Abstract
Aims/hypothesis
This study interrogated mitochondrial respiratory function and content in skeletal muscle biopsies of healthy adults between 30 and 72 years old with and without uncomplicated type 1 diabetes.
Methods
Participants (12 women/nine men) with type 1 diabetes (48 ± 11 years of age), without overt complications, were matched for age, sex, BMI and level of physical activity to participants without diabetes (control participants) (49 ± 12 years of age). Participants underwent a Bergström biopsy of the vastus lateralis to assess mitochondrial respiratory function using high-resolution respirometry and citrate synthase activity. Electron microscopy was used to quantify mitochondrial content and cristae (pixel) density.
Results
Mean mitochondrial area density was 27% lower (p = 0.006) in participants with type 1 diabetes compared with control participants. This was largely due to smaller mitochondrial fragments in women with type 1 diabetes (−18%, p = 0.057), as opposed to a decrease in the total number of mitochondrial fragments in men with diabetes (−28%, p = 0.130). Mitochondrial respiratory measures, whether estimated per milligram of tissue (i.e. mass-specific) or normalised to area density (i.e. intrinsic mitochondrial function), differed between cohorts, and demonstrated sexual dimorphism. Mass-specific mitochondrial oxidative phosphorylation (OXPHOS) capacity with the substrates for complex I and complex II (CI + II) was significantly lower (−24%, p = 0.033) in women with type 1 diabetes compared with control participants, whereas mass-specific OXPHOS capacities with substrates for complex I only (pyruvate [CI pyr] or glutamate [CI glu]) or complex II only (succinate [CII succ]) were not different (p > 0.404). No statistical differences (p > 0.397) were found in mass-specific OXPHOS capacity in men with type 1 diabetes compared with control participants despite a 42% non-significant increase in CI glu OXPHOS capacity (p = 0.218). In contrast, intrinsic CI + II OXPHOS capacity was not different in women with type 1 diabetes (+5%, p = 0.378), whereas in men with type 1 diabetes it was 25% higher (p = 0.163) compared with control participants. Men with type 1 diabetes also demonstrated higher intrinsic OXPHOS capacity for CI pyr (+50%, p = 0.159), CI glu (+88%, p = 0.033) and CII succ (+28%, p = 0.123), as well as higher intrinsic respiratory rates with low (more physiological) concentrations of either ADP, pyruvate, glutamate or succinate (p < 0.012). Women with type 1 diabetes had higher (p < 0.003) intrinsic respiratory rates with low concentrations of succinate only. Calculated aerobic fitness (Physical Working Capacity Test [PWC130]) showed a strong relationship with mitochondrial respiratory function and content in the type 1 diabetes cohort.
Conclusions/interpretation
In middle- to older-aged adults with uncomplicated type 1 diabetes, we conclude that skeletal muscle mitochondria differentially adapt to type 1 diabetes and demonstrate sexual dimorphism. Importantly, these cellular alterations were significantly associated with our metric of aerobic fitness (PWC130) and preceded notable impairments in skeletal mass and strength.
Graphical abstract

Similar content being viewed by others

Introduction
For the first time in history, people with type 1 diabetes on intensive insulin therapy are living into the later decades of life [1, 2]. However, ageing adults with diabetes are at higher risk for the occurrence of geriatric syndromes, particularly those associated with deteriorations in skeletal muscle, including frailty [3], falls/fractures [4, 5] and functional disability [6, 7]. These occurrences lead to decreased independence/quality of life [8], higher rates of institutionalisation [9], additional comorbidities [8] and, consequently, premature mortality [9]. The cellular mechanisms underlying deficits to skeletal muscle in type 1 diabetes, particularly in older age, remain largely unknown.
Mitochondrial dysfunction has long been considered to be a primary mediator of age-related muscle decline [10]. In older people without diabetes, declines in in vivo mitochondrial oxidative capacity are associated with reduced gait speed [11], muscle strength and quality [12], resting metabolic rate [13] and insulin sensitivity [14]. Though considerable variability in mitochondrial (dys)function exists amongst adults of the same age (predominantly due to variability in aerobic fitness), the literature generally supports an age-dependent downward trend in skeletal muscle mitochondrial function and content [15, 16].
Evidence exists that mitochondrial dysfunction occurs early in type 1 diabetes, and, hence, at a considerably earlier age in life than in those without type 1 diabetes (reviewed in [17, 18]). We recently reported a decrease in skeletal muscle mitochondrial respiratory function in physically active young adults with type 1 diabetes, despite no change in mitochondrial content [19], suggesting intrinsic mitochondrial deficiencies. However, the deficits in mitochondrial oxidative capacity may not be a universal phenomenon in those with type 1 diabetes as some have reported no differences between control groups and young adults with type 1 diabetes [20,21,22].
With an ageing population of adults with type 1 diabetes on the horizon, understanding whether deficits in muscle mitochondria exist, persist or worsen beyond young adulthood is imperative. Therefore, we employed a cross-sectional study interrogating mitochondrial respiratory function and ultrastructure in skeletal muscle biopsies of adults between 30 and 72 years of age with uncomplicated type 1 diabetes. We hypothesised that women and men with uncomplicated type 1 diabetes have reduced muscle mitochondrial respiratory function and content compared with matched control groups.
Methods
Recruitment and participant characteristics
Female and male participants (hereafter referred to as women and men) with uncomplicated type 1 diabetes between 30 and 72 years old were recruited from the McMaster University campus area and surrounding cities in Southwestern Ontario, Canada. Type 1 diabetes participants were closely matched with participants without diabetes (control group) for age (± 4 years), sex (self-identified male or female), BMI (± 4 kg/m2) and physical activity levels. The latter was assessed by participants’ self-reported leisure physical activity type and time. We excluded people diagnosed with type 2 diabetes, statin-induced myopathy or myalgia, heart disease, severe hypertension, stage 3 neuropathy or severe retinopathy; who used assistive walking devices; who used corticosteroids and NSAIDs (non-steroidal anti-inflammatory drugs); and who smoked or used tobacco products. The study was reviewed and approved by the Hamilton Integrated Research Ethics Board (HiREB #5344), in accordance with the Declaration of Helsinki. All participants (n = 42) gave verbal and written informed consent.
Participant characteristics are presented in Table 1, including the Physical Working Capacity Test at a heart rate (HR) of 130 beats/min (PWC130) and maximal voluntary contraction (MVC). There were no significant differences in any characteristics except for HbA1c, which was significantly higher in individuals with type 1 diabetes compared with control participants. A neurological examination of the peripheral nervous system by a neuromuscular clinician revealed similar scores between groups, except for ~20% of participants with type 1 diabetes, who had evidence of a mild sensory neuropathy (decreased vibration more than mild and/or absent ankle reflexes). No study participants demonstrated severe or even moderate peripheral neuropathy by examination, nor was there any evidence of proximal limb motor deficit.
In both the control and type 1 diabetes groups, ~63% of women were premenopausal (n = 7/8 for control/type 1 diabetes), and ~ 37% of women were postmenopausal (n = 4 each group). In the control group, 43% reported using hormonal contraceptives (birth control or intrauterine device) compared with 50% in the type 1 diabetes group (n = 3 and 4, respectively). Postmenopausal women (n = 5/4 for control/type 1 diabetes) did not declare use of hormone replacement therapy except for one in the type 1 diabetes group. Menstrual cycle was not controlled for in this study.
