Abstract
External beam radiotherapy is an effective curative treatment option for localized prostate cancer, the most common cancer in men worldwide. However, conventionally fractionated courses of curative external beam radiotherapy are usually 8–9 weeks long, resulting in a substantial burden to patients and the health-care system. This problem is exacerbated in low-income and middle-income countries where health-care resources might be scarce and patient funds limited. Trials have shown a clinical equipoise between hypofractionated schedules of radiotherapy and conventionally fractionated treatments, with the advantage of drastically shortening treatment durations with the use of hypofractionation. The hypofractionated schedules are supported by modern consensus guidelines for implementation in clinical practice. Furthermore, several economic evaluations have shown improved cost effectiveness of hypofractionated therapy compared with conventional schedules. However, these techniques demand complex infrastructure and advanced personnel training. Thus, a number of practical considerations must be borne in mind when implementing hypofractionation in low-income and middle-income countries, but the potential gain in the treatment of this patient population is substantial.
Key points
-
The global burden of prostate cancer is increasing and prostate cancer is becoming a major source of health-care burden in low-income and middle-income countries (LMICs).
-
Radiotherapy is an essential treatment modality in the management of prostate cancer. However, radiotherapy resources are lacking in LMICs, resulting in excess morbidity and mortality.
-
Hypofractionated radiotherapy schedules offer an opportunity to maintain excellent treatment outcomes while shortening curative radiotherapy courses. This approach expands the treatment capacity and could improve crucial access in communities with limited radiotherapy resources.
-
Initial investments are required for technological upgrades, such as intensity-modulated radiotherapy and image-guided radiotherapy, as well as in specialized training in order to optimally provide hypofractionated treatment. Discussion amongst government agencies and device manufacturers is essential to lower these costs.
-
Personnel training and access to external consultation are critical resources for developing radiotherapy centres. Information and communication technologies enable remote guidance between developing and developed radiotherapy centres.
-
In the long term, hypofractionation programmes result in long-term cost savings and simultaneously expand patient access to a curative modality in the management of prostate cancer.
Similar content being viewed by others
Introduction
Cancer incidence continues to increase and malignancy now represents the second most common cause of death and disability-adjusted life years worldwide after cardiovascular disease1. Prostate carcinoma is the third most prevalent type of cancer worldwide, with over 1,400,000 cases in 2020 and is the most common cancer in men; ~375,000 deaths from prostate were expected in the same year worldwide2. Prostate cancer incidence is rising owing to increased prostate-specific antigen (PSA) screening, longer life expectancy and growing awareness in men’s health. Although the incidence of prostate cancer remains highest in developed countries, the mortality rate is disproportionately higher in low-income and middle-income countries (LMICs). A 2016 analysis of global prostate cancer burden reported age-standardized incidence rates of 68 cases and 14.5 cases per 100,000 in developed and developing countries, respectively, and the respective mortality rates were 10 (15%) and 6.6 (46%) per 100,000 (ref.3).
Only a minority (~5%) of patients present with metastatic disease at the time of diagnosis4. Most patients have localized disease that is amenable to curative-intent treatment, with various management alternatives available, including surgery, external beam radiotherapy (EBRT) and brachytherapy. Radiation treatment and surgery have been shown to have equivalent long-term oncological outcomes, with differences only in the rates and types of associated adverse effects5. An analysis of patient-reported outcomes from the PROTECT trial (NCT02044172) — the largest and most influential randomized evidence comparing patients with localized prostate cancer to active surveillance, EBRT and radical prostatectomy — revealed higher rates of sexual dysfunction and urinary incontinence in patients who underwent prostatectomy, whereas EBRT was associated with a higher risk of gastrointestinal (GI) toxicity6. Notably, although the trial outcomes showed equivalence in oncological end points, the majority of patients were low risk, with >75% of patients having Gleason 6 disease and 90% having a PSA levels of <10 ng/ml (ref.7).
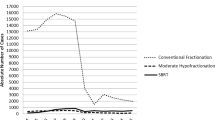
Traditionally, curative-intent EBRT has been delivered using conventional fractionation schedules, treating patients with 1.8–2.0 Gy per day. Initial studies have established that total doses of radiotherapy of 76–78 Gy, compared with lower doses of 68–70 Gy, improve disease control rates by approximately 10–15% at 5 years8,9,10. However, such treatment, albeit effective, entails a treatment course that spans over 7–8 weeks’ duration. The time and financial costs to both the patient and the treatment centre can be substantial. In limited-resource settings, alternative treatment options are necessary and hypofractionation presents that opportunity.
Over the past three decades, technological advancements in radiotherapy planning and delivery have enabled increased precision and accuracy for the treatment of prostate cancer with the advent of intensity-modulated radiotherapy (IMRT) and image-guided radiotherapy (IGRT) technologies11. The former enables fine dose shaping of the target while sparing nearby organs, whereas the latter ensures accuracy in patient setup for each radiation fraction. As such, several phase III randomized trials have investigated and established the clinical efficacy of hypofractionated radiotherapy schedules12,13,14,15,16,17,18,19,20. Hypofractionated radiotherapy schedules provide a larger dose per fraction than the conventional schedules that deliver 1.8–2 Gy. In addition to shortened treatment durations, hypofractionation could present an additional biological benefit in that prostate cancers are thought to have a higher intrinsic sensitivity to larger fraction sizes owing to a posited lower alpha/beta ratio21.
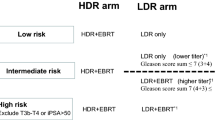
The American Society for Radiation Oncology (ASTRO), American Society of Clinical Oncology (ASCO) and American Urological Association (AUA) recognize that moderate hypofractionation is a compelling option in men with prostate cancer across all risk groups receiving EBRT to the prostate alone as endorsed in their 2018 joint guideline22. In moderate hypofractionation, the per fraction dose ranges between 2.4 and 3.4 Gy; the most commonly used regimen is 60 Gy in 20 fractions over 4 weeks. The joint guideline also makes a conditional recommendation for the use of ultra-hypofractionation in low-risk and intermediate-risk prostate cancer. The guideline defines ultra-hypofractionation as EBRT with a per fraction dose of ≥5 Gy. Usual regimens include 36.5 Gy in 5 fractions, 42.7 Gy in 7 fractions or 35 Gy in 5 fractions22. Furthermore, with the use of IMRT technology, ultra-hypofractionated radiotherapy can be delivered with increased precision and a sharp dose fall-off to surrounding normal tissues in a technique referred to as stereotactic body radiotherapy (SBRT).
This Review will acknowledge and contextualize the advantages that these shorter treatment courses could have for health-care systems, patients and caregivers, particularly in LMICs. We describe the evidence supporting the use of these treatment schemes, their technological requisites and the economic impacts of hypofractionation as they pertain to developing nations.
Framing the issue: global necessity and disparities
Radiotherapy is extensively used in the management of prostate cancer23. The optimal radiotherapy utilization rate in patients with prostate cancer — that is, the ideal number of patients who should receive it within the clinical context — has been estimated at ~60%24,25. This value is corroborated by the use of population-based data to verify estimates of need models in which 61% of prostate cancer patients were estimated to require radiation within 5 years of diagnosis26.
Despite the importance of radiotherapy in cancer treatment, radiotherapy centres are in short supply worldwide and >90% of patients in LMICs do not have access to this treatment modality27. A 2013 report by the International Atomic Energy Agency reported that only 23 of 52 African countries have access to EBRT28. A subsequent 2020 study of 84 LMICs using GLOBOCAN data revealed that only 4 (5%) had the requisite number of radiotherapy units and that almost 40% did not have any facilities present at all. The study projected that these figures will continue to worsen and constitutes a “silent crisis”29. In addition to these data demonstrating the paucity of radiotherapy availability in LMICs, a 2014 report by the Global Task Force on Cancer Care and Control highlighted that between one-third and half of global cancer deaths are avoidable and that 80% of these are in LMICs, where access to radiotherapy is one of the largest gaps in cancer care30.
In Brazil, an upper-middle-income country, close to 110,000 patients (about 20% of cancer diagnoses) requiring radiotherapy were estimated to miss out on receiving this treatment. As a result, >5,000 deaths were attributable to the lack of adequate treatment for the five most common cancers, namely prostate, breast, colorectal, lung and cervical cancers31. Part of the issue is antiquated technology; a 2019 Brazilian federal census showed that 34% of the radiotherapy machines in Brazil were obsolete, with this proportion projected to grow to 51% in 2022 if replacements are not acquired32.
Even in high-income countries disparities exist in access to radiotherapy. A study from Sweden, a high-income country, found that patients with a low income and who were unmarried had a higher likelihood of not receiving standard-of-care radiotherapy management for their cancer33. Often, the reason for this discrepancy is geographical, with patients living in rural areas being disproportionately affected34. The use of shorter treatment courses with hypofractionation can mitigate this latter issue by reducing travel expenses and increasing patient convenience35,36.
Thus, radiotherapy access is a global concern. However, the effects of this lack of access are most pronounced in the developing world, where the greatest disparity exists. The 2015 report by the Lancet Oncology Commission called for an action plan that aimed to increase radiotherapy treatment capacity by 25% in 2025 compared with capacity in 2015 (ref.37). Progress on these goals involving capacity-building in radiotherapy access is being actively investigated by the senior author of this Review and is pending publication. Hypofractionation offers the opportunity to increase treatment capacity for a single radiotherapy machine by simply reducing the number of treatment sessions required per patient, thereby expanding machine capacity for a disease that is becoming more and more common as the developing world advances.
Clinical evidence
A number of clinical trials have evaluated the benefits and outcomes associated with moderate and ultra-hypofractionation in men with prostate cancer as well as the role of concurrent androgen deprivation therapy (ADT).
Evidence supporting moderate hypofractionation
The joint guideline recognizes that moderate hypofractionation should be offered to men with low-risk, intermediate-risk and high-risk prostate cancer; common fractionation schedules typically administer 60–72 Gy over 4–6 weeks12,13,14,16,17,18,38. The bulk of current evidence supports equivalent results with the use of 60 Gy in 20 fractions over 4 weeks to the prostate with or without the inclusion of seminal vesicles and omission of pelvic lymph nodes compared with conventional fractionation22. This schedule was evaluated across patients with predominantly low-risk and intermediate-risk disease in two phase III trials in the presence or absence of ADT16,18.
Seven prospective randomized control trials (RCTs), including close to 6,500 patients in total, have been performed from 2013 to 2019, and demonstrate that moderate hypofractionation renders comparable disease control rates to conventional fractionated regimens12,13,14,16,17,18,38. The largest of these include the CHHiP and PROFIT trials16,18. The former trial enrolled 3,200 patients of all risk groups, although >70% of patients fell into the intermediate risk category. Patients were randomized to one of three arms: the conventional arm of 74 Gy in 34 fractions or one of two hypofractionation arms, of either 60 Gy in 20 fractions or 57 Gy in 19 fractions. After a median follow-up of approximately 5 years, 60 Gy in 20 fractions were found to be non-inferior to 74 Gy in 34 fractions in terms of clinical or biochemical failure, with 90.6% and 88.3% of patients being failure free in the hypofractionated and conventional arms, respectively (p = 0.0018). Similarly, long-term toxicity did not differ between the arms16. The PROFIT trial enrolled 1,200 patients with intermediate-risk disease and randomized them to conventional 78 Gy in 39 fractions versus hypofractionated 60 Gy in 20 fractions. At 5 years, the biochemical recurrence-free survival (BCFS) was 85% in both arms. Grade 3 or greater late toxicity did not differ significantly between the two arms18. (Table 1).
