with a median global severity score of 1. The segmental pattern of LGE was consistent with more involvement of the free wall and the base and mid-LV.
Biomarker values compared to control population
There was no significant difference between mean cTnI levels in the DMD and control cohorts (Table 2). Normal values were derived from the control population.
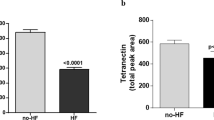
Based on a cut-off of 268 pg/ml, which represents the 99th percentile for cTnI levels as derived from the healthy cohort, five subjects (9%) had elevated cTnI at baseline, six (16%) had elevated cTnI at the second visit, and four (16%) had elevated cTnI at the third visit (Fig. 1). All DMD subjects had at least one normal cTnI. All controls were at or below the 99th percentile cut-off. There was also no difference between cTnI in DMD and control at visits 2 or 3 (p = 0.663, p = 0.155). Of note, all patients with cTnI > 268 pg/ml at the initial visit had LGE on their baseline CMR.
BNP values were not significantly different than controls at baseline or on follow-up visits. NT-proBNP was increased in DMD compared to controls at baseline, though it did not reach statistical significance (p = 0.10). NT-proBNP was significantly greater in the DMD subjects compared with controls at visits 2 and 3 (Table 2). CK-MB values were significantly increased in DMD subjects when compared to controls at all timepoints.
CTnI, BNP, and NT-proBNP levels did not change significantly over time. There was a significant increase in CK-MB levels from the first to third visits (Table 3). CK-MB levels did not change significantly from the first to second visits.
Biomarker correlation with CMR findings
There was no correlation in the entire DMD cohort between cTnI, BNP, or CK-MB and CMR function, LGE, ECV, or native T1 values (Table 4a). NT-proBNP correlated with indexed left ventricular end diastolic volume and indexed maximum left atrial volume at baseline.
Subgroup analysis showed no correlation between biomarkers studied and CMR markers in the ambulatory cohort (Table 4b). There were significant positive correlations in the non-ambulatory subgroup, but these no longer reached significance after correction for multiple comparisons (Table 4c). Although the medians within subgroups were not significantly different, the cTnI elevations occurred exclusively in the non-ambulatory subjects in their teenage years (Fig. 2a) and in subjects with normal to mildly depressed LVEF (Fig. 2b).
Subjects with elevated cTnI were more likely to have LGE present on baseline CMR, though this did not reach statistical significance (Table 5). Fifty-six percent of subjects with elevated cTnI at either of the first two visits had worsening of their LGE based on qualitative scoring on final MRI (N = 9), while 36.8% of those with normal cTnI values demonstrated worsening of LGE (p = 0.314). Sixty-seven percent of subjects with elevated cTnI at either of the first two visits had worsening of their LGE by FWHM on final MRI, while 52.6% of those with normal cTnI values demonstrated worsening LGE by FWHM (p = 0.457).
Discussion
This study is the first to evaluate cTnI, BNP, and NT-proBNP levels longitudinally in a relatively large asymptomatic DMD cohort. We have demonstrated that these biomarkers show no consistent correlation with measures of cardiac function obtained from CMR. Additionally, this study is the first to report that cTnI can fluctuate between normal and abnormal over time in a subset of asymptomatic patients with DMD. On average, patients with DMD do not have a baseline elevation of cTnI when compared to age-matched healthy male controls. There was no patient who had an elevated cTnI at all three visits. The non-ambulatory subgroup exhibits cTnI leak while cardiac function is preserved by CMR. After a period of presumed cardiomyocyte damage and reduction in cardiac function, there is no longer as significant of an asymptomatic leakage of cTnI. The correlation between NT-proBNP and both indexed LVEDV as well as maximum LA volume is likely due to atrial stretch. While NT-proBNP levels were higher in the DMD population than in controls, this is of uncertain clinical significance with no consistent correlation to measures of cardiac function.