Characteristics specific to the type 1 diabetes cohort are presented in Table 2. On average, diabetes duration was 28 (±13) years and age of diagnosis was 19 (±10) years. Diabetes duration was significantly longer (p = 0.027) in men (36 ± 11 years) than women (23 ± 13 years). Two participants self-reported symptoms of diabetes-related complications (neuropathy [n = 1] and mild retinopathy/neuropathy [n = 1], respectively), though neurological examination by a neuromuscular clinician did not confirm these self-reports, as mentioned earlier.
Study protocol
Participants visited the laboratory twice with 7–9 days between visits. All participants were instructed to consume a standardised meal 1.5–2 h prior to their visits and refrain from caffeine, alcohol and moderate to vigorous exercise for at least 24 h before each visit.
Visit 1
Body height and weight were recorded to calculate BMI while body composition was assessed via dual-energy x-ray absorptiometry (DEXA; GE Healthcare, Toronto, ON, Canada). Muscle strength was assessed by isometric MVC of the right leg (unless otherwise specified) using an isokinetic dynamometer (Biodex System 3; Biodex Medical Systems, Shirley, NY, USA). Participants were instructed to contract their quadriceps isometrically as hard as they could for 5 s and to rest for 30 s. This was repeated three times with the highest recorded value used. Aerobic fitness was assessed by the PWC130 cycling test. Participants were provided with a wrist-based HR watch (Polar M430, Polar, USA) and instructed to cycle at a cadence between 50 and 70 rev min−1 and maintain it for 10 min. Baseline power was set at 25 watts and thereafter adjusted according to the watch HR data. The goal was to carefully adjust workload in order to steadily increase HR to 130 beats/min by 8 min into the cycling test (with cadence being constant). For the remaining 2 min, power was slightly adjusted if HR began to exceed 135 beats/min. Power and HR were recorded every 15 s during the entire fitness test in order to generate a standard curve of power output (x axis) vs HR (y axis). The slope of the standard curve was used to calculate the power output at 130 beats/min and was also normalised to lean body mass (LBM) (Table 1).
Visit 2
A Bergström needle sample of vastus lateralis muscle was obtained under local anaesthetic (2% lidocaine, 0.005 mg/ml adrenaline [epinephrine]) [23]. A portion of the sample muscle (~15–20 mg) was immediately placed in ice-cold BIOPS buffer [19] for subsequent in vitro assessment of mitochondrial respiratory function. Approximately 5 mg of muscle was placed in ice-cold 2% glutaraldehyde (buffered with 0.1 M sodium cacodylate [pH 7.4]) to preserve the muscle ultrastructure for transmission electron microscopy (TEM) analysis. A blood sample was obtained using venepuncture for HbA1c analysis at the McMaster Core Facility laboratory.
Mitochondrial bioenergetics in permeabilised muscle fibres
The freshly obtained muscle sample in ice-cold BIOPS buffer was divided into small muscle bundles (~1.5–5 mg wet weight) for the preparation of permeabilised muscle fibres (PmFBs), as previously described [24]. Following this, the PmFBs were weighed and washed in buffer Z (in mmol/l: 105 K-MES, 30 KCl, 10 KH2PO4, 5 MgCl2·6H2O, 1 EGTA and 5 mg ml-1 BSA [pH 7.1]) until measurements were initiated (<20 min).
Mitochondrial respiratory kinetics were assessed using the Oroboros Oxygraph-2K (Oroboros Instruments, Innsbruck, Austria), similar to our previous study [19]. The chambers were filled with 2 ml of buffer Z supplemented with 20 mmol/l creatine [25] and 5 μmol/l blebbistatin, and experiments were undertaken at 37°C with constant stirring at 750 rev/min and mild hyperoxygenation (250–275 μmol/l O2).
ADP-stimulated respiratory kinetics were determined through ADP (A5258; Sigma-Aldrich, USA) titrations in the presence of 5 mmol/l pyruvate (P2256; Sigma-Aldrich), 2 mmol/l malate (M1000; Sigma-Aldrich) and 10 mmol/l succinate (S2378; Sigma-Aldrich) to recruit both complex I and complex II (CI + II). Standard pyruvate (CI pyr) and glutamate (CI glu) (GLU303; BioShop, Burlington, ON, Canada) titrations, including 2 mmol/l malate and 5 mmol/l ADP, were performed to determine complex I kinetics. Complex II kinetics were determined through standard succinate titrations (CII succ) in the presence of 10 μmol/l rotenone (R8875; Sigma-Aldrich) and 5 mmol/l ADP. Mitochondrial LEAK respiration (state II) was measured in the presence of saturating complex I substrates (5 mmol/l pyruvate and 2 mmol/l malate) and in the absence of adenylates (i.e. ADP). In doing so, any change in respiration is largely considered to be the result of increased/decreased coupling of oxidative phosphorylation (OXPHOS) to ATP synthesis due to proton re-entry into the matrix through either uncoupling mechanisms or H+-dependent transporters that have been altered [26]. In other words, herein, mitochondrial LEAK respiration refers to the in vitro measure of mitochondrial respiration compensating for proton leak across the inner mitochondrial membrane [27]. Integrity of the mitochondria (outer mitochondrial membrane) was verified by the addition of 10 μmol/l cytochrome c (cat no. 192-10; Lee Biosolutions, Maryland Heights, MO, USA). Any experiments that had a > 10% increase in respiration after the addition of cytochrome c were excluded.
All respirometry data were normalised per milligram wet weight (from here on, referred to as mass-specific mitochondrial respiration); however, this does not discern whether the function per mitochondria has changed or whether mitochondrial content per milligram wet weight has changed. Thus, we further normalised each participant’s respiration rates to their own unique mitochondrial content (area density, discussed below). Importantly, since mitochondrial content was determined in a subset of participants (n = 18 and 17 for control and type 1 diabetes, respectively), the intrinsic mitochondrial respiration data do not include all participants in the study, only those we could normalise to (from here on, referred to as intrinsic mitochondrial respiration).
TEM
TEM Facility staff at McMaster University Medical Centre processed the fresh muscle samples fixed in 2% glutaraldehyde, as described previously [28]. Mitochondrial area density, size, number per muscle area and cristae (pixel) density were quantified in a subset of control (n = 18) and type 1 diabetes (n = 17) participants by Nikon Imaging Software (NIS)-Elements AR (v4.6; Melville, NY, USA) using representative micrographs, as previously described in detail [19].
Citrate synthase assay
The maximal activities of citrate synthase (CS) were determined as previously described [29]. In brief, muscle homogenate was added to a cuvette containing 5,5′-dithiobis (2-nitrobenzoic acid) (DTNB) (D1830; Sigma-Aldrich), acetyl-CoA (A2181; Sigma-Aldrich) and Tris-HCl buffer (pH 8.1) and incubated at 37°C. Oxaloacetate (O4126; Sigma-Aldrich) was then added to initiate the reaction. Absorbance was measured continuously at 412 nm for 2 min at 37°C using a ultraviolet-visible (UV-vis) spectrophotometer (Cary Bio-300; Varian, Palo Alto, CA, USA), and the slope between 30 s and 90 s was used for calculations. Enzyme activity was measured in duplicate and CS maximal activity (expressed as nmol min-1 [mg protein]-1) was expressed relative to total protein measured with a bicinchoninic acid (BCA) assay kit (Pierce, Rockford, IL, USA).