Overall, the data from these RCTs suggest that the efficacy of moderate hypofractionation is not influenced by patient comorbidity, age, anatomy or urinary function. Late GI and genitourinary (GU) toxic effects are comparable between the two fractionation schemes, although RTOG 0415 and HYPRO did report a higher incidence of late toxicity with hypofractionation14,15. Acute GU toxicity was also similar in both groups; however, moderate hypofractionation might be correlated with a higher risk of acute GI toxicity. In the CHHiP trial, grade 2 or greater acute GI toxicity was observed in 38% of patients who received 60 Gy in 20 fractions compared to 25% of patients in the conventional arm (p <0.0001)16. Similarly, Aluwini et al. observed a grade 2 or greater acute GI toxicity incidence of 42% versus 31.2% in the hypofractionated and conventional arms, respectively (p = 0.0015)39. The increase in toxicity observed in the hypofractionated arms of these studies could be explained in part by the higher biological equivalent dose (BED) used. BED is a function of total dose and is a proportional dose per fraction. It has been proposed that BEDs of >180 Gy are associated with a greater risk of toxicity40. Some patient characteristics (prostate volume, age, and baseline GI and/or GU symptoms) are correlated with an increased risk of toxicity despite conventional or hypofractionation schedules22. Similarly, a Cochrane meta-analysis of 10 RCTs with a total of 8,278 patients showed no difference in overall survival (HR 0.94, 95% CI 0.83–1.07) and equivalent prostate cancer-specific survival (HR 1.00, 95% CI 0.72–1.39) between hypofractionation and conventional fractionation. In this Cochrane review, only acute GI toxicity was found to be higher in moderate hypofractionation compared with conventional schedules (RR 1.45, 95% CI 1.19–1.75)41.
Evidence for ultra-hypofractionation
The 2018 joint guideline presents a conditional recommendation for ultra-hypofractionation as an alternative to conventional EBRT in patients with low-risk and intermediate-risk disease22. When the guideline was released, these recommendations were conditional on new data becoming available from ongoing randomized trials. The National Comprehensive Cancer Network (NCCN) lists SBRT as an appropriate treatment option for patients with localized prostate cancer in all risk groups42. Two key phase III trials, both of which were published after the joint guideline, support ultra-hypofractionation19,20 (Table 1). HYPO-RT-PC randomized 1,200 patients with intermediate-risk and high-risk disease to 78 Gy in 39 fractions versus 42.7 Gy in 7 fractions20. After 5 years, failure-free survival in patients who received SBRT was non-inferior to conventional fractionation, at 85% in both arms (p = 0.99). However, patients in the ultra-hypofractionation arm experienced significantly more grade ≥2 GU and GI toxic effects after radiotherapy up to 3 months post treatment than patients in the conventional therapy arm. However, these differences dissipated with longer follow-up duration, except for GU toxicity alone, which, at 1 year, was significantly higher for ultra-hypofractionation at 6% compared with 2% in the conventional therapy arm (p = 0.004). PACE-B was a non-inferiority trial of 874 patients with low-risk and intermediate-risk prostate cancer who were randomized to 78 Gy in 39 fractions, 62 Gy in 20 fractions or 36.25 Gy in 5 fractions19. No differences were observed in grade 2 or worse acute GI toxicity between the conventional or moderate hypofractionation versus the SBRT arms, with an incidence of 12% and 10%, respectively (p = 0.38). Similarly, grade ≥2 acute GU toxic effects between these same groups was at 27% versus 23% (p = 0.16). Oncological outcomes are still eagerly awaited. The promising early toxicity data from PACE-B compared with HYPO-RT-PC suggest that the lower BED in this trial might be preferable. Additionally, all patients in PACE-B were treated with SBRT rather than non-intensity-modulated techniques, whereas this proportion was only 20% in HYPO-RT-PC.
A key aspect to note in these randomized trials is that the majority of patients enrolled had low-risk or intermediate-risk disease. Only 11% of patients in HYPO-RT-PC (NCT03274687) had high-risk disease as defined by T-stage or Gleason grade, suggesting that extrapolation of ultra-hypofractionation to this patient population should be done with caution20. Furthermore, the majority (95%) of patients in the PACE-B (NCT01584258) trial had prostate volumes of <80 cc (ref.19). A 2015 dosimetric analysis of prostate volumes in prostate cancer patients receiving SBRT reported that patients with a V100 (volume receiving 100% of the prescription dose) of >120 cc had the greatest decline in urinary quality of life (QoL)43. Prostate size was not reported in HYPO-RT-PC and, therefore, this detail could further explain the differences in acute toxicities between the two trials. Nevertheless, the results of these trials support the non-inferiority of disease control of ultra-hypofractionation in comparison to moderate hypofractionation and conventional schedules with similar toxicity profiles19,20.
A 2019 systematic review and meta-analysis assessed >6,000 patients treated with SBRT in 38 prospective trials with a median follow-up period of 39 months44. In this meta-analysis, the majority of patients had intermediate-risk disease (n = 2,901), with 78% of included studies containing some proportion of this patient population. Of the 38 trials in the meta-analysis, 92% included patients with low-risk disease and only 38% included patients with high-risk disease. Using data from 2,343 patients in 14 studies, the meta-analysis calculated the overall 5-year BCFS at 95.3% (95% CI 91.3–97.5; p <0.001); in patients with intermediate-risk disease, the 5-year BCRFS was slightly lower, at 92.1% (95% CI 89.2–94.3), whereas BCRFS was 96.7% (95% CI 95.2–97.8) in patients with low-risk disease. Trials including patients with high-risk prostate cancer rarely described the BCRFS results and, therefore, quantitative synthesis was not performed in this patient subset. The estimated incidences of late grade ≥3 GI and GU events were 1.1% (95% CI 0.6–2.0) and 2.0% (95% CI 1.4–2.8), respectively. QoL outcomes measured using the Expanded Prostate Cancer Index Composite (EPIC-26) questionnaire were reported in 25 studies and 3,293 patients. Both GU and GI EPIC-26 scores returned to pre-radiotherapy baseline 2 years after treatment and remained non-significantly different at 5 years compared with the 2-year scores (p = 0.5 and p = 0.8 for GU and GI, respectively). This meta-analysis provides evidence that SBRT for localized prostate cancer is associated with excellent disease control, minimal toxicity and negligible effects on QoL44. Notably, these data largely pertain to patients with low-risk and intermediate-risk disease and, therefore, cannot routinely be applied to patients with high-risk disease.
Role of ADT in hypofractionation
ADT plays an essential role in the management of high-risk and unfavourable intermediate-risk (UIR) prostate cancers treated with radiotherapy. Several trials have established the benefit of the addition of 18–36 months of ADT in patients with high-risk disease and of 4–6 months of ADT in patients with intermediate-risk disease treated with conventionally fractionated radiotherapy schedules45,46,47,48,49,50,51,52. The AUA/ASTRO/Society of Urologic Oncology (SUO) Guideline on the management of clinically localized prostate cancer recommends the use of concurrent ADT in these risk groups in the setting of definitive radiotherapy53.
However, the benefit of ADT is not as well defined in the setting of hypofractionation given that no comparative, randomized trials have directly evaluated this question. The use of ADT was heterogeneous in the moderate hypofractionation trials discussed in this current Review and ranged from none of the patients in the study to the entire cohort, making the contribution of ADT difficult to determine. Nevertheless, the oncological outcomes between the hypofractionated arms of these trials do not seem to drastically differ12,14,16,17,18,38 (Table 1).
Interestingly, none of the patients in the PACE-B or HYPO-RT-PC ultra-hypofractionation trials received ADT, although PACE-B excluded patients with high-risk disease and only a minority of patients had high-risk disease in HYPO-RT-PC19,20.
Thus, ADT was not strongly indicated for the majority of patients enrolled in these trials.
However, several studies in the past few years have investigated the role of ADT in the setting of ultra-hypofractionation for patients with high-risk and UIR disease. A National Cancer Database (NCDB) analysis compared 558 men who received SBRT with 40,797 men who received moderate hypofractionation or conventionally fractionated radiotherapy for the treatment of high-risk or UIR prostate cancer; all patients received concurrent ADT. The study revealed no difference in survival between the two cohorts at 6 years after treatment54. A prospective phase II trial of 154 men with UIR or high-risk prostate cancer treated with SBRT plus 6 months or 24 months of ADT (for UIR and high-risk disease, respectively) reported a favourable 5-year BCFS of 97% and reasonable rates of late grade ≥2 GI and GU toxicities at 7% and 18%, respectively55. No cases of grade 4+ toxicity were reported, which is consistent with the safety data from another phase I/II prospective study evaluating 35 Gy in 5 fractions with concurrent ADT in patients with high-risk disease56. SHARP, a multicentre, prospective consortium57, reported the outcomes of 344 patients with high-risk prostate cancer treated with SBRT, of whom 72% received concurrent ADT. At 4 years after treatment, BCFS and distant metastasis-free survival were 82% and 89%, respectively, suggesting reasonable oncological control. Furthermore, late grade 3+ toxicities were low, at <3%57. Together, these results support the role of SBRT with the addition of ADT in patients with high-risk disease, although further randomized evaluation is certainly warranted.
Summary of evidence
The NCCN42 and 2018 joint22 guidelines suggest moderate hypofractionated radiotherapy as a standard of care in patients with all risk categories of prostate cancer. These guidelines also recognize that, with appropriate expertise and technology, ultra-hypofractionation is a reasonable option for patients with localized disease in patients with low-risk or intermediate-risk disease22,42. In light of the COVID-19 pandemic, SBRT is being encouraged as the schedule of choice for eligible patients in order to minimize hospital visits and, therefore, infection exposure58.
Given that improvement in overall survival has never been observed with any treatment scheme, whether it be hypofractionation, SBRT or conventional dose escalation, other factors need to be considered when determining the optimal management option for patients. Consequently, patient convenience and cost-effectiveness are of utmost importance when determining the best therapy option for patients with localized disease.
Technical considerations
As radiotherapy precision evolves, so too do the technical requirements to necessitate its delivery. At a minimum, modern prostate radiotherapy involves CT-based simulation to guide subsequent treatment using megavoltage linear accelerators (LINACs). Additional upgrades are necessary for advanced methods such as intensity modulation and image-guided treatment delivery.
Treatment simulation
Standard treatment simulation for patients with prostate cancer who will undergo either moderate hypofractionation or SBRT uses CT in the first instance. CT simulation requires several considerations to ensure simulation quality and reproducibility of treatment set-up, particularly relating to intra-patient variability in rectal and bladder filling and prioritizing dose reduction to these structures as critical organs at risk (OARs). To minimize rectal filling discrepancies, patients are instructed to empty their bowels before simulation, using enemas, suppositories and probiotics, although no single rectal management method has been deemed optimal59.
Both retrospective and prospective series have found significant associations between rectal distension and decreased disease control, although this association can be reduced by daily cone-beam CT (CBCT) imaging60,61. Furthermore, in addition to bowel preparation, patients are commonly asked to empty their bladder and to drink a standardized quantity of fluids before they undergo simulation to maintain consistent pelvic anatomy between treatments and to reduce the amount of bladder and bowel inside the treatment field, decreasing the likelihood and severity of toxic effects. A treatment-planning study investigating the effect of bladder filling on radiation dose showed that the median effective dose received by the bladder differed by 20 Gy between a full and empty bladder scan for a radical prostate plan62.