Cardiac troponin isotypes are primarily thought to be released due to subendocardial ischemia, though elevated filling pressures, increased wall stress, endothelial dysfunction, arrhythmias, tachycardia, anemia, and hypotension may contribute.36,37 These factors lead to increased cardiomyocyte stretch and membrane permeability leading to cTn release from the cytosol.38,39 Increased wall stress leads to cardiomyocyte apoptosis releasing cTn.40,41 Inflammatory cytokines and neurohormones may be directly toxic to cardiomyocytes as proposed in stress-induced cardiomyopathy.42 Cardiac Troponin T has been shown to be chronically elevated in patients with skeletal myopathies without cardiac involvement. CTnI is rarely elevated in the absence of cardiac involvement in this same population.43
Variability and elevation of cTnI has also been described in hypertrophic cardiomyopathy (HCM). CTnI levels correlate with reduced GLS and increased LV thickness in the HCM population and are thought to be due to subendocardial ischemia from poor perfusion and elevated filling pressures. As our study has shown, patients with DMD have reduced LVEDV and mass. They also do not have the correlation of cTnI with LV thickness as in HCM and any elevated filling pressures would likely be persistent rather than episodic. Therefore, the mechanism leading to cTnI leak for patients with DMD may be unique, and likely related to the hypothesized recurrent myocardial injury related to loss of dystrophin.
Recent reports have suggested an association between cTnI levels and LGE as well as native T1 values in DMD.44 Our cohort did not show a consistent correlation between any of the cardiac biomarkers tested and a multitude of markers of cardiac function by CMR. We expect this may have been due to the different assays used for cTnI detection as well as our larger cohort. LGE may have also been graded differently between centers. There was a trend towards patients with elevated cTnI being more likely to have LGE present, though this was not statistically significant. However, a significant portion of patients with DMD who developed new LGE lesions did not have a corresponding abnormal cTnI, BNP, or NT-proBNP value during their follow-up period in our study. Most subjects with cTnI elevation demonstrated an increase in LGE at subsequent visits. While not all subjects with an increase in LGE at follow-up visits had elevated cTnI, these represent one moment in time and it would be reasonable to assume that those subjects had elevated cTnI due to myocardial damage at some point in the intervening time between visits. The worsening of LGE could also be indicative of scar burden from continued cardiomyocyte destruction not detected by the cardiac biomarkers used in this study.
The clinical progression of DMD is well documented as progressive decline in skeletal muscle function, followed by development of cardiomyopathy in the second decade of life and impaired respiratory function. While cardiorespiratory issues are the leading cause of death in patients with DMD, it has been suggested that after a period of decline in cardiac function there is a plateau and maintenance of a stable LVEF in late-stage DMD.45
Eight subjects had insufficient blood volumes for any biomarker analysis and were excluded from the study. There was also insufficient sample to obtain two cTnI and one NT-proBNP values at the third visit. Coefficient of variation was high in a small number of samples as well. These numbers combined may have decreased the power of the analysis resulting in significant associations remaining undetected. This seems unlikely as there were few significant correlations even before correction for multiple analyses.
Recent studies have shown that episodes of chest pain associated with ST segment changes on ECG and elevated cTnI, “dystrophinitis”, can present with acute reductions in LVEF.23 This information taken together with other studies43 would suggest that a certain subset of DMD patients will have clinical and subclinical episodes of acute cardiomyocyte destruction. These episodes of clinical and subclinical dystrophinitis may represent an early pathology in the process of cardiomyocyte destruction in the DMD population. CTnI may be more useful as a marker of these episodes of dystrophinitis characterized by severely elevated cTnI. The trend of cTnI in patients with this acute clinical presentation can aid in assessing efficacy of interventions. However, clinical intervention based on mild asymptomatic elevations of cTnI, as have been documented here, are likely not warranted as this likely represents progression of disease that is unlikely to be modified by therapy.
Given the variability in cTnI within the DMD population and the presence of these intermittent mild elevations, high-sensitivity cTnI assays are unlikely to be clinically useful. These intermittent, asymptomatic elevations should not be an immediate cause for concern of an acute toxicity or secondary cardiac insult. Because the mild cTnI leak likely represents the progression of the DMD pathology, we hypothesize that high-sensitivity cTnI would be less useful for drug toxicity monitoring for the same reason. However, this has not to our knowledge been evaluated in DMD and the research implications of high-sensitivity cTnI elevation warrant study.
Of note, this study evaluated one assay. Normative data derived from controls can only be used for that particular assay. Similarly, different centers often have different normative values for their cardiac biomarkers. For this reason, values from different centers may not be translatable, necessitating the use of a core laboratory with a consistent assay.