Statistics
Statistical analyses were performed using GraphPad Prism (version 8.0) software (San Diego, CA, USA). All data were initially tested for normal distribution (D’Agostino–Pearson omnibus test) and equal group variance (Brown–Forsythe variance test). The specific analyses used are defined in the figure legends. Statistical significance was established at p ≤ 0.05.
Results
At study initiation, a design to interrogate sex differences was not considered. However, recent work demonstrating sexual dimorphism in human skeletal muscle mitochondrial bioenergetics [30,31,32] made it critical to present control vs type 1 diabetes data as follows: combined (all participants irrespective of sex); women (female participants only); and men (male participants only).
Skeletal muscle mitochondrial ultrastructure
Mean mitochondrial area density was significantly lower (p = 0.006) in the type 1 diabetes group (−27%; Fig. 1b) vs control participants. Women with type 1 diabetes demonstrated a ~20% decrease (p = 0.110) in density while men with type 1 diabetes demonstrated a ~35% decrease (p = 0.033) (Fig. 1b). In women, this was largely due to a decrease (p = 0.057) in mitochondrial fragment size (−18%; Fig. 1c) and not mitochondrial fragment number per muscle area (−9%, p = 0.141) (Fig. 1d). In men, lower mitochondrial density was largely due to decreased (p = 0.130) mitochondrial fragment number per muscle area (−28%; Fig. 1d) compared with mitochondrial size (−9%, p = 0.380) (Fig. 1c). Mitochondrial cristae density (measured by pixel density) was not different (p > 0.270) between cohorts irrespective of sex (Fig. 1e).
Quantification of mitochondrial content and characteristics using representative micrographs captured by TEM. Since TEM provides two-dimensional images, mitochondrial content was determined by calculating the percentage mitochondrial area ‘density’ (mean mitochondrial size × number of mitochondrial fragments per tissue area, expressed as % area of muscle [45]) in a subset of participants with type 1 diabetes (n = 16) and without type 1 diabetes (n = 18). Mitochondrial cristae density was also determined by calculating the pixel density of each mitochondrion whereby a lower pixel density is indicative of swollen mitochondria or reduced cristae surface area. (a) Representative micrographs. Scale bar, 1 μm. (b) Mitochondrial density was significantly lower (**p = 0.006) in combined type 1 diabetes vs control participants. Compared with control participants, women with type 1 diabetes had observably lower (p = 0.110) density while men with type 1 diabetes had significantly lower (*p = 0.033) density. (c) Compared with control participants, individual mitochondrion size was observably lower (†p = 0.056) in women but not men with type 1 diabetes. (d) The number of mitochondrial fragments per unit area was significantly lower in combined participants (*p = 0.048) and men (*p = 0.014), but not women (p = 0.549), with type 1 diabetes. (e) Mitochondrial cristae density was not statistically different with type 1 diabetes. The data were analysed using an unpaired Student’s t test (two-tailed). One male participant with type 1 diabetes was a significant outlier using the ROUT test in GraphPad Prism, depicted as a red circle, and was removed from all statistical analyses in this figure. Boxes represent the interquartile range, whiskers show the maximum and minimum, the horizontal solid line indicates the median and the cross indicates the mean. AU, arbitrary units; CON, control; T1D, type 1 diabetes
Skeletal muscle mitochondrial OXPHOS capacity
CS activity
No difference was found in CS activity between cohorts in a subset of participants (n = 14) (combined [−18%, p = 0.265], women [−17%, p = 0.088], men [+14%, p > 0.999]) (Fig. 2a).
Skeletal muscle mitochondrial CS activity and OXPHOS capacity. (a) CS activity was non-significantly lower (‡p = 0.088) only in women with T1D. Respiration assays were performed in PmFBs, supported by saturating complex I (pyruvate + malate) and complex II (succinate) substrates (CI + II OXPHOS capacity), and normalised by initial muscle wet weight (pmol s−1 [mg wet weight]−1) and by mitochondrial area density, i.e. intrinsic mitochondrial respiration. (b) Mass-specific CI + II OXPHOS capacity was significantly lower (*p = 0.042) in women, but not men, with type 1 diabetes compared with control participants. (c) Intrinsic CI + II OXPHOS capacity was not different between cohorts irrespective of sex. A Student’s unpaired t test (one-tailed) was used to analyse the data. One control female participant was not included in the analyses due to methodological issues. Boxes represent the interquartile range, whiskers show the maximum and minimum, the horizontal solid line indicates the median and the cross indicates the mean. CON, control; mito, mitochondrial; T1D, type 1 diabetes; wt, weight
CI + II-supported respiration
Mitochondrial CI + II OXPHOS capacity was comparable between cohorts for both mass-specific (−11%, p = 0.165) and intrinsic (+11%, p = 0.217) respiration (Fig. 2b,c). Separated by sex, mass-specific CI + II OXPHOS capacity was significantly lower in women (−24%, p = 0.033) but not men with type 1 diabetes (+5%, p = 0.397) (Fig. 2b,c). In contrast, intrinsic CI + II OXPHOS capacity was not different in women with type 1 diabetes (+5%, p = 0.378), while in men with type 1 diabetes it was 25% non-significantly higher (p = 0.163) compared with control participants (Fig. 2b,c).
Complex I-supported respiration
To determine whether alterations exist at the level of complex I or upstream dehydrogenases, specifically pyruvate dehydrogenase (PDH) and glutamate dehydrogenase (GDH), CI pyr and CI glu OXPHOS capacity was also measured as both substrates generate NADH that supports complex I activity. No differences were found between groups with mass-specific CI pyr OXPHOS capacity (combined [−8%; p = 0.572], women [−14%; p = 0.404], men [+1%; p = 0.970]) or CI glu OXPHOS capacity (combined [−3%; p = 0.853], women [−12%; p = 0.404]), except in men with type 1 diabetes where a 42% non-significant increase was measured compared with control participants (p = 0.218) (Fig. 3a,c).