In centres with the capacity to also perform MRI simulation, data support an overall reduction of contoured prostate volume of approximately 26% when comparing combined CT–MRI co-registered treatment planning for target delineation with CT simulation alone and is possibly associated with reductions in acute GU toxicity63. Evidence also suggests that combined CT–MRI can better delineate and spare dosing to erectile tissue, although whether this dose reduction translates into decreased erectile toxicity has yet to be established64. POTEN-C (NCT03525262) is a phase II RCT currently accruing to evaluate the outcomes of neurovascular bundle sparing in prostate SBRT. The trial is expected to complete accrual in June 2024, with a target of 120 patients randomized 1:1 to neurovascular-sparing and non-sparing arms65.
However, much of the evidence to date for hypofractionation has not relied exclusively on MRI guidance for treatment planning; for example, in HYPO-RT-PC and PACE-B, MR-fusion during the simulation process was highly recommended but not mandated. We would recommend the routine addition of MR-fusion if available for ultra-hypofractionation treatment planning; however, it is not essential if not available given that much of the evidence base was developed without it.
Precise target localization before the delivery of each fraction is critical in SBRT owing to the high radiotherapy doses used. For prostate SBRT, transrectal ultrasonography-guided insertion of fiducial seed markers is often performed before simulation to improve target localization. Typically, patients are simulated 7 days after marker insertion to allow for possible seed migration, although some evidence suggests that, in the absence of oedema, seed positions do not vary substantially between insertion and simulation66,67,68. Fiducial marker implantation facilitates the targeting of radiotherapy and increases the accuracy of CBCT matching by up to 91% in the lateral direction and 64% in both the anterior–posterior and superior–inferior directions, respectively, compared with soft-tissue matching alone69,70. Fiducial markers are typically created from a radio-opaque metal such as gold and 3–4 fiducials are usually inserted inside the prostate at different levels of the gland in non-coplanar positions71. Insertion is performed as a 5–10-minute outpatient procedure under local anaesthesia and is commonly well tolerated. Severe adverse events are uncommon: a small number of patients experience urinary urgency (16%), haematuria (13%) or haematospermia (10%). In rare instances, systemic infection could occur in about 3% of patients72. Although recommended, fiducial placement is not mandatory if daily CBCT is available and implemented73,74.
The use of rectal hydrogel spacers (SPACEOAR) can be considered to decrease rectal dose and potential toxicity in patients receiving SBRT. A dosimetric analysis determined that the addition of rectal spacers resulted in a significant decrease of the volume of rectum receiving 28 Gy or more in patients treated with 35 Gy in 5 fractions as per linear correlation analysis (r = 0.626; p = 0.04)75. Similarly, in a phase I trial of 551 patients treated with SBRT, the use of hydrogel spacers was associated with significantly lower risk of grade 2+ late GI (HR 0.24; p = 0.01) and GU (HR 0.37; p <0.001) toxicities compared with no spacer insertion76. Economic evaluations have suggested long-term cost effectiveness with the use of SPACEOAR, particularly in the setting of SBRT77,78; however, the initial cost of this patented procedure, which is on average US$ 2,500 per patient, as well as the technical expertise required for the injection might prove to be prohibitive in LMICs79. Furthermore, scepticism exists regarding the efficacy of SPACEOAR given that the initial randomized evidence supporting its approval did not meet the primary end point of acute GI toxicity improvement in the initial analysis80,81. Furthermore, neither the PACE-B nor the HYPO-RT-PC phase III trials of prostate ultra-hypofractionation mandated the use of hydrogel spacer injections19,20.
Treatment planning
The adaptation of standardized procedures for OAR and target delineation, such as those recommended by the European Society for Radiotherapy and Oncology guidelines82, is useful for both SBRT and moderate hypofractionation in order to ensure that treatment is in accordance with tried and tested protocols. For instance, the PROFIT (NCT00304759) trial18 and CHHiP (ISRCTN97182923)/RTOG 0415 (NCT00331773) studies14,16 contour the rectum using different methods: rectal wall versus hollow structure, respectively. As such, that clinicians follow radiotherapy planning protocols carefully is critical in order to provide safe and effective treatment for patients. Defining a consistent method for planning and evaluation is paramount for each radiotherapy department as the OAR delineation method of choice must be correlated with its corresponding dose–volume constraints.
The clinical target volume includes the entire prostate and, in patients with intermediate-risk and high-risk disease, also incorporates the proximal seminal vesicles as defined on CT or MRI fusion. A planning target volume (PTV) is created as a 5–10 mm expansion on the clinical target volume for hypofractionation and can be 3–7 mm for SBRT; this margin varies based on institutional type, frequency of IGRT, and bladder and bowel preparation policies83.
The 2018 joint guideline provides recommendations for normal tissue constraints for moderate hypofractionation or SBRT based on several published reference trials12,13,14,16,17,18,22,84,85,86. Moreover, at least two dose constraint points must be applied for bladder and rectum: one close to the midpoint of the total dose and the other close to the total prescription dose22. In 2020, NRG (a non-profit research organization formed by the union of three groups: the National Cancer Trials Network, Radiation Therapy Oncology Group (RTOG), and Gynaecology Oncology Group) released a consensus contouring guideline that also provides dose constraint recommendations for moderate hypofractionation, which are in keeping with the 2018 joint guideline87. These expert-developed resources are invaluable for radiotherapy departments that are beginning to develop their prostate hypofractionation programme and are usually easily accessible even for cancer centres operating within LMICs.
Radiotherapy machines
Either gantry-based LINACs equipped with pre-treatment image guidance capabilities or robotic arm-based devices such as the Cyber-Knife (CK) can be used to deliver moderate hypofractionation or SBRT using megavoltage photons. The CK system offers a greater degree of versatility in beam arrangement as it is not constrained to a single plane of rotation. In addition, CK offers real-time fiducial tracking using kV X-ray fluoroscopy throughout treatment delivery, which can modify the position of the treatment head in accordance with patient motion88. Much of the published literature for SBRT stems from experiences using the CK system89. A pooled analysis of 1,100 patients from a multi-institutional consortium of prospective phase II trials investigating prostate SBRT reported a 95%, 84% and 81% rate of 5-year BCFS for patients with low-risk, intermediate-risk and high-risk disease, respectively90. These oncological outcomes reflect those observed from more protracted treatment courses such as moderate hypofractionation or conventional schedules.
However, CK systems are not as readily available as standard LINAC machines, particularly in LMICs, as their cost can be anywhere within US$ 3–5 million91. Furthermore, the treatment times are substantially longer with CK than with standard LINACs (45 versus 15 minutes, on average)92. Two studies have compared the treatment plans of patients with low-risk prostate cancer treated with LINAC and CK-based SBRT regimens who were treated with 36.25 Gy in 5 fractions. Investigators found no dosimetric advantage between CK and non-CK techniques and, in fact, reported that LINAC techniques were associated with superior rectum and bladder sparing93,94. Similarly, a systematic review concluded that robotic arm-based and gantry-based SBRT were associated with equivalent biochemical failure and toxicity rates92. Importantly, the authors of this study drew attention to the reduced treatment time associated with gantry-based LINACs compared with robotic-arm LINACs, which is a crucial factor to consider in limited-resource settings. Notably, these studies use modern LINACs, in which flattening filter-free technology, which saw widespread adoption by 2010 for stereotactic treatments, enables a reduced treatment time and steeper dose gradient compared with older LINACs. Nevertheless, these data provide strong evidence that SBRT can be safely and effectively performed with the more readily available gantry-based LINAC systems in conjunction with CBCT capacity and that the oncological and toxicity outcomes are not inferior to those observed with CK units.
Finally, evolving evidence suggests that MRI-LINACs can feasibly administer a course of SBRT without fiducial placement95,96,97. These machines, which have become commercially available since 2018, have adaptive day-to-day online imaging capabilities, enabling treatment adaptation in the event of plan deviations98,99. However, like CK systems, these novel machines are expensive, costing CAD$ 8.5–10 million100, and have more limited operational capacity than gantry-based LINACs given their comparatively longer treatment durations (typically ~45 minutes as opposed to typically 20 minutes)101. MR-LINACs are, therefore, not well suited for implementation in the developing world.
Treatment delivery and quality assurance
Intensity modulation has been used in many trials and is becoming more commonly implemented for localized prostate cancer treatment given its superior ability to conform to the target volume and to spare nearby normal tissues (Figs 1,2). Only one prospective study has been designed to compare IMRT and 3D-conformal radiotherapy (3D-CRT)102. In this trial, 215 patients treated with 70 Gy in 25 fractions were randomized to receive treatment with either IMRT or 3D-CRT. After 4.6 years’ median follow-up duration, IMRT was associated with lower toxicity rates than 3D-CRT (RTOG grade ≥2 late GU toxicity 3.7% and 12.3%, respectively (p = 0.02); RTOG grade ≥2 late GI toxicity 6.4% and 21.7%, respectively (p = 0.001); RTOG grade ≥2 early GI toxicity 7% and 24%, respectively (p = 0.001); RTOG grade ≥2 early GU toxicity 9% and 27%, respectively (p = 0.001)). The 5-year rate of BCFS was not different for the IMRT and 3D-CRT groups, at 95.4% and 94.3% (p = 0.678), respectively102. A secondary analysis of the RTOG 0126 trial, which compared IMRT and 3D-CRT in patients with prostate cancer, mirrored these findings, with the IMRT arm experiencing significantly less acute GI and GU toxicity than the 3D-CRT arm (10% and 15%, respectively; p = 0.042) as well as grade ≥2 late GI toxicity (15% and 22%, respectively; p = 0.039). These data suggest that IMRT is superior to 3D-CRT for use in hypofractionated prostate radiotherapy delivery, although 3D-CRT is associated with acceptable toxicity rates and oncological outcomes if IMRT is not available103
A dose colour map of a 3D conformal plan used to treat a prostate target using moderate hypofractionation are depicted in axial (part a) and sagittal planes (part b). For a treatment without the use of margin-reducing techniques like image-guided radiotherapy, a 1 cm planning target volume (PTV) margin is used around the prostate. The use of an intensity-modulated radiotherapy technique, shown in axial (part c) and sagittal (part d) planes, results — for this patient — in a modest reduction on the high-dose region overlapping the bladder and rectum but at the expense of small cold spots within the prostate. For comparative purposes, the white line represents the portion of rectum receiving >85% of the prescribed dose (represented by the dark blue colour on the dose map).
The management of inter-fraction and intra-fraction variation is one of the main technical challenges in treatment delivery. A robust quality assurance programme combined with a suitable target margin according to the image-guidance approach is critical in ensuring the safe and effective delivery of moderate hypofractionated and SBRT for localized prostate cancer treatment. Target localization can vary and can be dependent on rectal and bladder filling, even while the treatment is being delivered104. Thus, confirmation of the anatomy is crucial before the delivery of each fraction to avoid a reduction in treatment efficacy and an increase in toxic effects105. Where IGRT is absent, such as in low-resource settings where LINAC upgrades can be cost prohibitive, a larger margin is required, resulting in much higher doses to nearby structures and organs such as the rectum (Figs 3,4).
A dose colour map for a volumetric modulated arc therapy plan proposed to treat a prostate target using stereotactic body radiotherapy without the use of image-guided radiotherapy (IGRT) (planning target volume (PTV) margin of 1 cm) shown in axial (part a) and sagittal (part b) planes and with the use of IGRT (PTV margin of 0.5 cm) in axial (part c) and sagittal (part d) planes. Despite the use of volumetric modulated arc therapy for delivery, without the use of IGRT, the bladder and rectum doses would be unacceptably high and would result in substantial underdosing of the prostate. For comparative purposes, the white line represents the portion of rectum receiving >85% of the prescribed dose (represented by the dark blue colour on the dose map).
The blue circles represent planning criteria for rectal toxicity. Both plans were produced using volumetric modulated arc therapy. The non-image-guided plan does not meet the rectal criteria despite the use of volumetric modulated arc therapy and results in more substantial underdosing of the target volume.