Limitations and future directions
Though this is the largest prospectively enrolled DMD cohort to date to be followed longitudinally, these subjects were enrolled with varying degrees of cardiac dysfunction at baseline. We suspect there were episodes of cardiomyocyte destruction and cTnI leak that were not detected between visits due to the relatively short half-life of cTnI in circulation.46) Future studies should investigate troponin degradation products that may be present in the circulation for a longer period of time. Evaluation of post-translational modification patterns of the cTnI released in the DMD population may also give a specific phenotype for the pathologic process occurring in DMD patients. Finally, multiple other biomarkers with potential to monitor DMD disease progression have been presented.47,48 As the goal of this manuscript was to assess standard cardiac biomarkers, we have not included an assessment of these more novel biomarkers, but future work should evaluate whether these biomarkers have a role in the assessment of drug toxicity.
Conclusions
CTnI is elevated in a small number of asymptomatic DMD subjects. Given the known pathogenesis of disease and the rapid clearance of cTnI, it is reasonable to suspect that all or most boys will have intermittent elevation of cTnI as they have ongoing myocardial damage. Studies planning to use cTnI for the assessment of drug cardiotoxicity should be aware of these intermittent elevations and understand that elevations may reflect progression of disease and not acute cardiotoxicity related to an investigational drug.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funding sources had no input into the study design, the collection, analysis, and interpretation of data, or the writing of the manuscript or decision to submit.
References
Dooley, J., Gordon, K. E., Dodds, L. & MacSween, J. Duchenne muscular dystrophy: a 30-year population-based incidence study. Clin. Pediatr. (Philos) 49, 177–179 (2010).
Boland, B. J., Silbert, P. L., Groover, R. V., Wollan, P. C. & Silverstein, M. D. Skeletal, cardiac, and smooth muscle failure in Duchenne muscular dystrophy. Pediatr. Neurol. 14, 7–12 (1996).
Nigro, G., Comi, L. I., Politano, L. & Bain, R. J. The incidence and evolution of cardiomyopathy in Duchenne muscular dystrophy. Int. J. Cardiol. 26, 271–277 (1990).
Bach, J. R. & Martinez, D. Duchenne muscular dystrophy: continuous noninvasive ventilatory support prolongs survival. Respir. Care 56, 744–750 (2011).
Van Ruiten, H. J. et al. Why are some patients with Duchenne muscular dystrophy dying young: an analysis of causes of death in North East England. Eur. J. Paediatr. Neurol. 20, 904–909 (2016).
Wittlieb-Weber, C. A. et al. Risk factors for cardiac and noncardiac causes of death in males with Duchenne muscular dystrophy. Pediatr. Cardiol. 41, 764–771 (2020).
Meyers, T. A. & Townsend, D. Cardiac pathophysiology and the future of cardiac therapies in Duchenne muscular dystrophy. Int. J. Mol. Sci. 20, 4098 (2019).
Wang, M., Birnkrant, D. J., Super, D. M., Jacobs, I. B. & Bahler, R. C. Progressive left ventricular dysfunction and long-term outcomes in patients with Duchenne muscular dystrophy receiving cardiopulmonary therapies. Open Heart 5, e000783 (2018).
Dao, Q. et al. Utility of B-type natriuretic peptide in the diagnosis of congestive heart failure in an urgent-care setting. J. Am. Coll. Cardiol. 37, 379–385 (2001).
Doust, J. A., Pietrzak, E., Dobson, A. & Glasziou, P. How well does B-type natriuretic peptide predict death and cardiac events in patients with heart failure: systematic review. Br. Med. J. 330, 625 (2005).
Demachi, J. et al. Characteristics of the increase in plasma brain natriuretic peptide level in left ventricular systolic dysfunction, associated with muscular dystrophy in comparison with idiopathic dilated cardiomyopathy. Neuromuscul. Disord. 14, 732–739 (2004).
van Bockel, E. A. et al. Cardiac assessment of patients with late stage Duchenne muscular dystrophy. Neth. Heart J. 17, 232–237 (2009).
Mohyuddin, T., Jacobs, I. B. & Bahler, R. C. B-type natriuretic peptide and cardiac dysfunction in Duchenne muscular dystrophy. Int. J. Cardiol. 119, 389–391 (2007).
Mori, K. et al. Plasma levels of natriuretic peptide and echocardiographic parameters in patients with Duchenne’s progressive muscular dystrophy. Pediatr. Cardiol. 23, 160–166 (2002).
Kobayashi, T. & Solaro, R. J. Calcium, thin filaments, and the integrative biology of cardiac contractility. Annu. Rev. Physiol. 67, 39–67 (2005).