Skeletal muscle OXPHOS capacity of complex I supported by pyruvate (CI pyr) or glutamate (CI glu) and complex II supported by succinate (CII succ) in PmFBs. Respiration assays were normalised by the initial muscle wet weight (pmol s−1 [mg wet weight]−1) (a, c, e) or by mitochondrial area density (i.e. intrinsic mitochondrial function) (b, d, f). Neither (a) mass-specific nor (b) intrinsic CI pyr OXPHOS capacity was different between cohorts. One male participant with type 1 diabetes was not included in the analyses due to methodological issues. While (c) mass-specific CI glu OXPHOS capacity was observably higher in men with type 1 diabetes compared with control men (p = 0.220), only (d) intrinsic CI glu OXPHOS capacity was significantly higher in men with T1D (*p = 0.033). As a result of methodological issues, data were not obtained for n = 4 control (one woman, three men) and n = 4 type 1 diabetic (one woman, three men) participants. Only (f) intrinsic CII succ OXPHOS capacity was observably higher (§p = 0.057) in the type 1 diabetes cohort. A Student’s unpaired t test (two-tailed) was used to analyse all the data. Boxes represent the interquartile range, whiskers show the maximum and minimum, the horizontal solid line indicates the median and the cross indicates the mean. CON, control; mito, mitochondrial; T1D, type 1 diabetes; wt, weight
When normalised to mitochondrial content, CI pyr and CI glu OXPHOS capacities were non-significantly higher (both +27%, p > 0.201) in participants with type 1 diabetes (Fig. 3b,d). When separated by sex, we observed a non-significant 50% increase (p = 0.159) in intrinsic CI pyr OXPHOS capacity and a significant 88% increase (p = 0.033) in intrinsic CI glu OXPHOS capacity in men with type 1 diabetes only (Fig. 3b,d).
Complex II-supported respiration
No differences were found in mass-specific CII succ OXPHOS capacity between groups (combined [−6%; p = 0.502], women [−9%; p = 0.475], men [−3%; p = 0.868]) (Fig. 3e). Normalised to mitochondrial content, CII succ OXPHOS capacity was 25% higher in the type 1 diabetes cohort (p = 0.058) (Fig. 3f). However, women and men with type 1 diabetes demonstrated non-significant 23% (p = 0.268) and 28% (p = 0.123) increases, respectively, in intrinsic CII succ OXPHOS capacity (Fig. 3f).
Skeletal muscle mitochondrial respiratory response to low substrate concentrations
ADP
The ability of mitochondria to respond to changing energy demands (i.e. range of subsaturating ADP concentrations) was interrogated. ADP was titrated at increasing physiological concentrations considered to be representative of conditions of sedentary/low physical activity to moderate/high physical activity and beyond. Collectively, mass-specific submaximal ADP-stimulated respiration was similar (p = 0.230) between cohorts (Fig. 4a). When separated by sex, women with type 1 diabetes demonstrated a reduction in ADP-stimulated respiration (main effect p < 0.001), while in men it was non-significantly higher (main effect p = 0.095) (Fig. 4c,e). In contrast, intrinsic submaximal ADP-stimulated respiration was significantly higher (main effect p = 0.002) in individuals with type 1 diabetes (Fig. 4b); however, no statistical difference was found in women (main effect p = 0.474), whereas a significant increase was found in men (main effect p = 0.001) (Fig. 4d,f).
CI + II-supported mitochondrial respiration stimulated by subsaturating ADP concentrations (CI pyr + CII succ mJO2) in PmFBs. Respiration assays were normalised by initial muscle wet weight (pmol s−1 [mg wet weight]−1) (a, c, e) and by mitochondrial area density (i.e. intrinsic mitochondrial function) (b, d, f). Compared with control participants, mass-specific ADP-stimulated respiration showed a main effect for lower rates (***p < 0.001) in type 1 diabetes for women (c) and observably higher rates (¶p = 0.095) in men with type 1 diabetes (e). However, intrinsic ADP-stimulated respiration showed similar rates in type 1 diabetes for women (d) compared with control participants, whereas a main effect for higher respiration rates was found in type 1 diabetes for combined participants (**p = 0.002) and men (**p = 0.001) (b and f, respectively). A two-way ANOVA was performed to determine a main effect of disease state. One control female participant with type 1 diabetes was not included in the analyses due to methodological issues. Boxes represent the interquartile range, whiskers show the maximum and minimum, the horizontal solid line indicates the median and the cross indicates the mean. c, combined; CON, control; m, men; mito, mitochondrial; mJO2, mitochondrial oxygen flux; T1D, type 1 diabetes; w, women; wt, weight
Pyruvate and glutamate
We also interrogated the response of complex I and/or upstream dehydrogenases to low (i.e. subsaturating) concentrations of pyruvate or glutamate. No differences were found between groups for mass-specific submaximal pyruvate-supported respiration (combined [−8%; p = 0.258], women [−12%; p = 0.545], men [−2%; p = 0.894]) (Fig. 5a,c,e) or submaximal glutamate-supported respiration (combined [+9%; p = 0.232], women [−0.7%; p = 0.956], men [+30%; p = 0.197]) (Fig. 6a,c,e). In contrast, intrinsic pyruvate and glutamate submaximal respiration were both significantly increased (main effect p = 0.003 and p = 0.030, respectively) in the type 1 diabetes cohort (Figs 5b, 6b). Only men with type 1 diabetes showed a significant increase in both pyruvate- (main effect p = 0.005) and glutamate-supported (main effect p = 0.012) respiration (Figs 5f, 6f).
Mitochondrial respiration stimulated by subsaturating pyruvate concentrations (CI pyr mJO2) in PmFBs. Respiration assays were normalised by initial muscle wet weight (pmol s−1 [mg wet weight]−1) (a, c, e) and by mitochondrial area density (i.e. intrinsic mitochondrial function) (b, d, f). No statistical differences were found (p > 0.050) in mass-specific mitochondrial respiration between cohorts (a, c and e). Intrinsic pyruvate-stimulated respiration showed a main effect for higher rates in type 1 diabetes for combined participants (**p = 0.003) and men (**p = 0.005) but not women (p = 0.118) (b, f and d, respectively). A two-way ANOVA was performed to determine a main effect of disease state. One control female participant and one male participant with type 1 diabetes were not included in the analyses due to methodological issues. Boxes represent the interquartile range, whiskers show the maximum and minimum, the horizontal solid line indicates the median and the cross indicates the mean. c, combined; CON, control; m, men; mito, mitochondrial; mJO2, mitochondrial oxygen flux; T1D, type 1 diabetes; w, women; wt, weight
Mitochondrial respiration stimulated by subsaturating glutamate concentrations (CI glu mJO2) in PmFBs. Respiration assays were normalised by initial muscle wet weight (pmol s−1 [mg wet weight]−1) (a, c, e) and by mitochondrial area density (i.e. intrinsic mitochondrial function) (b, d, f). No statistical differences (p > 0.050) were found in mass-specific mitochondrial respiration between cohorts (a, c and e). Compared with control participants, intrinsic glutamate-stimulated respiration showed a main effect for higher rates in type 1 diabetes for combined participants (*p = 0.030) and men (*p = 0.012) but not women (p = 0.438) (b, f and d, respectively). A two-way ANOVA was performed to determine a main effect of disease state. As a result of methodological issues, data were not obtained in four control participants (one woman, three men) and four participants with type 1 diabetes (one woman, three men). Boxes represent the interquartile range, whiskers show the maximum and minimum, the horizontal solid line indicates the median and the cross indicates the mean. c, combined; CON, control; m, men; mito, mitochondrial; mJO2, mitochondrial oxygen flux; T1D, type 1 diabetes; w, women; wt, weight
Succinate
The response of complex II to low concentrations of succinate was also interrogated. No significant differences were found in mass-specific submaximal succinate-supported respiration between groups (combined [−6%; p = 0.335], women [−2%; p = 0.813], men [+17%; p = 0.149]) (Fig. 7a,c,e). In contrast, intrinsic submaximal succinate-supported respiration was significantly increased in the type 1 diabetes group (main effect p < 0.001), and this was consistent in both women and men (main effect p = 0.003 and p < 0.001, respectively) (Fig. 7b,d,f).