Several options are available to assess prostate displacement during treatment: cine-MRI, electromagnetic transponders such as Calypso system by Varian106, CBCT, fiducial markers and ultrasonography. Each method has advantages and limitations in terms of cost, precision and treatment time22, but the overall goal with all of these systems is to ascertain the inter-fraction and intra-fraction movement of the prostate to enable the application of smaller PTV margins.
Moderate hypofractionation does not require as stringent image guidance as SBRT given the lower dose per fraction and reduced risk of serious adverse effects if one fraction is sub-optimally targeted. This less-stringent approach is reflected in the PTV margin used (5–10 mm), which is often similar to that of conventionally fractionated plans. As such, alternate image guidance approaches can be considered. The use of CBCT and orthogonal kV–kV with fiducials as image-guidance modalities have been compared in a retrospective study of PTV margin definition. The study showed no difference in the accuracy of target delineation and determined that PTV margins can be kept at 5–8 mm with daily imaging regardless of modality used107. Furthermore, more than half of patients in the seminal CHHiP trial16 were not treated with IGRT techniques yet grade 2+ toxicity was only ~12% in the hypofractionated groups despite the lack of image guidance. These data suggest that moderate hypofractionation can be safely and effectively delivered without strict IGRT requirements, improving access in centres in LMICs in which the costs of IGRT upgrades can be prohibitive. However, daily IGRT should be encouraged for facilities with this capability, even for moderate hypofractionation.
Techniques to limit inter-fraction variation include controlling bladder and bowel filling with the intake of a defined volume of water108, the use of laxatives109, a strict diet throughout the course of treatment110 and immobilization of the prostate using an endorectal balloon111. Hydrogel spacers can improve rectal dose and toxicity112. However, despite all these alternatives, the joint AUA/ASCO/ASTRO guideline recommends that, until data from phase III trials are available, each centre should define its IGRT protocol22.
A number of clinical and technical considerations apply to moderate and ultra-hypofractionated treatments (Table 2). As per the 2018 joint guidelines, ultra-hypofractionation should be restricted to patients with a prostate volume of <100 cc, International Prostate Symptom Score (IPSS) of <20 and non-high-risk disease as the majority of published prospective evidence supports these specifications22. Trials that are currently in progress, such as the RTOG/NRG GU005 (NCT03367702) trial and the HEAT trial (NCT01794403), further restrict the criterion of prostate volume to be <70 cc and <80 cc, respectively113,114. From a technological perspective, most of the available data for ultra-hypofractionation are derived from patients treated with IMRT. This is due, in part, to the temporal association between the adoption of intensity modulation in localized prostate trials and the novelty of ultra-hypofractionation. IGRT was mandated in both randomized trials of ultra-hypofractionation as were smaller PTV expansions in comparison to moderate hypofractionation studies, which did not have these requirements19,20,22.
For centres in LMICs considering the transition to hypofractionation, several key points must be considered. First, the appropriate treatment machine must be acquired and commissioned. Gantry-based LINAC systems, the most readily available and affordable radiotherapy machines, can be effective for both moderate and ultra-hypofractionated therapies. Newer technologies such as CK or MR-LINACs, although tempting due to their novelty, are not the most economical investment for a department owing to their high initial start-up costs as well as longer treatment duration. Secondly, clear patient preparation and simulation protocols can provide cost-effective methods to improve treatment outcomes. Stringent pre-treatment patient protocols to ensure bladder filling and rectal emptying are inexpensive to establish, easy to implement and can drastically improve target localization, reducing treatment margins and decreasing overall toxicity. Next, the choice of image guidance, if any, must be determined. An option in departments with multiple LINACs is to equip one with onboard CBCT capabilities and subsequently distribute patient load so that interval IGRT can be performed for all patients, for example, on a weekly basis. However, centres interested in ultra-hypofractionation must keep in mind that IGRT is mandatory for each fraction. If initial upgrade costs for IGRT capabilities are prohibitive, moderate hypofractionation can still be performed with reasonable outcomes16. Finally, treatment planning protocols, including target volume margins and normal tissue tolerances, must be adapted based on IGRT frequency and quality to ensure efficacy and safety.
Cost and cost-effectiveness
Despite the clinical and logistical advantages of hypofractionation, cost and sustainability remain the driving force behind the clinical implementation of new treatment methodologies. Several financial considerations beyond the initial machine purchase cost must be examined by a radiotherapy department prior to developing a hypofractionation programme, including machine commissioning, maintenance, power, staffing and training expenses. Economic evaluations are helpful in providing guidance and long-term cost comparisons between different radiotherapy techniques and modalities.
Economic evaluation studies
Developments in radiotherapy, from standard 3D-CRT, IMRT and incorporation of IGRT, have increased the associated costs for each treatment course. These costs are largely associated with the increased labour required to plan, check and administer IMRT treatments and, therefore, the cost is variable amongst health-care systems. In general, the cost of a conventional course of 3D-CRT for localized prostate cancer has been estimated to be approximately CAD$ 13,500 for each patient, whereas IMRT costs approximately CAD$ 14,520 for each patient in Canada115,116. In the USA, this cost differential was greater than in Canada, in that 3D-CRT was US$ 13,013 per course, whereas IMRT cost US$ 27,084 (ref.117). A British study reported a cost of £ 4,799.31 and £ 5,920.93 for a conventional course of 3D-CRT and IMRT, respectively118. Although IMRT has a higher nominal cost than 3D-CRT, the incremental cost-effectiveness ratio (ICER) of IMRT was shown to be under the generally accepted range of US$ 50,000/quality-adjusted life years (QALY) in the USA119 and Canada115 owing to the eventual health economic savings of this modality, which are due, in general, to lower rates of toxicity120. Likewise, despite higher initiation costs than conventional radiotherapy and moderate hypofractionation, SBRT shows promise for prostate cancer treatment in terms of both the long-term cost savings associated with this modality and the potential radiobiological benefits for disease control with larger fraction sizes21.
A number of economic evaluations have compared conventional, hypofractionated and ultra-hypofractionated treatment for localized prostate cancer121,122,123,124,125,126 (Table 3). A 2012 study by Hodges et al.125 performed a cost–utility comparison between SBRT and conventional IMRT for a model 70-year-old man with localized prostate cancer. In their model, both modalities resulted in a mean QALY of 7.9 years but SBRT was associated with a higher total cost of US$ 22,152 versus US$ 35,431 for conventional IMRT. Sensitivity analysis showed that up to a 6% decrease in efficacy and 4% decrease in toxicity outcomes for SBRT was allowed to maintain an ICER of approximately US$ 50,000 per QALY, which is a commonly accepted willingness-to-pay threshold. Another 2012 US-based study compared the cost utility of conventional IMRT, SBRT and proton therapy. SBRT was found to be the least costly modality with a lifetime cost of US$ 24,873 versus IMRT (US$ 33,068) and proton therapy (US$ 69,412) and resulted in the most QALYs at 8.11 years versus 8.05 and 8.06 years for the same modalities, respectively126. In 2014, Sher et al.124 compared conventional IMRT versus CK-based SBRT and non-CK-based SBRT using a 65-year-old man with low-risk prostate cancer as a model patient. The authors concluded astounding ICERs of US$ 285,000 per QALY and US$ 591,100 per QALY for IMRT over non-CK-based and CK-based SBRT, respectively, suggesting a considerable cost benefit of SBRT over conventional IMRT.
Moderate hypofractionation and SBRT have also been evaluated. A Canadian cost–utility analysis compared conventional, moderate hypofractionated and SBRT treatment schedules in a model 70-year-old man with low-risk prostate cancer. SBRT was ultimately demonstrated to be the most cost-effective option, with a cost of CAD$ 4,368–6,333 per QALY, compared with CAD$ 4,956–6,462 and CAD$ 5,935–7,992 per QALY for moderate hypofractionated and conventional treatment, respectively123. In a secondary analysis of a randomized trial, Voong et al.122 reported a difference of US$ 7,000 at a median of 6 years with conventional (US$ 30,241) versus hypofractionated IMRT (US$ 22,957), with no threshold reported within the sensitivity analysis wherein conventional treatment would be less costly. Finally, a Hungarian cost–utility analysis comparing 3D-CRT with conventional and moderately hypofractionated IMRT concluded that, compared with conventional 3D-CRT, conventional IMRT and hypofractionated IMRT resulted in ICERs of €1,624 and €5,600 less per QALY, respectively121.
Furthermore, these observations are supported by real world data. A 2019 Surveillance, Epidemiology, and End Results (SEER) database analysis estimated an annual cost saving of US$ 160–360 million with the exclusive use of moderate hypofractionation in the USA compared with conventional fractionation127. In LMICs, these cost savings could translate to more money being available for equipment acquisition and upgrades, personnel training, and an opportunity to expand the treatment capacity of the centre127.
Hardware costs
Image-guidance is necessary to decrease toxicity and improve treatment delivery and, for certain techniques such as SBRT, high-quality image guidance is essential. A 2014 comparison of various image-guided radiotherapy strategies estimated the individual costs of distinct IGRT techniques128. In this analysis, the daily costs for cine-MRI, electromagnetic transponders, CBCT, fiducial and ultrasonography were US$ 3,000–4,000/scan, US$ 64–141/day, US$ 143/day, US$ 87/day and US$ 67/day, respectively, according to the Medicare fee schedule. The cost of a transponder placement was estimated at US$ 1,200/patient and fiducial marker placement cost was estimated at US$ 391/patient.
The additional costs of adjunct technologies for radiotherapy delivery must also be taken into consideration. In 2017, the average price of a LINAC was US$ 1,976,000 and the inclusion of the equipment required for CBCT cost an additional US$ 350,000, representing an increase of ~18% in the cost of the machine129. As a result, some centres, whether in high-income countries or LMICs, can find the initial cost prohibitive beyond funding of the basic LINAC, restricting the use of hypofractionated strategies such as SBRT, which require additional equipment130.
In 2012, in order to address the radiotherapy shortage, the Brazilian government spearheaded a national project to expand LINAC capacity within the country131. The initial goal was to expand 32 existing radiotherapy centres and build 48 new centres with a total goal of adding 80 LINACs nationally; however, 8 years after the initiation of the project, only 38 LINACs have been installed and only 29 are operational. Additionally, the goal is now to expand to 100 LINACs total (adding 20 more LINACs to the initial goal of 80) by November 2021, a goal which has been hampered by the COVID-19 pandemic. In Brazil’s radiotherapy expansion project, the estimated cost to upgrade a multi-leaf collimator (MLC) from 80 to 120 leaves to enable increased precision in dose shaping and to add IMRT licenses is US$ 350,000. The upgrade to CBCT capability would add another US$ 350,000. Acquisition of these upgrades, which are necessary in order to provide SBRT, would result in a total cost that is much higher than a basic LINAC.
Machine upkeep and maintenance costs are additional financial considerations for a radiotherapy programme, which can be particularly burdensome to low-resource centres. A 2021 survey of 28 African countries reported that LINAC downtime in these countries is associated with failures of the vacuum pump, power instability and malfunction of the MLCs132. Recurring costs have been estimated to account for a further 5.5–15% of the initial machine investments133. LINAC maintenance and quality assurance (QA) have been estimated to have a median annual cost of US$ 41,390, with further annual electrical costs of US$ 2,800 for machine operation. The median cost per fraction of radiotherapy has been calculated as US$ 11.02 for LINAC machines, which further illustrates the cost benefits of hypofractionation in minimizing these added costs134.
