Abstract
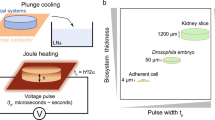
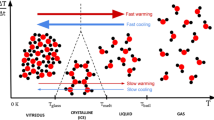
The three classical core technologies for the preservation of live mammalian biospecimens—slow freezing, vitrification and hypothermic storage—limit the biomedical applications of biospecimens. In this Review, we summarize the principles and procedures of these three technologies, highlight how their limitations are being addressed via the combination of microfabrication and nanofabrication, materials science and thermal-fluid engineering and discuss the remaining challenges.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$99.00 per year
only $8.25 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Fischbach, M. A., Bluestone, J. A. & Lim, W. A. Cell-based therapeutics: the next pillar of medicine. Sci. Transl Med. 5, 179ps177 (2013).
Singh, V. K., Kalsan, M., Kumar, N., Saini, A. & Chandra, R. Induced pluripotent stem cells: applications in regenerative medicine, disease modeling, and drug discovery. Front. Cell Dev. Biol. 3, 2 (2015).
Campbell, L. D. et al. Development of the ISBER best practices for repositories: collection, storage, retrieval and distribution of biological materials for research. Biopreserv. Biobank. 10, 232–233 (2012).
Jing, L., Yao, L., Zhao, M., Peng, L.-P. & Liu, M. Organ preservation: from the past to the future. Acta Pharmacol. Sin. 39, 845–857 (2018).
Massarotti, C. et al. State of the art on oocyte cryopreservation in female cancer patients: a critical review of the literature. Cancer Treat. Rev. 57, 50–57 (2017).
Giwa, S. et al. The promise of organ and tissue preservation to transform medicine. Nat. Biotechnol. 35, 530–542 (2017).
Organ Donation Statistics. (Health Resources & Services Administration, 2019); https://www.organdonor.gov/statistics-stories/statistics.html
Evans, R. W. in Xenotransplantation (ed. Platt, J. L.) 29–51 (2000).
Aijaz, A. et al. Biomanufacturing for clinically advanced cell therapies. Nat. Biomed. Eng. 2, 362–376 (2018).
Yong, K. W. et al. Cryopreservation of human mesenchymal stem cells for clinical applications: current methods and challenges. Biopreserv. Biobank. 13, 231–239 (2015).
Chi, H.-J. et al. Cryopreservation of human embryos using ethylene glycol in controlled slow freezing. Hum. Reprod. 17, 2146–2151 (2002).
Pegg, D. E. Principles of cryopreservation. Methods Mol. Biol. 368, 39–57 (2007).
Fuller, B. et al. Applications and optimization of cryopreservation technologies to cellular therapeutics. Cell Gene Ther. Insights 3, 359–378 (2017).
Rezazadeh Valojerdi, M., Eftekhari-Yazdi, P., Karimian, L., Hassani, F. & Movaghar, B. Vitrification versus slow freezing gives excellent survival, post warming embryo morphology and pregnancy outcomes for human cleaved embryos. J. Assist. Reprod. Genet. 26, 347–354 (2009).
Glujovsky, D. et al. Vitrification versus slow freezing for women undergoing oocyte cryopreservation. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD010047.pub2 (2014).
Shi, Q., Xie, Y., Wang, Y. & Li, S. Vitrification versus slow freezing for human ovarian tissue cryopreservation: a systematic review and meta-anlaysis. Sci. Rep. 7, 8538 (2017).
Rall, W. F. & Fahy, G. M. Ice-free cryopreservation of mouse embryos at −196 °C by vitrification. Nature 313, 573–575 (1985).
He, X. M., Park, E. Y. H., Fowler, A., Yarmush, M. L. & Toner, M. Vitrification by ultra-fast cooling at a low concentration of cryoprotectants in a quartz micro-capillary: a study using murine embryonic stem cells. Cryobiology 56, 223–232 (2008).
Gain, P. et al. Global survey of corneal transplantation and eye banking. JAMA Ophthalmol. 134, 167–173 (2016).
Guarrera, J. V. et al. Hypothermic machine preservation facilitates successful transplantation of ‘orphan’ extended criteria donor livers. Am. J. Transpl. 15, 161–169 (2015).
Wang, W., Penland, L., Gokce, O., Croote, D. & Quake, S. R. High fidelity hypothermic preservation of primary tissues in organ transplant preservative for single cell transcriptome analysis. BMC Genomics 19, 140 (2018).