Januzzi, J. L. et al. High-sensitivity Troponin T concentrations in acute chest pain patients evaluated with cardiac computed tomography. Circulation 121, 1227–1234 (2010).
Saiedi, S. A. E. et al. Left ventricular diastolic dysfunction without left ventricular hypertrophy in obese children and adolescents: a tissue Doppler imaging and Cardiac Troponin I Study. Cardiol. Young 28, 76–84 (2017).
Jones, M., O’Gorman, P., Kelly, C., Mahon, N. & Fitzgibbon, M. C. High-sensitive cardiac troponin-I facilitates timely detection of subclinical anthracycline-mediated cardiac injury. Ann. Clin. Biochem. 54, 149–157 (2017).
Zhang, C. et al. Predictive values of N-terminal Pro-B-type natriuretic peptide and cardiac Troponin I for myocardial fibrosis in hypertrophic obstructive cardiomyopathy. PLoS ONE 11 e0146572 (2016).
Agarwal, A. et al. Relationship of cardiac troponin to systolic global longitudinal strain in hypertrophic cardiomyopathy. Echocardiography 34, 1470–1477 (2017).
Horwich, T. B., Patel, J., Maclellan, W. R. & Fonarow, G. C. Cardiac Troponin I is associated with impaired hemodynamics, progressive left ventricular dysfunction, and increased mortality rates in advanced heart failure. Circulation 108, 833–838 (2003).
Bodor, G. S., Porterfield, D., Voss, E. M., Smith, S. & Apple, F. S. Cardiac troponin-I is not expressed in fetal and healthy or diseased adult human skeletal muscle tissue. Clin. Chem. 41, 1710–1715 (1995).
Hor, K. N. et al. Progression of Duchenne cardiomyopathy presenting with chest pain and Troponin elevation. J. Neuromuscul. Dis. 4, 307–314 (2017).
Matsumura, T., Saito, T., Fujimura, H. & Shinno, S. Cardiac troponin I for accurate evaluation of cardiac status in myopathic patients. Brain Dev. 29, 496–501 (2007).
Spurney, C. F. et al. Current state of cardiac troponin testing in Duchenne muscular dystrophy cardiomyopathy: review and recommendations from the Parent Project Muscular Dystrophy expert panel. Open Heart (2021).
Messroghli, D. R. et al. Modified Look-Locker inversion recovery (MOLLI) for high-resolution T1 mapping of the heart. Magn. Reson. Med. 52, 141–146 (2004).
Moon, J. C. et al. Myocardial T1 mapping and extracellular volume quantification: a Society for Cardiovascular Magnetic Resonance (SCMR) and CMR Working Group of the European Society of Cardiology consensus statement. J. Cardiovasc. Magn. Reson. 15, 92 (2013).
Kellman, P. & Hansen, M. S. T1-mapping in the heart: accuracy and precision. J. Cardiovasc. Magn. Reson. 16, 2 (2014).
Xue, H. et al. Motion correction for myocardial T1 mapping using image registration with synthetic image estimation. Magn. Reson. Med. 67, 1644–1655 (2012).
Soslow, J. H. et al. Evaluation of post-contrast myocardial t1 in Duchenne muscular dystrophy using cardiac magnetic resonance imaging. Pediatr. Cardiol. 36, 49–56 (2015).
Dodson, J. A. et al. Left atrial passive emptying function determined by cardiac magnetic resonance predicts atrial fibrillation recurrence after pulmonary vein isolation. Circ. Cardiovasc. Imaging 7, 586–592 (2014 Jul).
Cerqueira, M. D. et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 105, 539–542 (2002).
Soslow, J. H. et al. The role of matrix metalloproteinases and tissue inhibitors of metalloproteinases in Duchenne muscular dystrophy cardiomyopathy. J. Card. Fail 25, 259–267 (2019).
Messroghli, D. R. et al. Modified Look-Locker inversion recovery (MOLLI) for high-resolution T1 mapping of the heart. Magn. Reson. Med. 52, 141–146 (2004).
Harris, P. A. et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inf. 42, 377–381 (2009).
Kociol, R. D. et al. Troponin elevation in heart failure prevalence, mechanisms, and clinical implications. J. Am. Coll. Cardiol. 56, 1071–1078 (2010).