Personnel and training costs
Finally, the stringent dosimetric constraints, complex planning requirements and treatment monitoring involved in hypofractionation will require advanced training and departmental protocol development that meets internationally accepted standards set by trial protocols and are in line with the International Commission of Radiation Units and Measures (ICRU)135. Radiology departments will be required to fund the additional training required to ensure proper treatment setup and delivery themselves as well as covering the costs of equipment maintenance and QA. Skilled personnel training has been identified as a particular challenge in LMICs, in which human resources are often limited. A 2014 study of radiation therapy infrastructure and human resources in LMICs estimated deficits of 39%, 68% and 67% in radiation oncologists, medical physicists and radiation therapists, respectively; in 2020, they estimated that these same needs would grow to be 103%, 292% and 270%, respectively, of the 2014 capacity29. Often, training must be sought in well-established cancer centres in industrialized countries, which presents further issues. The first of these is the cost of training. The cost of a European-trained team of four radiation oncologists, three medical physicists and seven therapists has been estimated at €1.85–2.516 million, which is prohibitive to most radiation oncology centres in LMICs. Nevertheless, the International Atomic Energy Agency (IAEA) provides grant support for candidates from low-income countries and partial coverage for trainees from middle-income countries to train abroad27. The second issue is of ‘brain drain’, whereby trained professionals opt to emigrate to more industrialized countries after training for better opportunities, resources and QoL. This phenomenon has been identified as a particular issue for medical physicists as they seek support in countries where they are not identified as health professionals, which is commonplace in LMICs136. The brain drain phenomenon has been identified as a major concern in the global oncology community and a call to action has been made for developed countries to help LMIC institutions to retain personnel after training by abolishing policies such as merit-based immigration, which involves setting educational and skill requirements for prospective immigrants137.
Obstacles and opportunities for LMICs
Despite the advantages of hypofractionation, adoption in LMICs remains low compared with high-income countries138. A 2021 international ESTRO survey of over 2,300 radiation oncologists reported that radiation oncologists from LMICs (OR 0.54; p <0.001) and Asia-Pacific regions (OR 0.47; p <0.001) were significantly less likely to use hypofractionation on multivariable analysis than Europeans. In prostate cancer treatment specifically, respondents practicing in the Middle East and Africa reported the lowest rates of hypofractionation utilization (18–30%) despite also being nations in which resource limitations are high. The authors of the study raise concerns that a knowledge gap existed, particularly in Africa, where respondents had the lowest acceptance of hypofractionation but, conversely, the highest support for controversial indications such as elective pelvic irradiation138. Provider education is an important consideration in the implementation and acceptance of a hypofractionation programme and, as such, just as critical to the development of a hypofractionation programme as the technical infrastructure.
Opportunities for improvement
As global access to the internet expands, e-learning approaches provide a promising and robust platform for educational opportunities between developed and developing countries. For example, the Africa Radiation Oncology Network (AFRONET) coordinated by the IAEA, enables radiation oncology trainees from Anglophone African countries to learn from international experts in the field139. Several other professional organizations, including ASTRO and the American Association of Physicists in Medicine (AAPM), have developed online training modules specifically geared towards LMICs in order to extend opportunities for education, cancer care, research and outreach to developing nations140. The radiation oncology community is encouraged to take advantage of information and communication technologies (ICTs) in order to extend opportunities for education, cancer care, research and outreach to developing nations141. In particular, ICT platforms can enable educational sessions and resources to be shared from established oncology centres in developed countries with developing centres in LMICs. In 2019, experts from the UK and Canada, in consultation with the IAEA, led a 4.5-day web-based programme on the target volume delineation in the treatment of prostate cancer. It was attended by 22 participants from 11 African LMICs. Participants were able to participate in 1:1 tutorials to consolidate their learning and, in some cases, produce acceptable target volume and normal tissue contours, with only minor revision required142. Furthermore, in day-to-day operations, cloud-based technology could be used for plan review, whereby experts from established centres can offer aid and opinions on more complex plans remotely141,143.
Several other ICT-powered programmes are currently in existence144. BOTSOGO is a collaborative effort between Harvard Medical School and the oncology community of Botswana, which includes monthly tumour boards as well as guidance on developing a local research infrastructure145. Radiating Hope, a non-profit organization dedicated to updating and providing radiotherapy equipment to developing countries, has developed a remote platform to enable treatment planning QA and technical support144,146. The Quality Assurance Review Centre (QARC) is a US-based programme from the University of Massachusetts Medical School that provides remote radiotherapy plan QA as well as clinical trial support for developing countries144. Global RT is an online forum for the education and discussion of the essential nature of radiotherapy for the global community, which also lists global oncology opportunities for interested volunteers147.
As machine learning (ML) and artificial intelligence technologies evolve, the development of machine-assisted planning also offers an opportunity for LMICs. In 2019, the first patient with localized prostate cancer was treated with IMRT via a machine-generated plan as part of a clinical trial in Canada148. Since then, substantial focus has been directed towards advancing these technologies in the field of radiation oncology. Not only does the use of ML-based planning algorithms expand the capacity for patient treatment but it might also support the training of inexperienced personnel and guide them through the planning process without the need for direct supervision. Furthermore, ML can facilitate plan QA, a process in most centres in which new radiotherapy plans are reviewed by the departmental group for safety and quality. In this way, centres with limited personnel can focus their human resources on reviewing only on the cases with the most complex concerns necessitating group discussion149. A 2020 perspective piece by Australian radiation therapists urged that ML education be incorporated in radiation therapy training programmes as its role in patient care expands and is substantiated150; however, at the time of writing, the field of ML and its application to radiotherapy is still in its infancy. Further refinement of these technologies is required before regular practice implementation can occur in developed countries with sufficient personnel oversight and, subsequently, in LMICs.
Modelling the impact of prostate hypofractionation
The potential for increasing access to radiotherapy by using moderate hypofractionation and/or SBRT in the treatment of localized prostate cancer can be illustrated with a real-life working example. A 2013 analysis of African radiotherapy resources by the IAEA identified Nigeria as needing the most additional machines (138 machines) to adequately service their population28. Thus, the potential benefits of hypofractionation in Nigeria can be used to model the effects of hypofractionation rollout in other LMICs.
Capacity
This model begins with a number of assumptions. According to the IAEA directory of radiotherapy centres, as of 2020, Nigeria has seven linear accelerators to service the entire country151. Each radiotherapy unit is estimated to treat 400–600 patients a year for all indications37,152. Given that a course of conventional radiotherapy for prostate cancer tends be longer than most other radiotherapy treatments153, usually requiring 38–39 daily fractions, the lower end of 400 patients is a reasonable capacity estimate per radiotherapy machine per year. By contrast, moderate hypofractionation will be assumed to be 20 daily fractions and SBRT to be 5 daily fractions as per CHHiP/PROFIT and PACE-B schedules. According to the GLOBOCAN database, a total of 15,306 cases of prostate cancer were reported in Nigeria in 2020 (ref.2), which, when considering previous series reporting that nearly 60% of patients presenting for care in southwestern Nigeria had metastatic stage at presentation154,155, means that 6,122 (40%) patients annually would require radical treatment for localized prostate cancer. For the purposes of this example, we assume that all patients will be eligible for radical radiotherapy and that prostatectomy will not be considered as a competing treatment modality.
Considering all assumptions, a total of 2,800 prostate cancer patients (46% of all incident prostate cancers per year) can be treated annually with conventional treatment using Nigeria’s current machine capacity, before even considering the use of the machine to treat other malignancies that ‘compete’ for radiotherapy resources. The implementation of hypofractionation would translate into a twofold increase in capacity, without any additional investment. SBRT has the most drastic effect, with a treatment course that requires only one-eighth of the fractions needed for a conventional course. The implementation of SBRT would, therefore, mean that nearly all patients would be able to access curative therapy. Thus, the benefit of using hypofractionation to increase the proportion of patients who will be able to receive curative intent radiotherapy is clear.
Cost
According to a 2016 economic analysis that directly compared the costs of a conventional, hypofractionation and ultra-hypofractionated schedule, the total cost of treating all 2,800 patients with arc-based conventional fractionation would be CAD$ 16,618,000 (US$ 12.6 million)123. By contrast, hypofractionation and SBRT with the same arc-based system would cost CAD$ 13,876,800 and CAD$ 12,230,400, respectively, for these same 2,800 patients. This difference amounts to a total cost-saving of almost CAD$ 3 million and CAD$ 4.5 million with hypofractionation and ultra-hypofractionation, respectively, compared with a conventional fractionation schedule. However, the start-up costs associated with machine upgrade and personnel training must also be considered, although personnel training can be covered by the IAEA programme for trainees from LMICs. Assuming that each LINAC requires MLC and CBCT upgrades (which are estimated to cost US$ 700,000 as per the Brazilian report131) to provide optimal hypofractionation treatment, the cost would total US$ 4.9 million (CAD$ 6.25 million). Thus, using moderate hypofractionation the initial capital invested in upgrading these LINACs would break even in a little over 2 years and the costs would be recouped in less than 2 years for SBRT. Notably, although IMRT and CBCT capabilities are ideal for moderate hypofractionation, they are not mandatory and, therefore, represent an area of initial cost-savings that could lead to faster recoupment of overall costs. Thus, by lobbying government agencies for increased funding and device manufacturers to lower acquisition costs for LINACs, the necessary infrastructure can be established in LMICs such as Nigeria, and these countries could expect to offer curative treatment options to more patients with localized prostate cancer in a sustainable manner.
These data are in line with a modelling analysis on the cost savings of switching from conventional to moderate hypofractionation in African countries, which predicted an even greater financial benefit of hypofractionation. This study used an activity-based costing model, which comprehensively accounted for optimal allocation algorithms to treatment machines as well as personnel salaries, consumable resources, and costs of construction and maintenance. Over a span of 5 years (2019–2025), Nigeria would be expected to save US$ 91.2 million in total (about US$ 13 million a year) if considering factors beyond machine and treatment costs such as maintenance and education156.
The population level benefits of hypofractionation can also extend to upper-middle income countries. In 2016, in the Brazilian public health system, 27,757 patients with intermediate-risk and high-risk prostate cancer were in need of definitive treatment with radiotherapy. Nevertheless, only 53.4% of this population are estimated to have received radiotherapy in this system, resulting in a projected death of 562 patients with intermediate-risk prostate cancer and of 298 with high-risk disease in the 10–13 years from diagnosis31. Considering that, in 2016, all patients in the Brazilian public health system were treated using a conventionally fractionated radiotherapy regimen (74 Gy in 37 fractions), almost the entire prostate cancer population (98.8%) requiring radiotherapy in that year could have been treated by the adoption of moderate hypofractionation radiotherapy (60 Gy in 20 fractions).
Conclusions
Evolving evidence supports the efficacy and safety of moderate hypofractionation and ultra-hypofractionation in the management of localized prostate cancer. With resource allocation being a key consideration in LMICs, abbreviating treatment times can alleviate health-care burden and costs to both providers and patients. Hypofractionated regimens can be delivered without substantial added costs to current radiotherapy programmes and, in the long term, have proven more cost-effective. As the world population ages and prostate cancer becomes more prevalent, radiotherapy providers should be encouraged to consider the timely adoption of these treatment schedules.
References
Global Burden of Disease Cancer Collaboration. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2017: a systematic analysis for the global burden of disease study. JAMA Oncol. 5, 1749–1768 (2019).
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249 (2021).
Wong, M. C. S. et al. Global incidence and mortality for prostate cancer: analysis of temporal patterns and trends in 36 Countries. Eur. Urol. 70, 862–874 (2016).
Thompson, S. R. et al. Estimation of the optimal utilisation rates of radical prostatectomy, external beam radiotherapy and brachytherapy in the treatment of prostate cancer by a review of clinical practice guidelines. Radiother. Oncol. 118, 118–121 (2016).