Coutts, M., Hinton, S., Zheng, J. & Scharp, D. W. Hypothermic storage and preservation of human pancreatic acinar tissue. Vitr. Cell Dev. Biol. Anim. 43, 2–6 (2007).
Elliott, G. D., Wang, S. & Fuller, B. J. Cryoprotectants: a review of the actions and applications of cryoprotective solutes that modulate cell recovery from ultra-low temperatures. Cryobiology 76, 74–91 (2017).
Bhattacharya, M. S. A review on cryoprotectant and its modern implication in cryonics. Asian J. Pharm. https://doi.org/10.22377/ajp.v10i3.721 (2016).
Akiyama, Y., Shinose, M., Watanabe, H., Yamada, S. & Kanda, Y. Cryoprotectant-free cryopreservation of mammalian cells by superflash freezing. Proc. Natl Acad. Sci. USA 116, 7738–7743 (2019).
Mazur, P. Freezing of living cells: mechanisms and implications. Am. J. Physiol. 247, C125–C142 (1984).
He, X. Thermostability of biological systems: fundamentals, challenges, and quantification. Open Biomed. Eng. J. 5, 47–73 (2011).
Gardner, D. K., Lane, M., Stevens, J. & Schoolcraft, W. B. Changing the start temperature and cooling rate in a slow-freezing protocol increases human blastocyst viability. Fertil. Steril. 79, 407–410 (2003).
Jang, T. H. et al. Cryopreservation and its clinical applications. Integr. Med. Res. 6, 12–18 (2017).
Mahadevan, M. & Trounson, A. O. Effect of cooling, freezing and thawing rates and storage conditions on preservation of human spermatozoa. Andrologia 16, 52–60 (1984).
Dumont, F., Marechal, P.-A. & Gervais, P. Cell size and water permeability as determining factors for cell viability after freezing at different cooling rates. Appl. Environ. Microbiol. 70, 268–272 (2004).
Best, B. P. Cryoprotectant toxicity: facts, issues, and questions. Rejuvenation Res. 18, 422–436 (2015).
Karlsson, J. O., Szurek, E. A., Higgins, A. Z., Lee, S. R. & Eroglu, A. Optimization of cryoprotectant loading into murine and human oocytes. Cryobiology 68, 18–28 (2014).
Davidson, A. F., Glasscock, C., McClanahan, D. R., Benson, J. D. & Higgins, A. Z. Toxicity minimized cryoprotectant addition and removal procedures for adherent endothelial cells. PLoS ONE 10, e0142828 (2015).
Peyridieu, J. F. et al. Critical cooling and warming rates to avoid ice crystallization in small pieces of mammalian organs permeated with cryoprotective agents. Cryobiology 33, 436–446 (1996).
Seki, S. & Mazur, P. The dominance of warming rate over cooling rate in the survival of mouse oocytes subjected to a vitrification procedure. Cryobiology 59, 75–82 (2009).
Huang, H. et al. Predehydration and ice seeding in the presence of trehalose enable cell cryopreservation. ACS Biomater. Sci. Eng. 3, 1758–1768 (2017).
Southard, J. H., Senzig, K. A. & Belzer, F. O. Effects of hypothermia on canine kidney mitochondria. Cryobiology 17, 148–153 (1980).
Usta, O. B. et al. Supercooling as a viable non-freezing cell preservation method of rat hepatocytes. PLoS ONE 8, e69334 (2013).
Colletti, L. M. et al. The production of tumor necrosis factor alpha and the development of a pulmonary capillary injury following hepatic ischemia/reperfusion. Transplantation 49, 268–272 (1990).
Strüber, M. et al. Inhaled nitric oxide as a prophylactic treatment against reperfusion injury of the lung. Thorac. Cardiovasc. Surg. 47, 179–182 (1999).
Hausenloy, D. J. & Yellon, D. M. Ischaemic conditioning and reperfusion injury. Nat. Rev. Cardiol. 13, 193–209 (2016).
Koyama, I., Bulkley, G. B., Williams, G. M. & Im, M. J. The role of oxygen free radicals in mediating the reperfusion injury of cold-preserved ischemic kidneys. Transplantation 40, 590–595 (1985).
Ferng, A. S. et al. Novel vs clinical organ preservation solutions: improved cardiac mitochondrial protection. J. Cardiothorac. Surg. 12, 7 (2017).
Wekerle, T., Segev, D., Lechler, R. & Oberbauer, R. Strategies for long-term preservation of kidney graft function. Lancet 389, 2152–2162 (2017).