Mitochondrial respiration stimulated by subsaturating succinate concentrations (CII succ mJO2) in PmFBs. Respiration assays were normalised by initial muscle wet weight (pmol s−1 [mg wet weight]−1) (a, c, e) and by mitochondrial area density (i.e. intrinsic mitochondrial function) (b, d, f). No statistical differences (p > 0.050) were found in mass-specific mitochondrial respiration between cohorts (a, c and e). Compared with control participants, intrinsic succinate-stimulated respiration showed a main effect for higher rates in type 1 diabetes for combined participants (***p < 0.001), women (**p = 0.003) and men (***p < 0.001) (b, d, and f). A two-way ANOVA was performed to determine a main effect of disease state. Boxes represent the interquartile range, whiskers show the maximum and minimum, the horizontal solid line indicates the median and the cross indicates the mean. c, combined; CON, control; m, men; mito, mitochondrial; mJO2, mitochondrial oxygen flux; T1D, type 1 diabetes; w, women; wt, weight
Skeletal muscle mitochondrial coupling
Collectively, mitochondrial LEAK respiration was 40% higher (p = 0.007) in participants with type 1 diabetes compared with control participants (Fig. 8a). When separated by sex, LEAK respiration was not different in women with type 1 diabetes (+8%; p = 0.608), while in men with type 1 diabetes LEAK respiration was 82% greater (p = 0.002) (Fig. 8b,c), compared with control participants.
Intrinsic mitochondrial LEAK (state II) respiration. Mitochondrial respiration was measured in the absence of ADP but presence of saturating complex I substrates (pyruvate + malate) to drive (maximise) proton leak-dependent respiration (i.e. absence of adenylates). Compared with control participants, LEAK respiration (i.e. state II) was significantly higher with type 1 diabetes for combined participants (**p = 0.007) and men (**p = 0.002) but not women (p = 0.408). A Student’s unpaired t test (two-tailed) was used to analyse the data. One control female participant was not included in the analyses due to methodological issues. Boxes represent the interquartile range, whiskers show the maximum and minimum, the horizontal solid line indicates the median and the cross indicates the mean. CON, control; T1D, type 1 diabetes; wt, weight
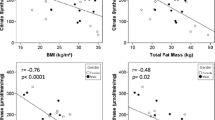
Correlation analyses
Figure 9 contains a customised heat map summarising the correlational analyses performed in the type 1 diabetes cohort, separated into women (Fig. 9a) and men (Fig. 9b), between metrics that we considered clinically relevant and the mitochondrial respiratory measures undertaken.
Heat map of correlations between mitochondrial measures performed and metrics of clinical relevance in women (a) and men (b) with type 1 diabetes. The heat map shows the computed Pearson r correlations using GraphPad Prism. Positive correlations are given in shades of blue/green, and negative correlations in shades of red, with intensity indicating the magnitude of the correlation. *p ≤ 0.050 and ●p ≤ 0.120. Aerobic fitness, muscle mass, muscle strength and fat mass refer to PWC130, % LBM, MVC and % flash monitoring, respectively. Glu, glutamate; mito, mitochondrial; Pyr, pyruvate; Succ, succinate; T1D, type 1 diabetes
Discussion
This is the first study to interrogate mitochondrial respiratory function and content in muscle biopsies of adults with uncomplicated type 1 diabetes with a wide age span (30–72 years old) in comparison with strictly matched control participants (age, sex, BMI and self-reported physical activity levels). The success in our matching strategy was supported by the comparable LBM, muscle strength and calculated aerobic fitness between cohorts. Despite the similarities in these clinically relevant metrics, mitochondrial OXPHOS capacity, mitochondrial respiratory response to low (‘physiological’) substrate concentrations and ultrastructure were altered with type 1 diabetes and demonstrated sexual dimorphism. Specifically, at the whole-muscle level, we found mitochondrial OXPHOS capacity and submaximal ADP respiration were significantly lower in women, but not men, with type 1 diabetes compared with control groups. We also found mitochondrial density to be significantly lower in women and men with type 1 diabetes, with decreased mitochondrial fragment size in women and reduced number of mitochondrial fragments in men being the primary drivers of the decreased density. When respiration rates were normalised to mitochondrial density, the mitochondrial respiratory deficiencies in women with type 1 diabetes disappeared, whereas in men with type 1 diabetes, we found significant increases in mitochondrial OXPHOS capacity and mitochondrial respiratory rates in response to low concentrations of ADP, pyruvate, glutamate or succinate, indicating normal and enhanced intrinsic mitochondrial respiratory function between sexes, respectively. Altogether, these novel findings reveal differential adaptations of muscle mitochondria to type 1 diabetes in middle- to older-aged women and men without overt diabetes complications.
Previous works from our group and others have reported decrements in muscle mitochondrial respiration in young people with type 1 diabetes. These include attenuations in in vivo and in vitro muscle oxidative capacity [19, 30, 33,34,35], decreased submaximal ADP-stimulated respiration [19, 30], decreased complex II submaximal and maximal respiration [19, 30] and decreased complex IV activity [22]. However, these findings are not consistent across all studies, as some groups did not observe differences in mitochondrial OXPHOS capacity [20, 22] and complex II function [22], with only deficiencies in complex IV function reported [22]. These in vitro studies also measured markers of mitochondrial content and reported no differences in mitochondrial area density [19], protein expression of complexes I to V [19, 30] or CS activity [22], indicating intrinsic mitochondrial respiratory deficiencies occur early in the progression of type 1 diabetes in human muscle. While informative, the bulk of studies to date have studied adolescents and young adults, making it unclear if older adults with type 1 diabetes exhibit similar or worsened muscle mitochondria dysfunction. In this study of older adults with type 1 diabetes who are relatively healthy, we found normal CS activity and normal or enhanced intrinsic mitochondrial respiratory function, which was also observably different between sexes. Women with type 1 diabetes had normal intrinsic mitochondrial CI + II OXPHOS capacity, submaximal ADP respiration, and CI pyr and CI glu submaximal respiration, whereas intrinsic CII succ submaximal respiration was significantly higher. In contrast, men with type 1 diabetes had a non-significant increase (p = 0.163) in intrinsic mitochondrial CI + II OXPHOS capacity and significantly greater CI glu OXPHOS capacity, mitochondrial ADP submaximal respiration and CI pyr, CI glu and CII succ submaximal respiration, respectively. While these novel findings contradicted our working hypothesis [17] and the current literature available in young adults with type 1 diabetes, they provide for the first time invaluable insight and evidence that muscle health, as it pertains to mitochondrial function, can generally be preserved in adults with type 1 diabetes with increasing age and disease duration.