Hamdy, F. C. et al. 10-Year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer. N. Engl. J. Med. 375, 1415–1424 (2016).
Donovan, J. L. et al. Patient-reported outcomes after monitoring, surgery, or radiotherapy for prostate cancer. N. Engl. J. Med. 375, 1425–1437 (2016).
Lane, J. A. et al. Active monitoring, radical prostatectomy, or radiotherapy for localised prostate cancer: study design and diagnostic and baseline results of the ProtecT randomised phase 3 trial. Lancet Oncol. 15, 1109–1118 (2014).
Pasalic, D. et al. Dose escalation for prostate adenocarcinoma: a long-term update on the outcomes of a phase 3, single institution randomized clinical trial. Int. J. Radiat. Oncol. Biol. Phys. 104, 790–797 (2019).
Michalski, J. M. et al. Effect of standard vs dose-escalated radiation therapy for patients with intermediate-risk prostate cancer: the NRG Oncology RTOG 0126 randomized clinical trial. JAMA Oncol. 4, e180039 (2018).
Peeters, S. T. et al. Dose-response in radiotherapy for localized prostate cancer: results of the Dutch multicenter randomized phase III trial comparing 68 Gy of radiotherapy with 78 Gy. J. Clin. Oncol. 24, 1990–1996 (2006).
Wortel, R. C. et al. Late side effects after image guided intensity modulated radiation therapy compared to 3D-conformal radiation therapy for prostate cancer: results from 2 prospective cohorts. Int. J. Radiat. Oncol. Biol. Phys. 95, 680–689 (2016).
Pollack, A. et al. Randomized trial of hypofractionated external-beam radiotherapy for prostate cancer. J. Clin. Oncol. 31, 3860–3868 (2013).
Hoffman, K. E. et al. Risk of late toxicity in men receiving dose-escalated hypofractionated intensity modulated prostate radiation therapy: results from a randomized trial. Int. J. Radiat. Oncol. Biol. Phys. 88, 1074–1084 (2014).
Lee, W. R. et al. Randomized phase III noninferiority study comparing two radiotherapy fractionation schedules in patients with low-risk prostate cancer. J. Clin. Oncol. 34, 2325–2332 (2016).
Aluwini, S. et al. Hypofractionated versus conventionally fractionated radiotherapy for patients with prostate cancer (HYPRO): late toxicity results from a randomised, non-inferiority, phase 3 trial. Lancet Oncol. 17, 464–474 (2016).
Dearnaley, D. et al. Conventional versus hypofractionated high-dose intensity-modulated radiotherapy for prostate cancer: 5-year outcomes of the randomised, non-inferiority, phase 3 CHHiP trial. Lancet Oncol. 17, 1047–1060 (2016).
Arcangeli, G. et al. Moderate hypofractionation in high-risk, organ-confined prostate cancer: final results of a phase III randomized trial. J. Clin. Oncol. 35, 1891–1897 (2017).
Catton, C. N. et al. Randomized trial of a hypofractionated radiation regimen for the treatment of localized prostate cancer. J. Clin. Oncol. 35, 1884–1890 (2017).
Brand, D. H. et al. Intensity-modulated fractionated radiotherapy versus stereotactic body radiotherapy for prostate cancer (PACE-B): acute toxicity findings from an international, randomised, open-label, phase 3, non-inferiority trial. Lancet Oncol. 20, 1531–1543 (2019).
Widmark, A. et al. Ultra-hypofractionated versus conventionally fractionated radiotherapy for prostate cancer: 5-year outcomes of the HYPO-RT-PC randomised, non-inferiority, phase 3 trial. Lancet 394, 385–395 (2019).
Wang, J., Guerrero, M. & Li, X. How low is the alpha/beta ratio for prostate cancer? Int. J. Radiat. Oncol. Biol. Phys. 55, 194–203 (2003).
Morgan, S. C. et al. Hypofractionated radiation therapy for localized prostate cancer: an ASTRO, ASCO, and AUA evidence-based guideline. J. Clin. Oncol. 36, JCO1801097 (2018).
Jaffray, D. A. & Gospodarowicz, M. K. in Disease Control Priorities 3rd edn, Vol 3 (eds Gelband, H. & Jha, P.) Ch.14 (The World Bank, 2015).
Delaney, G., Jacob, S. & Barton, M. Estimating the optimal external-beam radiotherapy utilization rate for genitourinary malignancies. Cancer 103, 462–473 (2005).
Barton, M. B. et al. Estimating the demand for radiotherapy from the evidence: a review of changes from 2003 to 2012. Radiother. Oncol. 112, 140–144 (2014).
Tyldesley, S. et al. Estimating the Need for radiotherapy for patients with prostate, breast, and lung cancers: verification of model estimates of need with radiotherapy utilization data from British Columbia. Int. J. Radiat. Oncol. Biol. Phys. 79, 1507–1515 (2011).
Zubizarreta, E. H., Fidarova, E., Healy, B. & Rosenblatt, E. Need for radiotherapy in low and middle income countries — the silent crisis continues. Clin. Oncol. 27, 107–114 (2015).
Abdel-Wahab, M. et al. Status of radiotherapy resources in Africa: an International Atomic Energy Agency analysis. Lancet Oncol. 14, e168–e175 (2013).
Datta, N. R., Samiei, M. & Bodis, S. Radiation therapy infrastructure and human resources in low- and middle-income countries: present status and projections for 2020. Int. J. Radiat. Oncol. Biol. Phys. 89, 448–457 (2014).
Jaffray, D. A. & Gospodarowicz, M. Bringing global access to radiation therapy: time for a change in approach. Int. J. Radiat. Oncol. Biol. Phys. 89, 446–447 (2014).
Mendez, L. C., Moraes, F. Y., Fernandes, G. D. S. & Weltman, E. Cancer deaths due to lack of universal access to radiotherapy in the Brazilian public health system. Clin. Oncol. 30, e29–e36 (2018).
Ministerio de Saude, Secretaria de Atenção Especializada á Saúde; Departamento de Atenção Especializada e Temática. Censo Radioterapia https://portalarquivos.saude.gov.br/images/pdf/2019/julho/26/paper-radioterapia-ALT3.pdf (2019).
Olsson, L. I., Granstrom, F. & Glimelius, B. Socioeconomic inequalities in the use of radiotherapy for rectal cancer: a nationwide study. Eur. J. Cancer 47, 347–353 (2011).
Aneja, S. et al. Geographic analysis of the radiation oncology workforce. Int. J. Radiat. Oncol. Biol. Phys. 82, 1723–1729 (2012).
Aneja, S., Pratiwadi, R. R. & Yu, J. B. Hypofractionated radiation therapy for prostate cancer: risks and potential benefits in a fiscally conservative health care system. Oncology 26, 512–518 (2012).
Plataniotis, G. A. et al. A short radiotherapy course for locally advanced non-small cell lung cancer (NSCLC): effective palliation and patients’ convenience. Lung Cancer 35, 203–207 (2002).
Atun, R. et al. Expanding global access to radiotherapy. Lancet Oncol. 16, 1153–1186 (2015).
Incrocci, L. et al. Hypofractionated versus conventionally fractionated radiotherapy for patients with localised prostate cancer (HYPRO): final efficacy results from a randomised, multicentre, open-label, phase 3 trial. Lancet Oncol. 17, 1061–1069 (2016).
Aluwini, S. et al. Hypofractionated versus conventionally fractionated radiotherapy for patients with prostate cancer (HYPRO): acute toxicity results from a randomised non-inferiority phase 3 trial. Lancet Oncol. 16, 274–283 (2015).
Brenner, D. J. & Hall, E. J. Are we now able to define guidelines for moderate hypofractionation in prostate cancer radiation therapy? Int. J. Radiat. Oncol. Biol. Phys. 100, 871–873 (2018).
Hickey, B. E., James, M. L., Daly, T., Soh, F. Y. & Jeffery, M. Hypofractionation for clinically localized prostate cancer. Cochrane Database Syst. Rev. 9, CD011462 (2019).
National Comprehensive Cancer Network. Prostate Cancer https://www.nccn.org/professionals/physician_gls/pdf/prostate_blocks.pdf (2020).
Gomez, C. L. et al. Dosimetric parameters predict short-term quality-of-life outcomes for patients receiving stereotactic body radiation therapy for prostate cancer. Pract. Radiat. Oncol. 5, 257–262 (2015).
Jackson, W. C. et al. Stereotactic body radiation therapy for localized prostate cancer: a systematic review and meta-analysis of over 6,000 patients treated on prospective studies. Int. J. Radiat. Oncol. Biol. Phys. 104, 778–789 (2019).
Bolla, M. et al. Duration of androgen suppression in the treatment of prostate cancer. N. Engl. J. Med. 360, 2516–2527 (2009).
Hanks, G. E. et al. Phase III trial of long-term adjuvant androgen deprivation after neoadjuvant hormonal cytoreduction and radiotherapy in locally advanced carcinoma of the prostate: the radiation therapy oncology group protocol 92–02. J. Clin. Oncol. 21, 3972–3978 (2003).
Denham, J. W. et al. Short-term androgen suppression and radiotherapy versus intermediate-term androgen suppression and radiotherapy, with or without zoledronic acid, in men with locally advanced prostate cancer (TROG 03.04 RADAR): 10-year results from a randomised, phase 3, factorial trial. Lancet Oncol. 20, 267–281 (2019).
Nabid, A. et al. Duration of androgen deprivation therapy in high-risk prostate cancer: a randomized phase III trial. Eur. Urol. 74, 432–441 (2018).
Zapatero, A. et al. High-dose radiotherapy with short-term or long-term androgen deprivation in localised prostate cancer (DART01/05 GICOR): a randomised, controlled, phase 3 trial. Lancet Oncol. 16, 320–327 (2015).
D’Amico, A. V., Chen, M.-H., Renshaw, A. A., Loffredo, M. & Kantoff, P. W. Androgen suppression and radiation vs radiation alone for prostate cancer. JAMA 299, 289–295 (2008).
Jones, C. U. et al. Radiotherapy and short-term androgen deprivation for localized prostate cancer. N. Engl. J. Med. 365, 107–118 (2011).
Denham, J. W. et al. Short-term neoadjuvant androgen deprivation and radiotherapy for locally advanced prostate cancer: 10-year data from the TROG 96.01 randomised trial. Lancet Oncol. 12, 451–459 (2011).
Sanda, M. G. et al. Clinically localized prostate cancer: AUA/ASTRO/SUO guideline. Part I: risk stratification, shared decision making, and care options. J. Urol. 199, 683–690 (2018).
Patel, S. A. et al. Stereotactic body radiotherapy versus conventional/moderate fractionated radiation therapy with androgen deprivation therapy for unfavorable risk prostate cancer. Radiat. Oncol. 15, 217 (2020).
Macias, V. A. & Barrera-Mellado, I. Ultra-hypofractionated radiation therapy for unfavourable intermediate-risk and high-risk prostate cancer is safe and effective: 5-year outcomes of a phase II trial. BJU Int. 125, 215–225 (2020).
Callan, L. et al. A phase I/II trial of fairly brief androgen suppression and stereotactic radiation therapy for high-risk prostate cancer (FASTR-2): preliminary results and toxicity analysis. Adv. Radiat. Oncol. 4, 668–673 (2019).
van Dams, R. et al. Stereotactic body radiotherapy for high-risk localized CARcinoma of the Prostate (SHARP) consortium: analysis of 344 prospectively treated patients. Int. J. Radiat. Oncol. Biol. Phys. 110, 731–737 (2021).