Tomalty, H. E. et al. Kidney preservation at subzero temperatures using a novel storage solution and insect ice-binding proteins. Cryo Lett. 38, 100 (2017).
Casula, E. et al. Osmotic behaviour of human mesenchymal stem cells: implications for cryopreservation. PLoS ONE 12, e0184180 (2017).
Ross-Rodriguez, L. U., Elliott, J. A. & McGann, L. E. Characterization of cryobiological responses in tf-1 cells using interrupted freezing procedures. Cryobiology 60, 106–116 (2010).
Casula, E., Asuni, G. P., Sogos, V. & Cincotti, A. hMSCs from UCB: isolation, characterization and determination of osmotic properties for optimal cryopreservation. Chem. Eng. Trans. 43, 265–270 (2015).
Ebertz, S. L. & McGann, L. E. Osmotic parameters of cells from a bioengineered human corneal equivalent and consequences for cryopreservation. Cryobiology 45, 109–117 (2002).
Chen, H. H., Purtteman, J. J., Heimfeld, S., Folch, A. & Gao, D. Development of a microfluidic device for determination of cell osmotic behavior and membrane transport properties. Cryobiology 55, 200–209 (2007).
Niu, D., Zhao, G., Liu, X., Zhou, P. & Cao, Y. Prevention of osmotic injury to human umbilical vein endothelial cells for biopreservation: a first step toward biobanking of endothelial cells for vascular tissue engineering. Tissue Eng. Part C Methods 22, 270–279 (2016).
Chen, H.-h et al. A microfluidic study of mouse dendritic cell membrane transport properties of water and cryoprotectants. Int. J. Heat. Mass Transf. 51, 5687–5694 (2008).
Tseng, H. Y. et al. A microfluidic study of megakaryocytes membrane transport properties to water and dimethyl sulfoxide at suprazero and subzero temperatures. Biopreserv. Biobank. 9, 355–362 (2011).
Liu, W. et al. High-precision approach based on microfluidic perfusion chamber for quantitative analysis of biophysical properties of cell membrane. Int. J. Heat. Mass Transf. 86, 869–879 (2015).
Lyu, S.-R., Chen, W.-J. & Hsieh, W.-H. Measuring transport properties of cell membranes by a PDMS microfluidic device with controllability over changing rate of extracellular solution. Sens. Actuators B 197, 28–34 (2014).
Berthier, E. et al. Kit-on-a-lid-assays for accessible self-contained cell assays. Lab Chip 13, 424–431 (2013).
Li, L., Lv, X., Guo, H., Shi, X. & Liu, J. On-chip direct freezing and thawing of mammalian cells. RSC Adv. 4, 34443–34447 (2014).
Deutsch, M. et al. The individual-cell-based cryo-chip for the cryopreservation, manipulation and observation of spatially identifiable cells. I: methodology. BMC Cell Biol. 11, 54 (2010).
Afrimzon, E. et al. The individual-cell-based cryo-chip for the cryopreservation, manipulation and observation of spatially identifiable cells. II: functional activity of cryopreserved cells. BMC Cell Biol. 11, 83 (2010).
Roach, K. L. et al. High-throughput single cell arrays as a novel tool in biopreservation. Cryobiology 58, 315–321 (2009).
Zou, Y., Yin, T., Chen, S., Yang, J. & Huang, W. On-chip cryopreservation: a novel method for ultra-rapid cryoprotectant-free cryopreservation of small amounts of human spermatozoa. PLoS ONE 8, e61593 (2013).
Li, S., Liu, W. & Lin, L. On-chip cryopreservation of living cells. J. Assoc. Lab. Autom. 15, 99–106 (2010).
Bissoyi, A., Bit, A., Singh, B. K., Singh, A. K. & Patra, P. K. Enhanced cryopreservation of MSCs in microfluidic bioreactor by regulated shear flow. Sci. Rep. 6, 35416 (2016).
Yang, G., Zhang, A., Xu, L. X. & He, X. Modeling the cell-type dependence of diffusion-limited intracellular ice nucleation and growth during both vitrification and slow freezing. J. Appl. Phys. 105, 114701 (2009).
Karlsson, J., Cravalho, E. & Toner, M. A model of diffusion‐limited ice growth inside biological cells during freezing. J. Appl. Phys. 75, 4442–4455 (1994).
Kawata, T. et al. Water molecule movement by a magnetic field in freezing for tooth banking. Biomed. Res. 21, 351–354 (2010).