Enhanced intrinsic mitochondrial respiratory function has been previously reported in type 2 diabetes muscle in spite of many studies suggesting normal or dysfunctional mitochondria in adults with type 2 diabetes. Specifically, Larsen and colleagues found higher intrinsic mitochondrial substrate sensitivity to glutamate and succinate in biopsies from middle-aged adults with type 2 diabetes compared with age- and BMI-matched control groups [36]. While the mechanisms remain to be fully delineated, some studies suggest this is a compensatory effect and/or adaptation during the progression of diabetes [36, 37]. Interestingly, in the streptozotocin (STZ)-induced type 1 diabetes rodent model, Larsen and colleagues also found intrinsic mitochondrial OXPHOS capacity to be elevated in soleus, and to a varying degree in plantaris, and this occurred in parallel with reduced mitochondrial content [38], similar to our present work. Since insulin resistance is also a feature of type 1 diabetes, the enhanced intrinsic mitochondrial response to physiological substrate concentrations and/or capacity can be a compensatory mechanism for decreased glucose flux into the cell because of insulin resistance. However, this is strictly speculative at this time. We did measure the protein expression of mitochondrial pyruvate carrier 1 and 2 (MPC1, MPC2) in a subset of participants but found no statistical difference between groups (see Electronic supplementary material [ESM] Fig. 1).
Another potential explanation for the sexual dimorphism and altered mitochondrial respiratory function in type 1 diabetes is fibre type differences. While muscle fibre type was not measured, we have preliminary data that (compared with control groups) women with type 1 diabetes display a greater proportion of type IIX and type I fibres, while men exhibit more type IIX and reduced type I fibres. Both men and women with type 1 diabetes have less type IIA fibres. As type II fibres have greater substrate sensitivity than type I fibres, it may be that the differential fibre type expression between men and women with type 1 diabetes explains, in part, the sex differences in mitochondrial respiratory function observed herein.
Interestingly, we did not find significant differences in mitochondrial respiratory function and ultrastructure between pre- and postmenopausal women irrespective of type 1 diabetes (ESM Fig. 2). Altogether, if we compare these study findings with our previous work in younger cohorts with type 1 diabetes [19], we propose that in otherwise healthy women and men with uncomplicated type 1 diabetes entering their fourth decade of life and beyond, intrinsic mitochondrial respiratory function does not worsen, but, rather, differentially adapts to the type 1 diabetes environment to preserve mitochondrial health and, ultimately, muscle metabolic health. Indeed, this a significant stray from our initial hypothesis of accelerated muscle ageing in those with type 1 diabetes [17], but if we consider the complexity and heterogeneity of type 1 diabetes, what remains clear is that there is significant research needed to be done in the area, beginning with larger cohort studies in both sexes.
In the present study, there was the collective ~27% decrease in mitochondrial content (i.e. area density) in the type 1 diabetes cohort. This is in contrast to previous work and is intriguing considering that our participants were strictly matched, had comparable physical activity levels and scored similarly on the aerobic fitness test. Indeed, it is important to recognise that PWC130 is not a direct measure of maximal aerobic capacity (\( \dot{V}{\mathrm{O}}_{2\max } \)), but rather submaximal aerobic capacity. Thus, we cannot negate the possibility that our type 1 diabetes cohort had a lower maximal aerobic capacity compared with matched control participants, and a lower mitochondrial content as a result. On the other hand, a similar aerobic capacity between those with/without type 1 diabetes, as is suggested by our data, would indicate deficits in the mechanisms regulating skeletal muscle adaptations to increased physical activity/exercise in type 1 diabetes (i.e. mitochondrial biogenesis/degradation/quality control). In STZ rodent models, but not type 2 or insulin-resistant models, a decrease in peroxisome-proliferator-activated receptor-γ coactivator-1 alpha (PGC1a) expression, and consequently reduced transcription of mitochondrial genes, has been reported [39]. Insulin deprivation in adults with type 1 diabetes (and thus hyperglycaemia) reduces rates of mitochondrial ATP production and the expression of OXPHOS genes [40]. A recent study in STZ-induced diabetes also found reductions in OXPHOS capacity (but not intrinsic OXPHOS capacity) and reduced protein expression of PGC1a and proteins of the ETC and substrate transport (voltage-dependent anion channel [VDAC], adenine nucleotide translocase [ANT]) with acute insulin deprivation [41]. Interestingly, we did not find differences in adenine nucleotide translocase 1 (ANT1) or adenine nucleotide translocase 2 (ANT2) protein expression between sexes in a subset of participants with type 1 diabetes (ESM Fig. 1). Thus, while speculative, perhaps after more than two decades of exogenous insulin treatment concurrent with muscle insulin resistance, mitochondria undergo numerous adaptations to ensure adequate redox balance and ATP supply, similar to what has been previously suggested in type 2 diabetes [36, 37].
Perspectives and conclusions
Advances for type 1 diabetes care, while not a cure, are allowing those with this chronic disease to live consistently longer than ever before. However, the literature indicates that people with diabetes are more likely to suffer from fatigue, weakness and frailty with increasing age compared with control groups [4, 9]. Given that deficits in muscle mitochondria are well known to trigger catabolic signalling cascades and promote atrophy and loss of muscle strength [42], the present findings provide, for the first time, evidence that alterations to mitochondrial respiratory function and ultrastructure are occurring in middle- to older-aged adults with type 1 diabetes. Our findings also indicate that the mitochondrial changes may be an adaptation/compensation to the pathological consequences of type 1 diabetes (i.e. dysglycaemia and hyper/hypoinsulinaemia) and/or the loss of mitochondrial content. It is important to note that the participants recruited were active (recreationally to very active), mostly resided in a university-dwelling community, had at least a post-secondary education and, if they had type 1 diabetes, were well controlled and knowledgeable on the importance of a healthy lifestyle for managing their disease. Thus, the results of this study should be restricted to these demographics and support the dire need for further research into other demographics with type 1 diabetes, including those who have poor glycaemic management (~83% of youth and ~79% of adults with type 1 diabetes [43]), are sedentary and/or have unhealthy body weight (~60% of adults with type 1 diabetes are overweight/obese [44]).
Taken together, as we continue to uncover how muscle adapts to the type 1 diabetes environment in humans, what remains clear is that women and men are differentially impacted at the cellular level, and future studies must not only consider sex in the treatment and management of type 1 diabetes, but must also consider the importance of regular exercise/physical activity to maintain skeletal muscle metabolic health across the lifespan.
Data availability
All relevant data are included in this article.