Januzzi, J. L. Jr, Filippatos, G., Nieminen, M. & Gheorghiade, M. Troponin elevation in patients with heart failure: on behalf of the third Universal Definition of Myocardial Infarction Global Task Force: Heart Failure Section. Eur. Heart J. 33, 2265–2271 (2012).
Hessel, M. H. et al. Release of cardiac troponin I from viable cardiomyocytes is mediated by integrin stimulation. Pflug. Arch. 455, 979–986 (2008).
Sato, Y., Kita, T., Takatsu, Y. & Kimura, T. Biochemical markers of myocyte injury in heart failure. Heart 90, 1110–1113 (2004).
Narula, J. et al. Apoptosis in myocytes in end-stage heart failure. N. Engl. J. Med. 335, 1182–1189 (1996).
Labugger, R. et al. Extensive troponin I and T modification detected in serum from patients with acute myocardial infarction. Circulation 102, 1221–1226 (2000).
Lyon, A. R. et al. Stress (Takotsubo) cardiomyopathy—a novel pathophysiological hypothesis to explain catecholamine-induced acute myocardial stunning. Nat. Clin. Pract. Cardiovasc. Med. 5, 22–29 (2008).
Schmid, J. et al. Elevated cardiac troponin T in patients with skeletal myopathies. J. Am. Coll. Cardiol. 71, 1540–1549 (2018).
Voleti, S. et al. Levels correlate with cardiac MR LGE and native T1 values in duchenne muscular dystrophy cardiomyopathy and identify early disease progression. Pediatr. Cardiol. 41, 1173–1179 (2020).
Kwon, S. W. et al. Outcomes of cardiac involvement in patients with late-stage Duchenne muscular dystrophy under management in the pulmonary rehabilitation center of a tertiary referral hospital. Cardiology 121, 186–193 (2012).
Gerhardt, W. et al. S-troponin T in suspected ischemic myocardial injury compared with mass and catalytic concentrations of S-creatine kinase isoenzyme MB. Clin. Chem. 37, 1405–1411 (1991).
Anderson, J., Seol, H., Gordish-Dressman, H., Hathout, Y., Spurney, C. F. & CINRG Investigators. Interleukin 1 Receptor-Like 1 Protein (ST2) is a potential biomarker for cardiomyopathy in Duchenne muscular dystrophy. Pediatr. Cardiol. 38, 1606–1612 (2017).
Soslow, J. H. et al. The role of matrix metalloproteinases and tissue inhibitors of metalloproteinases in Duchenne muscular dystrophy cardiomyopathy. J. Card. Fail. 25, 259–267 (2019).
Funding information
Research reported in this publication was supported the Fighting Duchenne Foundation and the Fight DMD/Jonah & Emory Discovery Grant (Markham) (Nashville, TN), the National Heart, Lung, and Blood Institute of the National Institutes of Health under Award Numbers K23HL123938 and R56HL141248 (Soslow), K01HL121045 (Galindo), K08HL155852 (Raucci), and 5T32HL105334-10 (Baldwin) (Bethesda, MD), the Eunice Kennedy Shriver National Institute of Child Health and Human Development Award Number K12HD087023 (Raucci) (Bethesda, MD), the Food and Drug Administration Orphan Products Grant R01FD006649 (Soslow) (Silver Spring, MD), and the National Center for Advancing Translational Sciences, Grant 2 UL1 TR000445-06 (Bethesda, MD).
Author information
Authors and Affiliations
Contributions
J.H.S. and A.S. were responsible for conception and design of the study, acquisition, analysis, and interpretation of data as well as drafting the article. L.W.M. contributed to conception and design of the study as well as revision and final approval of the article. K.C., F.J.R., and W.B.B. contributed to acquisition of data and revision of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
Appropriate consents and assents were obtained as part of study enrollment.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sheybani, A., Crum, K., Raucci, F.J. et al. Duchenne muscular dystrophy patients: troponin leak in asymptomatic and implications for drug toxicity studies. Pediatr Res 92, 1613–1620 (2022). https://doi.org/10.1038/s41390-021-01682-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01682-5
This article is cited by
-
N-terminal titin fragment: a non-invasive, pharmacodynamic biomarker for microdystrophin efficacy
Skeletal Muscle (2024)
-
Successful treatment of acute myocardial injury of Duchenne muscular dystrophy with steroids: a case report
Journal of Cardiothoracic Surgery (2023)