Kaku, M. et al. Cryopreservation of periodontal ligament cells with magnetic field for tooth banking. Cryobiology 61, 73–78 (2010).
Abedini, S. et al. Effects of cryopreservation with a newly-developed magnetic field programmed freezer on periodontal ligament cells and pulp tissues. Cryobiology 62, 181–187 (2011).
Lee, S. Y. et al. Magnetic cryopreservation for dental pulp stem cells. Cells Tissues Organs 196, 23–33 (2012).
Conde, M. C. M. et al. Does cryopreservation affect the biological properties of stem cells from dental tissues? A systematic review. Braz. Dent. J. 27, 633–640 (2016).
Otero, L., Rodríguez, A. C., Pérez‐Mateos, M. & Sanz, P. D. Effects of magnetic fields on freezing: application to biological products. Compr. Rev. Food Sci. Food Saf. 15, 646–667 (2016).
Meng, L. et al. Development of a microfluidic device for automated vitrification human embryo. Fertil. Steril. 96, S207 (2011).
Heo, Y. S. et al. Controlled loading of cryoprotectants (CPAS) to oocyte with linear and complex CPA profiles on a microfluidic platform. Lab Chip 11, 3530–3537 (2011).
Song, Y. S. et al. Microfluidics for cryopreservation. Lab Chip 9, 1874–1881 (2009).
Lai, D., Ding, J., Smith, G. W., Smith, G. D. & Takayama, S. Slow and steady cell shrinkage reduces osmotic stress in bovine and murine oocyte and zygote vitrification. Hum. Reprod. 30, 37–45 (2015).
Swain, J. E., Lai, D., Takayama, S. & Smith, G. D. Thinking big by thinking small: application of microfluidic technology to improve art. Lab Chip 13, 1213–1224 (2013).
Zhao, G. & Fu, J. Microfluidics for cryopreservation. Biotechnol. Adv. 35, 323–336 (2017).
Zhang, W., Yang, G., Zhang, A., Xu, L. X. & He, X. Preferential vitrification of water in small alginate microcapsules significantly augments cell cryopreservation by vitrification. Biomed. Microdevices 12, 89–96 (2010).
Huang, H. et al. Alginate hydrogel microencapsulation inhibits devitrification and enables large-volume low-CPA cell vitrification. Adv. Funct. Mater. 25, 6939–6850 (2015).
Zhao, G., Liu, X., Zhu, K. & He, X. Hydrogel encapsulation facilitates rapid-cooling cryopreservation of stem cell-laden core-shell microcapsules as cell-biomaterial constructs. Adv. Healthc. Mater. 6, 1700988 (2017).
Chen, W., Shu, Z., Gao, D. & Shen, A. Q. Sensing and sensibility: single-islet-based quality control assay of cryopreserved pancreatic islets with functionalized hydrogel microcapsules. Adv. Health. Mater. 5, 223–231 (2016).
Cagol, N., Bonani, W., Maniglio, D., Migliaresi, C. & Motta, A. Effect of cryopreservation on cell-laden hydrogels: comparison of different cryoprotectants. Tissue Eng. Part C Methods 24, 20–31 (2018).
Lan, D. et al. Using a novel supramolecular gel cryopreservation system in microchannel to minimize the cell injury. Langmuir 34, 5088–5096 (2018).
Zhang, C. et al. Hydrogel cryopreservation system: an effective method for cell storage. Int. J. Mol. Sci. 19, 3330 (2018).
Huang, H. & He, X. in Multiscale Technologies for Cryomedicine: Implementation from Nano to Macroscale (eds He, X. & Bischof, J. C.) Ch. 4 (2016).
Demirci, U. & Montesano, G. Cell encapsulating droplet vitrification. Lab Chip 7, 1428–1433 (2007).
Kim, B.-H. et al. Effect of droplet vitrification on mitochondrial membrane potential and developmental competence in two-cell mouse embryos. Anim. Cells Syst. 15, 287–294 (2011).
An, L. et al. Efficient cryopreservation of mouse embryos by modified droplet vitrification (MDV). Cryobiology 71, 70–76 (2015).
Zhang, X. et al. Nanoliter droplet vitrification for oocyte cryopreservation. Nanomedicine 7, 553–564 (2012).
Samot, J. et al. Blood banking in living droplets. PLoS ONE 6, e17530 (2011).
Song, Y. S. et al. Vitrification and levitation of a liquid droplet on liquid nitrogen. Proc. Natl Acad. Sci. USA 107, 4596–4600 (2010).
de Vries, R. J. et al. Bulk droplet vitrification: an approach to improve large-scale hepatocyte cryopreservation outcome. Langmuir 35, 7354–7363 (2019).