Abbreviations
- CI + II :
-
Complex I and complex II
- CI glu :
-
Complex I-supported respiration stimulated by glutamate
- CI pyr :
-
Complex I substrate respiration stimulated by pyruvate
- CII succ :
-
Complex II substrate respiration stimulated by succinate
- CS:
-
Citrate synthase
- HR:
-
Heart rate
- LBM:
-
Lean body mass
- LEAK:
-
State II respiration
- MVC:
-
Maximal voluntary contraction
- OXPHOS:
-
Oxidative phosphorylation
- PGC1a:
-
Peroxisome-proliferator-activated receptor-γ coactivator-1 alpha
- PmFBs:
-
Permeabilised muscle fibres
- PWC130 :
-
Physical Working Capacity Test at HR of 130 beats/min
- STZ:
-
Streptozotocin
- TEM:
-
Transmission electron microscopy
References
Diabetes Control and Complications Trial (DCCT)/Epidemiology of Diabetes Interventions and Complications (EDIC) Study Research Group (2016) Mortality in type 1 diabetes in the DCCT/EDIC versus the general population. Diabetes Care 39(8):1378–1383. https://doi.org/10.2337/dc15-2399
Patterson CC, Dahlquist GG, Gyürüs E, Green A, Soltész G, EURODIAB Study Group (2009) Incidence trends for childhood type 1 diabetes in Europe during 1989-2003 and predicted new cases 2005-20: a multicentre prospective registration study. Lancet 373(9680):2027–2033. https://doi.org/10.1016/S0140-6736(09)60568-7
Aguayo GA, Hulman A, Vaillant MT et al (2019) Prospective association among diabetes diagnosis, HbA1c, glycemia, and frailty trajectories in an elderly population. Diabetes Care 42(10):1903–1911. https://doi.org/10.2337/dc19-0497
Yang Y, Hu X, Zhang Q, Zou R (2016) Diabetes mellitus and risk of falls in older adults: a systematic review and meta-analysis. Age Ageing 45(6):761–767. https://doi.org/10.1093/ageing/afw140
Fan Y, Wei F, Lang Y, Liu Y (2016) Diabetes mellitus and risk of hip fractures: a meta-analysis. Osteoporos Int 27(1):219–228. https://doi.org/10.1007/s00198-015-3279-7
Gregg EW, Beckles GL, Williamson DF et al (2000) Diabetes and physical disability among older U.S. adults. Diabetes Care 23(9):1272–1277. https://doi.org/10.2337/diacare.23.9.1272
Wong E, Backholer K, Gearon E et al (2013) Diabetes and risk of physical disability in adults: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 1(2):106–114. https://doi.org/10.1016/S2213-8587(13)70046-9
Laiteerapong N, Karter AJ, Liu JY et al (2011) Correlates of quality of life in older adults with diabetes: the diabetes & aging study. Diabetes Care 34(8):1749–1753. https://doi.org/10.2337/dc10-2424
Ferri-Guerra J, Aparicio-Ugarriza R, Salguero D et al (2020) The association of frailty with hospitalizations and mortality among community dwelling older adults with diabetes. J Frailty Aging 9(2):94–100. https://doi.org/10.14283/jfa.2019.31
López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G (2013) The hallmarks of aging. Cell 153(6):1194–1217. https://doi.org/10.1016/j.cell.2013.05.039
Choi S, Reiter DA, Shardell M et al (2016) 31P magnetic resonance spectroscopy assessment of muscle bioenergetics as a predictor of gait speed in the Baltimore Longitudinal Study of Aging. J Gerontol A Biol Sci Med Sci 71(12):1638–1645. https://doi.org/10.1093/gerona/glw059
Zane AC, Reiter DA, Shardell M et al (2017) Muscle strength mediates the relationship between mitochondrial energetics and walking performance. Aging Cell 16(3):461–468. https://doi.org/10.1111/acel.12568
Zampino M, Semba RD, Adelnia F et al (2020) Greater skeletal muscle oxidative capacity is associated with higher resting metabolic rate: results from the Baltimore Longitudinal Study of Aging. J Gerontol A Biol Sci Med Sci 75(12):2262–2268. https://doi.org/10.1093/gerona/glaa071
Fabbri E, Chia CW, Spencer RG et al (2017) Insulin resistance is associated with reduced mitochondrial oxidative capacity measured by 31P-magnetic resonance spectroscopy in participants without diabetes from the Baltimore Longitudinal Study of Aging. Diabetes 66(1):170–176. https://doi.org/10.2337/db16-0754
Gonzalez-Freire M, Scalzo P, D’Agostino J et al (2018) Skeletal muscle ex vivo mitochondrial respiration parallels decline in vivo oxidative capacity, cardiorespiratory fitness, and muscle strength: the Baltimore Longitudinal Study of Aging. Aging Cell 17(2):e12725. https://doi.org/10.1111/acel.12725
Porter C, Hurren NM, Cotter MV et al (2015) Mitochondrial respiratory capacity and coupling control decline with age in human skeletal muscle. Am J Physiol Endocrinol Metab 309(3):E224–E232. https://doi.org/10.1152/ajpendo.00125.2015
Monaco CMF, Gingrich MA, Hawke TJ (2019) Considering type 1 diabetes as a form of accelerated muscle aging. Exerc Sport Sci Rev 47(2):98–107. https://doi.org/10.1249/JES.0000000000000184
Monaco CMF, Perry CGR, Hawke TJ (2017) Diabetic myopathy: current molecular understanding of this novel neuromuscular disorder. Curr Opin Neurol 30(5):545–552. https://doi.org/10.1097/WCO.0000000000000479
Monaco CMF, Hughes MC, Ramos SV et al (2018) Altered mitochondrial bioenergetics and ultrastructure in the skeletal muscle of young adults with type 1 diabetes. Diabetologia 61(6):1411–1423. https://doi.org/10.1007/s00125-018-4602-6
Item F, Heinzer-Schweizer S, Wyss M et al (2011) Mitochondrial capacity is affected by glycemic status in young untrained women with type 1 diabetes but is not impaired relative to healthy untrained women. Am J Physiol Regul Integr Comp Physiol 301(1):R60–R66. https://doi.org/10.1152/ajpregu.00747.2010
Sedivy P, Dezortova M, Drobny M, Vlasakova Z, Herynek V, Hajek M (2018) Differences in muscle metabolism in patients with type I diabetes - influence of gender and nephropathy studied by (31)P MR spectroscopy. Physiol Res 67(3):433–441. https://doi.org/10.33549/physiolres.933745
Heyman E, Daussin F, Wieczorek V et al (2019) Muscle oxygen supply and use in type 1 diabetes, from ambient air to the mitochondrial respiratory chain: is there a limiting step? Diabetes Care 43(1):209–218. https://doi.org/10.2337/dc19-1125
Tarnopolsky MA, Pearce E, Smith K, Lach B (2011) Suction-modified Bergström muscle biopsy technique: experience with 13,500 procedures. Muscle Nerve 43(5):717–725. https://doi.org/10.1002/mus.21945
Hughes MC, Ramos SV, Turnbull PC et al (2015) Mitochondrial bioenergetics and fiber type assessments in microbiopsy vs. Bergstrom percutaneous sampling of human skeletal muscle. Front Physiol 6:360. https://doi.org/10.3389/fphys.2015.00360
Aliev M, Guzun R, Karu-Varikmaa M, Kaambre T, Wallimann T, Saks V (2011) Molecular system bioenergics of the heart: experimental studies of metabolic compartmentation and energy fluxes versus computer modeling. Int J Mol Sci 12(12):9296–9331. https://doi.org/10.3390/ijms12129296
Chance B, Williams GR (1955) Respiratory enzymes in oxidative phosphorylation. I. Kinetics of oxygen utilization. J Biol Chem 217(1):383–393. https://doi.org/10.1016/S0021-9258(19)57189-7