Zaorsky, N. G. et al. Prostate cancer radiation therapy recommendations in response to COVID-19. Adv. Radiat. Oncol. 5, 659–665 (2020).
Mcnair, H. A. et al. A systematic review: effectiveness of rectal emptying preparation in prostate cancer patients. Pract. Radiat. Oncol. 4, 437–447 (2014).
Heemsbergen, W. D. et al. Increased risk of biochemical and clinical failure for prostate patients with a large rectum at radiotherapy planning: results from the Dutch trial of 68 GY versus 78 Gy. Int. J. Radiat. Oncol. Biol. Phys. 67, 1418–1424 (2007).
De Crevoisier, R. et al. Increased risk of biochemical and local failure in patients with distended rectum on the planning CT for prostate cancer radiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 62, 965–973 (2005).
Moiseenko, V., Liu, M., Kristensen, S., Gelowitz, G. & Berthelet, E. Effect of bladder filling on doses to prostate and organs at risk: a treatment planning study. J. Appl. Clin. Med. Phys. 8, 55–68 (2006).
Ali, A. N. et al. Impact of magnetic resonance imaging on computed tomography-based treatment planning and acute toxicity for prostate cancer patients treated with intensity modulated radiation therapy. Pract. Radiat. Oncol. 3, e1–e9 (2013).
Buyyounouski, M. K. et al. Intensity-modulated radiotherapy with MRI simulation to reduce doses received by erectile tissue during prostate cancer treatment. Int. J. Radiat. Oncol. Biol. Phys. 58, 743–749 (2004).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03525262 (2021).
Patel, D., Tan, A., Brown, A. & Pain, T. Absence of prostate oedema obviates the need for delay between fiducial marker insertion and radiotherapy simulation. J. Med. Radiat. Sci. 67, 302–309 (2020).
Havnen, A., Liauw, S., Pelizzari, C. & Yenice, K. Image guided radiotherapy to the prostate after implantation of gold fiducials: is it necessary to wait 7 days for planning? Int. J. Radiat. Oncol. Biol. Phys. 72, S565–S566 (2008).
Linam, J. M., Yang, L. X. & Lee, J. W. No need to wait: fiducial migration in immediate versus delayed simulation for prostate IGRT. Int. J. Radiat. Oncol. Biol. Phys. 90, S824 (2014).
Moseley, D. J. et al. Comparison of localization performance with implanted fiducial markers and cone-beam computed tomography for on-line image-guided radiotherapy of the prostate. Int. J. Radiat. Oncol. Biol. Phys. 67, 942–953 (2007).
Dehnad, H. et al. Clinical feasibility study for the use of implanted gold seeds in the prostate as reliable positioning markers during megavoltage irradiation. Radiother. Oncol. 67, 295–302 (2003).
Iocolano, M. et al. Prostate fiducial marker placement in patients on anticoagulation: feasibility prior to prostate SBRT. Front. Oncol. 10, 203 (2020).
Gill, S. et al. Patient-reported complications from fiducial marker implantation for prostate image-guided radiotherapy. Br. J. Radiol. 85, 1011–1017 (2012).
Njeh, C. F., Parker, B. C. & Orton, C. G. Implanted fiducial markers are no longer needed for prostate cancer radiotherapy. Med. Phys. 44, 6113–6116 (2017).
Tøndel, H. et al. Radiotherapy for prostate cancer – does daily image guidance with tighter margins improve patient reported outcomes compared to weekly orthogonal verified irradiation? Results from a randomized controlled trial. Radiother. Oncol. 126, 229–235 (2018).
Ruggieri, R. et al. Volumetric-modulated arc stereotactic body radiotherapy for prostate cancer: dosimetric impact of an increased near-maximum target dose and of a rectal spacer. Br. J. Radiol. 88, 20140736 (2015).
Zelefsky, M. J. et al. Early tolerance and tumor control outcomes with high-dose ultrahypofractionated radiation therapy for prostate cancer. Eur. Urol. Oncol. 3, 748–755 (2020).
Levy, J. F. et al. Evaluating the cost-effectiveness of hydrogel rectal spacer in prostate cancer radiation therapy. Pract. Radiat. Oncol. 9, e172–e179 (2019).
Hutchinson, R. C., Sundaram, V., Folkert, M. & Lotan, Y. Decision analysis model evaluating the cost of a temporary hydrogel rectal spacer before prostate radiation therapy to reduce the incidence of rectal complications. Urol. Oncol. 34, 291.e19-26 (2016).
Edel, A. SpaceOAR Hydrogel — is the Difference Worthwhile? https://prostatecancerinfolink.net/2017/01/10/spaceoar-hydrogel-is-the-difference-worthwhile/#:∼:text=Is%20it%20worthwhile%20to%20treat,of%20bothersome%20acute%20rectal%20symptoms (2017).
Mariados, N. et al. Hydrogel spacer prospective multicenter randomized controlled pivotal trial: dosimetric and clinical effects of perirectal spacer application in men undergoing prostate image guided intensity modulated radiation therapy. Int. J. Radiat. Oncol. Biol. Phys. 92, 971–977 (2015).
Hall, W. A. et al. Considering benefit and risk before routinely recommending SpaceOAR. Lancet Oncol. 22, 11–13 (2021).
Salembier, C. et al. ESTRO ACROP consensus guideline on CT- and MRI-based target volume delineation for primary radiation therapy of localized prostate cancer. Radiother. Oncol. 127, 49–61 (2018).
Chaurasia, A. R. et al. Evaluating the potential benefit of reduced planning target volume margins for low and intermediate risk patients with prostate cancer using real-time electromagnetic tracking. Adv. Radiat. Oncol. 3, 630–638 (2018).
Norkus, D. et al. A randomized trial comparing hypofractionated and conventionally fractionated three-dimensional external-beam radiotherapy for localized prostate adenocarcinoma. Strahlenther. Onkol. 185, 715–721 (2009).
Norkus, D. et al. A randomized hypofractionation dose escalation trial for high risk prostate cancer patients: interim analysis of acute toxicity and quality of life in 124 patients. Radiat. Oncol. 8, 206 (2013).
Sanguineti, G. et al. Macroscopic hematuria after conventional or hypofractionated radiation therapy: results from a prospective phase 3 study. Int. J. Radiat. Oncol. Biol. Phys. 96, 304–312 (2016).
Hall, W. A. et al. NRG oncology updated international consensus atlas on pelvic lymph node volumes for intact and post-operative prostate cancer. Int. J. Radiat. Oncol. Biol. Phys. 109, 174–185 (2020).
Sarfaraz, M. CyberKnife® robotic arm stereotactic radiosurgery. J. Am. Coll. Radiol. 4, 563–565 (2007).
Alongi, F., Fiorentino, A. & De Bari, B. SBRT and extreme hypofractionation: a new era in prostate cancer treatments? Rep. Pract. Oncol. Radiother. 20, 411–416 (2015).
King, C. R. et al. Stereotactic body radiotherapy for localized prostate cancer: pooled analysis from a multi-institutional consortium of prospective phase II trials. Radiother. Oncol. 109, 217–221 (2013).
Saul, S. Geography has a role in Medicare cancer coverage. The New York Times https://www.nytimes.com/2008/12/17/health/policy/17knife.html (2008).
Avkshtol, V. et al. A comparison of robotic arm versus gantry linear accelerator stereotactic body radiation therapy for prostate cancer. Res. Rep. Urol. 8, 145–158 (2016).
Pawlicki, T. et al. Investigation of LINAC-based image-guided hypofractionated prostate radiotherapy. Med. Dosim. 32, 71–79 (2007).
Scobioala, S. et al. A treatment planning study comparing IMRT techniques and cyber knife for stereotactic body radiotherapy of low-risk prostate carcinoma. Radiat. Oncol. 14, 143 (2019).
Pathmanathan, A. U. et al. Magnetic resonance imaging-guided adaptive radiation therapy: a “Game Changer” for prostate treatment? Int. J. Radiat. Oncol. Biol. Phys. 100, 361–373 (2018).
Alongi, F. et al. 1.5T MR-guided and daily adapted SBRT for prostate cancer: feasibility, preliminary clinical tolerability, quality of life and patient-reported outcomes during treatment. Radiat. Oncol. 15, 69 (2020).
Corradini, S. et al. MR-guidance in clinical reality: current treatment challenges and future perspectives. Radiat. Oncol. 14, 92 (2019).
Lagendijk, J. J. W. et al. MRI/LINAC integration. Radiother. Oncol. 86, 25–29 (2008).
Eccles, C. L. & Campbell, M. Keeping up with the hybrid magnetic resonance linear accelerators: how do radiation therapists stay current in the era of hybrid technologies? J. Med. Imaging Radiat. Sci. 50, 195–198 (2019).
Morrison, A. Magnetic resonance guided radiotherapy: MR-simulation and MR-LINAC (CADTH, 2020).
Tetar, S. U. et al. Clinical implementation of magnetic resonance imaging guided adaptive radiotherapy for localized prostate cancer. Phys. Imaging Radiat. Oncol. 9, 69–76 (2019).
Viani, G. A. et al. Intensity-modulated radiotherapy reduces toxicity with similar biochemical control compared with 3-dimensional conformal radiotherapy for prostate cancer: a randomized clinical trial. Cancer 122, 2004–2011 (2016).
Michalski, J. M. et al. Preliminary toxicity analysis of 3-dimensional conformal radiation therapy versus intensity modulated radiation therapy on the high-dose arm of the Radiation Therapy Oncology Group 0126 prostate cancer trial. Int. J. Radiat. Oncol. Biol. Phys. 87, 932–938 (2013).
Kothari, G. et al. Stereotactic body radiotherapy for primary prostate cancer. Technol. Cancer Res. Treat. 17, 1533033818789633 (2018).
De Crevoisier, R. et al. Daily versus weekly prostate cancer image guided radiation therapy: phase 3 multicenter randomized trial. Int. J. Radiat. Oncol. Biol. Phys. 102, 1420–1429 (2018).
Bottero, M. et al. Electromagnetic transponder localization and real-time tracking for prostate cancer radiation therapy: clinical impact of metallic hip prostheses. Pract. Radiat. Oncol. 10, e538–e542 (2020).
Oehler, C. et al. PTV margin definition in hypofractionated IGRT of localized prostate cancer using cone beam CT and orthogonal image pairs with fiducial markers. Radiat. Oncol. 9, 229 (2014).
Loblaw, D. et al. Comparison of biochemical and toxicity outcomes from a contemporaneous cohort study of low-risk prostate cancer treated with different radiation techniques. Int. J. Radiat. Oncol. Biol. Phys. 87, S26 (2013).
Katz, A. J., Santoro, M., Ashley, R., Diblasio, F. & Witten, M. Stereotactic body radiotherapy for organ-confined prostate cancer. BMC Urol. 10, 1 (2010).
McBride, S. M. et al. Hypofractionated stereotactic body radiotherapy in low-risk prostate adenocarcinoma: preliminary results of a multi-institutional phase 1 feasibility trial. Cancer 118, 3681–3690 (2012).
Alongi, F. et al. Linac based SBRT for prostate cancer in 5 fractions with VMAT and flattening filter free beams: preliminary report of a phase II study. Radiat. Oncol. 8, 171 (2013).
Boike, T. P. et al. Phase I dose-escalation study of stereotactic body radiation therapy for low- and intermediate-risk prostate cancer. J. Clin. Oncol. 29, 2020–2026 (2011).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03367702 (2021).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT01794403 (2021).
Yong, J. H. E. et al. Cost-effectiveness of intensity-modulated radiotherapy in prostate cancer. Clin. Oncol. 24, 521–531 (2012).