Tedder, R. S. et al. Hepatitis B transmission from contaminated cryopreservation tank. Lancet 346, 137–140 (1995).
Grout, B. W. W. & Morris, G. Contaminated liquid nitrogen vapour as a risk factor in pathogen transfer. Theriogenology 71, 1079–1082 (2009).
Kuleshova, L. & Shaw, J. M. A strategy for rapid cooling of mouse embryos within a double straw to eliminate the risk of contamination during storage in liquid nitrogen. Hum. Reprod. 15, 2604–2609 (2000).
Shi, M. et al. High-throughput non-contact vitrification of cell-laden droplets based on cell printing. Sci. Rep. 5, 17928 (2015).
Marković, Z., Chatelet, P., Sylvestre, I., Kontić, J. & Engelmann, F. Cryopreservation of grapevine (Vitis vinifera L.) in vitro shoot tips. Open Life Sci. 8, 993–1000 (2013).
Bi, W.-L., Hao, X.-Y., Cui, Z.-H., Volk, G. M. & Wang, Q.-C. Droplet-vitrification cryopreservation of in vitro-grown shoot tips of grapevine (Vitis spp.). In Vitro Cell. Dev. Biol. Plant 54, 590–599 (2018).
Souza, F. V. D. et al. Droplet-vitrification and morphohistological studies of cryopreserved shoot tips of cultivated and wild pineapple genotypes. Plant Cell Tissue Organ Cult. 124, 351–360 (2016).
Jin, B., Kleinhans, F. W. & Mazur, P. Survivals of mouse oocytes approach 100% after vitrification in 3-fold diluted media and ultra-rapid warming by an IR laser pulse. Cryobiology 68, 419–430 (2014).
Khosla, K., Wang, Y., Hagedorn, M., Qin, Z. & Bischof, J. Gold nanorod induced warming of embryos from the cryogenic state enhances viability. ACS Nano 11, 7869–7878 (2017).
Robinson, M. P., Wusteman, M. C., Wang, L. & Pegg, D. E. Electromagnetic re-warming of cryopreserved tissues: effect of choice of cryoprotectant and sample shape on uniformity of heating. Phys. Med. Biol. 47, 2311–2325 (2002).
Manuchehrabadi, N. et al. Improved tissue cryopreservation using inductive heating of magnetic nanoparticles. Sci. Transl. Med. 9, eaah4586 (2017).
Wang, J., Zhao, G., Zhang, Z., Xu, X. & He, X. Magnetic induction heating of superparamagnetic nanoparticles during rewarming augments the recovery of hUCM-MSCs cryopreserved by vitrification. Acta Biomater. 33, 264–274 (2016).
Eskandari, N., Marquez-Curtis, L. A., McGann, L. E. & Elliott, J. A. W. Cryopreservation of human umbilical vein and porcine corneal endothelial cell monolayers. Cryobiology 85, 63–72 (2018).
Jomha, N. M. et al. Vitrification of intact human articular cartilage. Biomaterials 33, 6061–6068 (2012).
Vogel, T., Brockmann, J. G., Coussios, C. & Friend, P. J. The role of normothermic extracorporeal perfusion in minimizing ischemia reperfusion injury. Transplant. Rev. 26, 156–162 (2012).
Ravikumar, R., Leuvenink, H. & Friend, P. J. Normothermic liver preservation: a new paradigm? Transpl. Int. 28, 690–699 (2015).
Messer, S., Ardehali, A. & Tsui, S. Normothermic donor heart perfusion: current clinical experience and the future. Transpl. Int. 28, 634–642 (2015).
Cypel, M. et al. Normothermic ex vivo lung perfusion in clinical lung transplantation. N. Engl. J. Med. 364, 1431–1440 (2011).
Van Raemdonck, D., Neyrinck, A., Cypel, M. & Keshavjee, S. Ex-vivo lung perfusion. Transpl. Int. 28, 643–656 (2015).
Cypel, M. et al. Normothermic ex vivo perfusion prevents lung injury compared to extended cold preservation for transplantation. Am. J. Transplant. 9, 2262–2269 (2009).
Nasralla, D. et al. A randomized trial of normothermic preservation in liver transplantation. Nature 557, 50–56 (2018).