Nicholls DG, Budd SL (2000) Mitochondria and neuronal survival. Physiol Rev 80(1):315–360. https://doi.org/10.1152/physrev.2000.80.1.315
Crane JD, Devries MC, Safdar A, Hamadeh MJ, Tarnopolsky MA (2010) The effect of aging on human skeletal muscle mitochondrial and intramyocellular lipid ultrastructure. J Gerontol A Biol Sci Med Sci 65(2):119–128. https://doi.org/10.1093/gerona/glp179
Carter SL, Rennie CD, Hamilton SJ, Tarnopolsky MA (2001) Changes in skeletal muscle in males and females following endurance training. Can J Physiol Pharmacol 79(5):386–392. https://doi.org/10.1139/y01-008
Monaco CMF, Bellissimo CA, Hughes MC et al (2020) Sexual dimorphism in human skeletal muscle mitochondrial bioenergetics in response to type 1 diabetes. Am J Physiol Endocrinol Metab 318(1):E44–E51. https://doi.org/10.1152/ajpendo.00411.2019
Miotto PM, McGlory C, Holloway TM, Phillips SM, Holloway GP (2018) Sex differences in mitochondrial respiratory function in human skeletal muscle. Am J Physiol Regul Integr Comp Physiol 314(6):R909–R915. https://doi.org/10.1152/ajpregu.00025.2018
Skelly LE, Gibala MJ (2019) Skeletal muscle mitochondrial bioenergetics in humans: does sex matter? Exp Physiol 104(4):460–462. https://doi.org/10.1113/EP087447
Cree-Green M, Newcomer BR, Brown MS et al (2015) Delayed skeletal muscle mitochondrial ADP recovery in youth with type 1 diabetes relates to muscle insulin resistance. Diabetes 64(2):383–392. https://doi.org/10.2337/db14-0765
Crowther GJ, Milstein JM, Jubrias SA, Kushmerick MJ, Gronka RK, Conley KE (2003) Altered energetic properties in skeletal muscle of men with well-controlled insulin-dependent (type 1) diabetes. Am J Physiol Endocrinol Metab 284(4):E655–E662. https://doi.org/10.1152/ajpendo.00343.2002
Kacerovsky M, Brehm A, Chmelik M et al (2011) Impaired insulin stimulation of muscular ATP production in patients with type 1 diabetes. J Intern Med 269(2):189–199. https://doi.org/10.1111/j.1365-2796.2010.02298.x
Larsen S, Stride N, Hey-Mogensen M et al (2011) Increased mitochondrial substrate sensitivity in skeletal muscle of patients with type 2 diabetes. Diabetologia 54(6):1427–1436. https://doi.org/10.1007/s00125-011-2098-4
Boushel R, Gnaiger E, Schjerling P, Skovbro M, Kraunsøe R, Dela F (2007) Patients with type 2 diabetes have normal mitochondrial function in skeletal muscle. Diabetologia 50(4):790–796. https://doi.org/10.1007/s00125-007-0594-3
Larsen S, Scheede-Bergdahl C, Whitesell T, Boushel R, Bergdahl A (2015) Increased intrinsic mitochondrial respiratory capacity in skeletal muscle from rats with streptozotocin-induced hyperglycemia. Physiol Rep 3(7):e12467. https://doi.org/10.14814/phy2.12467
Franko A, von Kleist-Retzow JC, Böse M et al (2012) Complete failure of insulin-transmitted signaling, but not obesity-induced insulin resistance, impairs respiratory chain function in muscle. J Mol Med 90(10):1145–1160. https://doi.org/10.1007/s00109-012-0887-y
Karakelides H, Asmann YW, Bigelow ML et al (2007) Effect of insulin deprivation on muscle mitochondrial ATP production and gene transcript levels in type 1 diabetic subjects. Diabetes 56(11):2683–2689. https://doi.org/10.2337/db07-0378
Miotto PM, Petrick HL, Holloway GP (2020) Acute insulin deprivation results in altered mitochondrial substrate sensitivity conducive to greater fatty acid transport. Am J Physiol Endocrinol Metab 319(2):E345–E353. https://doi.org/10.1152/ajpendo.00495.2019
Romanello V, Sandri M (2016) Mitochondrial quality control and muscle mass maintenance. Front Physiol 6:422. https://doi.org/10.3389/fphys.2015.00422
Foster NC, Beck RW, Miller KM et al (2019) State of type 1 diabetes management and outcomes from the T1D exchange in 2016-2018. Diabetes Technol Ther 21(2):66–72. https://doi.org/10.1089/dia.2018.0384
Bohn B, Herbst A, Pfeifer M et al (2015) Impact of physical activity on glycemic control and prevalence of cardiovascular risk factors in adults with type 1 diabetes: a cross-sectional multicenter study of 18,028 patients. Diabetes Care 38(8):1536–1543. https://doi.org/10.2337/dc15-0030
Tarnopolsky MA, Rennie CD, Robertshaw HA, Fedak-Tarnopolsky SN, Devries MC, Hamadeh MJ (2007) Influence of endurance exercise training and sex on intramyocellular lipid and mitochondrial ultrastructure, substrate use, and mitochondrial enzyme activity. Am J Physiol Regul Integr Comp Physiol 292(3):R1271–R1278. https://doi.org/10.1152/ajpregu.00472.2006
Acknowledgements
The authors are extremely thankful to all the participants for their time and effort. The authors would also like to thank L. Brandt, E. Hatcher, K. Barnard and B. Hettinga for graciously helping and assisting with equipment set up for clinical measurements and/or collection of muscle samples. The authors express their appreciation to J. Voth for statistical assistance and G. Grafham and S. Ng for laboratory assistance. The graphical abstract was created using a full subscription with BioRender (www.biorender.com, accessed 17/05/2021).
Authors’ relationships and activities
The authors declare that there are no relationships or activities that might bias, or be perceived to bias, their work.
Funding
This study was funded by the Natural Sciences and Engineering Research Council of Canada (NSERC grants 2018-06324 and 2018-522456 to TJH). CMFM and AGD were recipients of NSERC graduate scholarships, the DeGroote Doctoral Scholarship of Excellence and the Department Graduate Student Research Excellence Award. JPN was supported by a CIHR postdoctoral fellowship.
Author information
Authors and Affiliations
Contributions
CMFM, AGD and TJH conceived and designed the experiments. CGRP, VL and MAT contributed to the conception of experiments. CMFM wrote the manuscript. CMFM performed all experiments with assistance from IAR and JPN. CMFM, AGD, MN, IAR, JPN and LVT analysed data. CMFM, CGRP and TJH interpreted data. MAT performed muscle biopsies and venous blood draw. CMFM, AGD and LVT assisted with muscle and blood sample collection and processing. All authors edited the manuscript and provided final approval of the version to be published. TJH is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of data and the accuracy of the data analysis.
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM
(PDF 296 kb)
Rights and permissions
About this article
Cite this article
Monaco, C.M.F., Tarnopolsky, M.A., Dial, A.G. et al. Normal to enhanced intrinsic mitochondrial respiration in skeletal muscle of middle- to older-aged women and men with uncomplicated type 1 diabetes. Diabetologia 64, 2517–2533 (2021). https://doi.org/10.1007/s00125-021-05540-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-021-05540-1