Yong, J. H. E. et al. Estimating the costs of intensity-modulated and 3-dimensional conformal radiotherapy in Ontario. Curr. Oncol. 23, 228–238 (2016).
Cooperberg, M. R. et al. Primary treatments for clinically localised prostate cancer: a comprehensive lifetime cost-utility analysis. BJU Int. 111, 437–450 (2013).
Hummel, S. R., Stevenson, M. D., Simpson, E. L. & Staffurth, J. A model of the cost-effectiveness of intensity-modulated radiotherapy in comparison with three-dimensional conformal radiotherapy for the treatment of localised prostate cancer. Clin. Oncol. 24, e159–e167 (2012).
Konski, A. et al. Using decision analysis to determine the cost-effectiveness of intensity-modulated radiation therapy in the treatment of intermediate risk prostate cancer. Int. J. Radiat. Oncol. Biol. Phys. 66, 408–415 (2006).
Konski, A. Cost effectiveness of prostate cancer radiotherapy. Transl. Androl. Urol. 7, 371–377 (2018).
Zemplenyi, A. T. et al. Cost-effectiveness analysis of intensity-modulated radiation therapy with normal and hypofractionated schemes for the treatment of localised prostate cancer. Eur J Cancer Care https://doi.org/10.1111/ecc.12430 (2018).
Voong, K. R. et al. Long-term economic value of hypofractionated prostate radiation: Secondary analysis of a randomized trial. Adv. Radiat. Oncol. 2, 249–258 (2017).
Sharieff, W. et al. The technique, resources and costs of stereotactic body radiotherapy of prostate cancer: a comparison of dose regimens and delivery systems. Technol. Cancer Res. Treat. 15, 171–178 (2016).
Sher, D. J., Parikh, R. B., Mays-Jackson, S. & Punglia, R. S. Cost-effectiveness analysis of SBRT versus IMRT for low-risk prostate cancer. Am. J. Clin. Oncol. 37, 215–221 (2014).
Hodges, J. C. et al. Cost-effectiveness analysis of stereotactic body radiation therapy versus intensity-modulated radiation therapy: an emerging initial radiation treatment option for organ-confined prostate cancer. J. Oncol. Pract. 8, e31s–e337 (2012).
Parthan, A. et al. Comparative cost-effectiveness of stereotactic body radiation therapy versus intensity-modulated and proton radiation therapy for localized prostate cancer. Front. Oncol. 2, 81 (2012).
Moore, A. et al. The financial impact of hypofractionated radiation for localized prostate cancer in the United States. J. Oncol. 2019, 8170428 (2019).
Das, S. et al. Comparison of image-guided radiotherapy technologies for prostate cancer. Am. J. Clin. Oncol. 37, 616–623 (2014).
Van Dyk, J., Zubizarreta, E. & Lievens, Y. Cost evaluation to optimise radiation therapy implementation in different income settings: a time-driven activity-based analysis. Radiother. Oncol. 125, 178–185 (2017).
da Saude, M. Plano de Expansão da Radioterapia no SUS. https://www.saude.gov.br/ciencia-e-tecnologia-e-complexo-industrial/complexo-industrial/plano-de-expansao-da-radioterapia-no-sus (2020).
Rosa, A. A. Status da Radioterapia Nacional e Desafios do Setor. (Sociedade Brasileira de Radioterapia, 2020).
Ige, T. A. et al. Surveying the challenges to improve linear accelerator-based radiation therapy in africa: a unique collaborative platform of all 28 african countries offering such treatment. Clin. Oncol. https://doi.org/10.1016/j.clon.2021.05.008 (2021).
Balogun, O., Rodin, D., Ngwa, W., Grover, S. & Longo, J. Challenges and prospects for providing radiation oncology services in Africa. Semin. Radiat. Oncol. 27, 184–188 (2017).
Van Der Giessen, P. H. et al. Multinational assessment of some operational costs of teletherapy. Radiother. Oncol. 71, 347–355 (2004).
Lariviere, M. J., Zhu, T. C. & Christodouleas, J. P. Important technical considerations for implementing the ASTRO/ASCO/AUA prostate cancer hypofractionated radiation guideline. Pract. Radiat. Oncol. 9, 197–199 (2019).
Barton, M. B., Zubizarreta, E. & Gospodarowicz, M. Radiotherapy in low- and middle-income countries. What can we do differently? Clin. Oncol. 29, 69–71 (2017).
El Saghir, N. S. et al. Impact of merit-based immigration policies on brain drain from low- and middle-income countries. JCO Glob. Oncol. 6, 185–189 (2020).
Rodin, D. et al. Hypofractionated radiotherapy in the real-world setting: an international ESTRO-GIRO survey. Radiother. Oncol. 157, 32–39 (2021).
Abdel-Wahab, M., Fidarova, E. & Polo, A. Global access to radiotherapy in low- and middle-income countries. Clin. Oncol. 29, 99–104 (2017).
Mayr, N. A. et al. International outreach: what is the responsibility of ASTRO and the major international radiation oncology societies? Int. J. Radiat. Oncol. Biol. Phys. 89, 481–484 (2014).
Ngwa, W. et al. Potential for information and communication technologies to catalyze global collaborations in radiation oncology. Int. J. Radiat. Oncol. Biol. Phys. 91, 444–447 (2015).
Scrase, C., Alonzi, R., El-Gayed, A., Shouman, T. H. & Hopkins, K. Radiotherapy training programs in lower- and middle-income countries (LMIC) of Africa: experience of the International Atomic Energy Agency (IAEA) in upskilling contouring competencies in disease specific sites - prostate cancer. Int. J. Radiat. Oncol. Biol. Phys. 108, e438–e439 (2020).
Elmore, S. N. C. et al. Global palliative radiotherapy: a framework to improve access in resource-constrained settings. Ann. Palliat. Med. 8, 274–284 (2019).
Ngwa, W. et al. Closing the cancer divide through ubuntu: information and communication technology-powered models for global radiation oncology. Int. J. Radiat. Oncol. Biol. Phys. 94, 440–449 (2016).
Efstathiou, J. A. et al. Addressing the growing cancer burden in the wake of the AIDS epidemic in Botswana: The BOTSOGO collaborative partnership. Int. J. Radiat. Oncol. Biol. Phys. 89, 468–475 (2014).
Fisher, B. J. et al. Radiation oncology in Africa: improving access to cancer care on the african continent. Int. J. Radiat. Oncol. Biol. Phys. 89, 458–461 (2014).
Global RT. Union for International Cancer Control & Global Task Force on Radiotherapy for Cancer Control. http://globalrt.org (2021).
Berlin, A. et al. Clinical application of a novel voxel- and machine learning-based automated planning method for prostate volumetric arc radiation therapy. Int. J. Radiat. Oncol. Biol. Phys. 102, e533 (2018).
Feng, M., Valdes, G., Dixit, N. & Solberg, T. D. Machine learning in radiation oncology: opportunities, requirements, and needs. Front. Oncol. 8, 110 (2018).
Chamunyonga, C., Edwards, C., Caldwell, P., Rutledge, P. & Burbery, J. The impact of artificial intelligence and machine learning in radiation therapy: considerations for future curriculum enhancement. J. Med. Imaging Radiat. Sci. 51, 214–220 (2020).
International Atomic Energy Association. Directory of radiotherapy centres. (IAEA, 2020).
Bentzen, S. M. et al. Towards evidence-based guidelines for radiotherapy infrastructure and staffing needs in Europe: the ESTRO QUARTS project. Radiother. Oncol. 75, 355–365 (2005).
The Royal College of Radiologists. Radiotherapy Dose Fractionation Third Edition (Royal College of Radiologists, 2019).
Badmus, T. A. et al. Burden of prostate cancer in southwestern Nigeria. Urology 76, 412–416 (2010).
Magnus, F. E. & Ofoha, C. G. Presentation, characteristics and co-morbidities of men with prostate cancer in Nigeria. J. Adv. Med. https://doi.org/10.9734/jammr/2019/v31i530297 (2019).
Irabor, O. C. et al. Can the adoption of hypofractionation guidelines expand global radiotherapy access? An analysis for breast and prostate radiotherapy. JCO Glob. Oncol. 6, 667–678 (2020).
Author information
Authors and Affiliations
Contributions
M.Y., A.G.G., N.M., V.F.B., L.C.M. and F.Y.M. researched data for the article. A.G.G., F.L.C., L.C.M. and F.Y.M. made substantial contributions to discussions of content. M.Y., A.G.G., F.L.C., N.M., V.F.B., H.P., A.B. and F.Y.M. wrote the article. All authors reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
H.P. declares consulting fees and conference support from Varian Medica Systems unrelated to the current work. F.L.C. declares grants from Boston Scientific and Sanofi, honoraria and conference support from Varian Medical Systems and participates on the data safety monitoring board of Abbvie and Bayer. The other authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Urology thanks S. Arcangeli, F. Alongi and the other, anonymous, reviewers for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
AFRONET: https://www.iaea.org/resources/webinar/africa-radiation-oncology-network-afronet
BOTSOGO: http://www.botsogo.org/
Global RT: http://globalrt.org/
Radiating Hope: https://www.radiatinghope.org/
Glossary
- Alpha/beta ratio
-
The ratio of linear and quadratic components that make up the model of cancer cell killing in response to radiotherapy; a measure of intrinsic sensitivity of a cell to radiation-induced death.
- Cone-beam CT
-
(CBCT). A medical imaging technique utilizing divergent X-ray beams to perform CT. Often used for onboard image-guided radiotherapy.
- Co-registered
-
Within treatment planning systems, the fusion or overlay of two separate images, often of different modalities (for example, MRI and CT) to aid treatment planning.
- Soft-tissue matching
-
During image-guided radiotherapy, matching is performed before each treatment fraction to ensure treatment accuracy. In prostate radiotherapy using CBCT, the soft tissue interface between the rectum and prostate (as opposed to bony landmarks) are used for set-up verification.
- Dose constraint points
-
Accepted dosimetric values to ensure the safety of normal tissues. Often, these constraints are expressed as a maximal dose limit to a specified volume of a normal tissue.
- Megavoltage photons
-
Megavoltage is the most common energy level used in modern linear accelerators for the treatment of most cancers owing to its deep penetration. Other photon energies, such as kilovoltage or orthovoltage, can be used for superficial cancers such as skin cancers.
- Incremental cost-effectiveness ratio
-
(ICER). A summary measure representing the economic value of an intervention in comparison to an alternative (comparator). The ICER is usually expressed as a monetary amount per quality-adjusted life year.
- Quality-adjusted life year
-
(QALY). A measure of disease burden that accounts for the quality and quantity of life lived. QALY scores range from 1 (a year lived in perfect health) to 0 (death). Comorbid conditions will result in a QALY measure that is intermediate to these values.
Rights and permissions
About this article
Cite this article
Yan, M., Gouveia, A.G., Cury, F.L. et al. Practical considerations for prostate hypofractionation in the developing world. Nat Rev Urol 18, 669–685 (2021). https://doi.org/10.1038/s41585-021-00498-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41585-021-00498-6
This article is cited by
-
A randomized phase II trial of MR-guided prostate stereotactic body radiotherapy administered in 5 or 2 fractions for localized prostate cancer (FORT)
BMC Cancer (2023)
-
Preoperative hypofractionated radiotherapy for soft tissue sarcomas: a systematic review
Radiation Oncology (2022)
-
A global approach to improving penile cancer care
Nature Reviews Urology (2022)
-
Mortality and biochemical recurrence after surgery, brachytherapy, or external radiotherapy for localized prostate cancer: a 10-year follow-up cohort study
Scientific Reports (2022)