St Peter, S. D., Imber, C. J., Lopez, I., Hughes, D. & Friend, P. J. Extended preservation of non-heart-beating donor livers with normothermic machine perfusion. Br. J. Surg. 89, 609–616 (2002).
Xu, H. et al. Excorporeal normothermic machine perfusion resuscitates pig DCD livers with extended warm ischemia. J. Surg. Res. 173, e83–e88 (2012).
Eshmuminov, D. et al. An integrated perfusion machine preserves injured human livers for 1 week. Nat. Biotechnol. 38, 189–198 (2020).
Berendsen, T. A. et al. A simplified subnormothermic machine perfusion system restores ischemically damaged liver grafts in a rat model of orthotopic liver transplantation. Transpl. Res. 1, 6 (2012).
Tolboom, H. et al. Subnormothermic machine perfusion at both 20 °C and 30 °C recovers ischemic rat livers for successful transplantation. J. Surg. Res. 175, 149–156 (2012).
Bruinsma, B. G. et al. Subnormothermic machine perfusion for ex vivo preservation and recovery of the human liver for transplantation. Am. J. Transpl. 14, 1400–1409 (2014).
Bruinsma, B. G. et al. Metabolic profiling during ex vivo machine perfusion of the human liver. Sci. Rep. 6, 22415 (2016).
Berendsen, T. A. et al. Supercooling enables long-term transplantation survival following 4 days of liver preservation. Nat. Med. 20, 790–793 (2014).
Guarrera, J. V. et al. Hypothermic machine preservation in human liver transplantation: the first clinical series. Am. J. Transpl. 10, 372–381 (2010).
Moers, C. et al. Machine perfusion or cold storage in deceased-donor kidney transplantation. N. Engl. J. Med. 360, 7–19 (2009).
Moers, C., Pirenne, J., Paul, A., Ploeg, R. J. & Machine Preservation Trial Study Group. Machine perfusion or cold storage in deceased-donor kidney transplantation. N. Engl. J. Med. 366, 770–771 (2012).
Hoyer, D. P. et al. Controlled oxygenated rewarming of cold stored livers prior to transplantation: first clinical application of a new concept. Transplantation 100, 147–152 (2016).
Hoyer, D. P., Paul, A. & Minor, T. Prediction of hepatocellular preservation injury immediately before human liver transplantation by controlled oxygenated rewarming. Transplant. Direct https://doi.org/10.1097/TXD.0000000000000636 (2017).
Schopp, I., Reissberg, E., Luer, B., Efferz, P. & Minor, T. Controlled rewarming after hypothermia: adding a new principle to renal preservation. Clin. Transl. Sci. 8, 475–478 (2015).
Bruinsma, B. G. et al. Supercooling preservation and transplantation of the rat liver. Nat. Protoc. 10, 484–494 (2015).
Robinson, W. R., Peters, R. H. & Zimmermann, J. The effects of body size and temperature on metabolic rate of organisms. Can. J. Zool. 61, 281–288 (1983).
Belzer, F. O. & Southard, J. H. Principles of solid-organ preservation by cold storage. Transplantation 45, 673–676 (1988).
Weeder, P. D., van Rijn, R. & Porte, R. J. Machine perfusion in liver transplantation as a tool to prevent non-anastomotic biliary strictures: rationale, current evidence and future directions. J. Hepatol. 63, 265–275 (2015).
de Perrot, M. et al. Report of the ISHLT working group on primary lung graft dysfunction part III: donor-related risk factors and markers. J. Heart Lung Transpl. 24, 1460–1467 (2005).
Snyder, K. K., Baust, J. M., Van Buskirk, R. G. & Baust, J. G. Enhanced hypothermic storage of neonatal cardiomyocytes. Cell Preserv. Technol. 3, 61–74 (2005).
Pogozhykh, D., Prokopyuk, V., Pogozhykh, O., Mueller, T. & Prokopyuk, O. Influence of factors of cryopreservation and hypothermic storage on survival and functional parameters of multipotent stromal cells of placental origin. PLoS ONE 10, e0139834 (2015).
Correia, C. et al. Effective hypothermic storage of human pluripotent stem cell-derived cardiomyocytes compatible with global distribution of cells for clinical applications and toxicology testing. Stem Cells Transl. Med 5, 658–669 (2016).
Groger, M. et al. Preservation of cell structure, metabolism, and biotransformation activity of liver-on-chip organ models by hypothermic storage. Adv. Healthc. Mater. 7, 1700616 (2018).
Xu, Y., Mawatari, K., Konno, T., Kitamori, T. & Ishihara, K. Spontaneous packaging and hypothermic storage of mammalian cells with a cell-membrane-mimetic polymer hydrogel in a microchip. ACS Appl. Mater. Interfaces 7, 23089–23097 (2015).
Southard, J. H. & Belzer, F. O. Organ preservation. Annu. Rev. Med. 46, 235–247 (1995).
McAnulty, J. F. Hypothermic organ preservation by static storage methods: current status and a view to the future. Cryobiology 60, S13–S19 (2010).
Puts, C. F. et al. Polyethylene glycol protects primary hepatocytes during supercooling preservation. Cryobiology 71, 125–129 (2015).
de Vries, R. J. et al. Supercooling extends preservation time of human livers. Nat. Biotechnol. 37, 1131–1136 (2019).
Huang, H., Yarmush, M. L. & Usta, O. B. Long-term deep-supercooling of large-volume water and red cell suspensions via surface sealing with immiscible liquids. Nat. Commun. 9, 3201 (2018).
Cox, S. J., Kathmann, S. M., Slater, B. & Michaelides, A. Molecular simulations of heterogeneous ice nucleation. I. Controlling ice nucleation through surface hydrophilicity. J. Chem. Phys. 142, 184704 (2015).
Shaw, R. A., Durant, A. J. & Mi, Y. Heterogeneous surface crystallization observed in undercooled water. J. Phys. Chem. B 109, 9865–9868 (2005).
Tabazadeh, A., Djikaev, Y. S. & Reiss, H. Surface crystallization of supercooled water in clouds. Proc. Natl Acad. Sci. USA 99, 15873–15878 (2002).
Huang, H., Rey-Bedón, C., Yarmush, M. L. & Usta, O. B. Deep-supercooling for extended preservation of adipose-derived stem cells. Cryobiology 92, 67–75 (2020).
Charlton, S. J. et al. Strong heterogeneity in advances in cryopreservation techniques in the mammalian orders. Zool. Sci. 35, 1–22 (2018).
Hunt, C. J. Technical considerations in the freezing, low-temperature storage and thawing of stem cells for cellular therapies. Transfus. Med. Hemother. 46, 134–150 (2019).
Meyer, H. Women ‘are being given false hope’ over freezing eggs. The Guardian (24 October 2014); https://www.theguardian.com/society/2015/oct/24/women-false-hope-freezing-eggs
Faulkner, K., Bentley, P. & Smyth, S. IVF clinics peddling false hope over egg freezing: doctors caught on camera making wildly optimistic claims about the method’s success. The Daily Mail (2 May 2017); https://www.dailymail.co.uk/news/article-4467352/Desperate-women-duped-freezing-eggs.html
Wang, X. & Riviere, I. Clinical manufacturing of CAR T cells: foundation of a promising therapy. Mol. Ther. Oncolytics 3, 16015 (2016).
Liu, D. & Pan, F. Advances in cryopreservation of organs. J. Huazhong Univ. Sci. Technol. Med. Sci. 36, 153–161 (2016).
Sharpe, M. E., Morton, D. & Rossi, A. Nonclinical safety strategies for stem cell therapies. Toxicol. Appl. Pharmacol. 262, 223–231 (2012).
Bissoyi, A., Nayak, B., Pramanik, K. & Sarangi, S. K. Targeting cryopreservation-induced cell death: a review. Biopreserv. Biobank. 12, 23–34 (2014).
Yagi, T. et al. Caspase inhibition reduces apoptotic death of cryopreserved porcine hepatocytes. Hepatology 33, 1432–1440 (2001).
Laurent, L. C. et al. Dynamic changes in the copy number of pluripotency and cell proliferation genes in human ESCs and IPSCs during reprogramming and time in culture. Cell Stem Cell 8, 106–118 (2011).
Dittmar, K. E. et al. Quality of cell products: authenticity, identity, genomic stability and status of differentiation. Transfus. Med. Hemother. 37, 57–64 (2010).
Iwatani, M. et al. Dimethyl sulfoxide has an impact on epigenetic profile in mouse embryoid body. Stem Cells 24, 2549–2556 (2006).
Chatterjee, A. et al. Effects of cryopreservation on the epigenetic profile of cells. Cryobiology 74, 1–7 (2017).
Browne, J., Tunnacliffe, A. & Burnell, A. Anhydrobiosis—plant desiccation gene found in a nematode. Nature 416, 38–38 (2002).
Yang, J. et al. Exploring the potential of biocompatible osmoprotectants as highly efficient cryoprotectants. ACS Appl. Mater. Interfaces 9, 42516–42524 (2017).
Stewart, S. & He, X. M. Intracellular delivery of trehalose for cell banking. Langmuir 35, 7414–7422 (2019).
Zhang, Y. T. et al. Cold-responsive nanoparticle enables intracellular delivery and rapid release of trehalose for organic-solvent-free cryopreservation. Nano Lett. 19, 9051–9061 (2019).
Parmegiani, L., Cognigni, G. E. & Filicori, M. Ultra-violet sterilization of liquid nitrogen prior to vitrification. Hum. Reprod. 24, 2969 (2009).
Eren, E. A. et al. Donations after circulatory death in liver transplant. Exp. Clin. Transpl. 14, 463–470 (2016).
Zhang, Z. B., Gao, W., Liu, L., Shi, Y. & Shen, Z. Y. Development and assessment of normothermic machine perfusion preservation for extracorporeal splitting of pig liver. Ann. Transpl. 22, 507–517 (2017).
Ratner, B. D., Hoffman, A. S., Schoen, F. J. & Lemons, J. E. Biomaterials Science: An Introduction to Materials in Medicine (Elsevier, 2004).
Juliano, L., Eastwood, G., Berard, T. & Mathew, A. J. The importance of collection, processing and biopreservation best practices in determining CAR-T starting material quality. Cell Gene Ther. Insights 4, 327–336 (2018).
Hawkins, B. J., Abazari, A. & Mathew, A. J. Biopreservation best practices for regenerative medicine GMP manufacturing & focus on optimized biopreservation media. Cell Gene Ther. Insights 3, 345–358 (2017).
Hong, Y. et al. A survey on the awareness and knowledge about elective oocyte cryopreservation among unmarried women of reproductive age visiting a private fertility center. Obstet. Gynecol. Sci. 62, 438 (2019).
Habka, D., Mann, D., Landes, R. & Soto-Gutierrez, A. Future economics of liver transplantation: a 20-year cost modeling forecast and the prospect of bioengineering autologous liver grafts. PLoS ONE 10, e0131764 (2015).
Household Income in the United States (Statistical Atlas, 2018); https://statisticalatlas.com/United-States/Household-Income
Wang, L., Huang, X. & Liu, X. On the ethical and legal problems of single women’s ‘frozen eggs’. Med. Jurisprud. 7, 33 (2015); https://xueshu.baidu.com/usercenter/paper/show?paperid=c2c90868c2099c115f3cbb4bbfe8b797&site=xueshu_se
Personalized Stem Cells, Inc. announces FDA approval of IND application for treatment of osteoarthritis with stem cells. Personalized Stem Cells, Inc. (22 July 2019); https://personalizedstemcells.com/wp-content/uploads/2019/08/Personalized-Stem-Cells-Inc.-Announces-FDA-Approval-of-IND-Application-for-Treatment-of-Osteoarthritis-with-Stem-Cells-July-22-2019.pdf
Pellegrini, G. et al. Navigating market authorization: the path Holoclar took to become the first stem cell product approved in the European Union. Stem Cells Transl. Med. 7, 146–154 (2018).
Risco, R., Elmoazzen, H., Doughty, M., He, X. & Toner, M. Thermal performance of quartz capillaries for vitrification. Cryobiology 55, 222–229 (2007).
Acknowledgements
The authors acknowledge partial funding for this work from NIH grants P41EB002503 and R01EB023632, NSF grant CBET-1831019 and NSFC grant 52076157 and from Xi’an Jiaotong University (Young Talent Support Program).
Author information
Authors and Affiliations
Contributions
H.H. and M.L.Y. conceived the project. H.H. performed the literature review and wrote the manuscript draft. H.H. and X.H. discussed the content and revised the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information Nature Biomedical Engineering thanks Stefan Schneeberger and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, H., He, X. & Yarmush, M.L. Advanced technologies for the preservation of mammalian biospecimens. Nat Biomed Eng 5, 793–804 (2021). https://doi.org/10.1038/s41551-021-00784-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41551-021-00784-z
This article is cited by
-
Cryopreservation breaks the organ transplant time barrier
Nature Reviews Nephrology (2023)
-
Making fitter cells and tissues
Nature Biomedical Engineering (2022)
-
Impact of Cryopreservation and Freeze-Thawing on Therapeutic Properties of Mesenchymal Stromal/Stem Cells and Other Common Cellular Therapeutics
Current Stem Cell Reports (2022)