Abstract
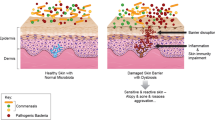
The skin is the largest organ in the human body, and it orchestrates many functions that are fundamentally important for our survival. Although the skin might appear to present a relatively inhospitable or even hostile environment, a multitude of commensals and also some potentially pathogenic microorganisms have successfully adapted to survive and/or thrive within the diverse ecological niches created by the skin’s topographical architecture. Dysbiosis within these microbial populations can result in the emergence and pathological progression of skin diseases. Unsurprisingly, this has led to a new focus of research both for the medical dermatology and cosmetic industries that is concerned with modulation of the skin microbiome to help address common microbially mediated or modulated conditions such as acne, body odour, and atopic dermatitis. This review presents an overview of our current understanding of the complex relationship of the skin with its microbiome and then introduces the concept of probiotic intervention for the management of microbial dysbiosis within the skin ecosystem.




Similar content being viewed by others
References
Sender R, Fuchs S, Milo R (2016) Revised estimates for the number of human and bacteria cells in the body. PLoS Biol 14(8):e1002533. https://doi.org/10.1371/journal.pbio.1002533
Grice EA, Segre JA (2011) The skin microbiome. Nat Rev Microbiol 9:244–253. https://doi.org/10.1038/nrmicro2537
Oh J, Byrd AL, Park M, Kong HH, Segre JA (2016) Temporal stability of the human skin microbiome. Cell 165(4):854–866. https://doi.org/10.1016/j.cell.2016.04.008
Schommer NN, Gallo RL (2013) Structure and function of the human skin microbiome. Trends in Microbiology 21:660–668. https://doi.org/10.1016/j.tim.2013.10.001
Cooper AJ, Weyrich LS, Dixit S, Farrer AG (2015) The skin microbiome: associations between altered microbial communities and disease. Aust J Dermatol 56:268–274. https://doi.org/10.1111/ajd.12253
Iizumi T, Battaglia T, Ruiz V, Perez Perez GI (2017) Gut microbiome and antibiotics. Arch Med Res 48:727–734. https://doi.org/10.1016/j.arcmed.2017.11.004
Kong HH (2011) Skin microbiome: genomics-based insights into the diversity and role of skin microbes [Internet]. Trends Mol Med 17:320–328. https://doi.org/10.1016/j.molmed.2011.01.013
Ursell LK, Clemente JC, Rideout JR, Gevers D, Caporaso JG, Knight R (2012) The interpersonal and intrapersonal diversity of human-associated microbiota in key body sites. J Allergy Clin Immunol [Internet] 129(5):1204–1208. https://doi.org/10.1016/j.jaci.2012.03.010
Huttenhower C, Gevers D, Knight R, Abubucker S, Badger JH, Chinwalla AT et al (2012) Structure, function and diversity of the healthy human microbiome. Nature 486(7402):207–214. https://doi.org/10.1038/nature11234
Kolarsick P, Kolarsick M, Goodwin C (2011) Anatomy and physiology of the skin. J Dermatol Nurses Assoc 3:203–213. https://doi.org/10.1097/JDN.0b013e3182274a98
Prausnitz MR, Elias PM, Franz TJ, Schmuth M, Tsai J-C, Menon GK, Holleran WM, Feingold KR (2012) Skin barrier and transdermal drug delivery. Dermatology 3:2065–2073
Losquadro WD (2017) Anatomy of the skin and the pathogenesis of nonmelanoma skin cancer. Facial Plastic Surgery Clinics of North America. W.B. Saunders 25:283–289. https://doi.org/10.1016/j.fsc.2017.03.001
Tobin DJ (2011) The anatomy and physiology of the skin. Springer Publishing Company, New York
Niemeyer - van der Kolk T, van der Wall HEC, Balmforth C, Van Doorn MBA, Rissmann R (2018) A systematic literature review of the human skin microbiome as biomarker for dermatological drug development. Br J Clin Pharmacol 84:2178–2193. https://doi.org/10.1111/bcp.13662
Tavaria FK (2017) Topical use of probiotics: the natural balance. Porto Biomed J [Internet] 2(3):69–70. https://doi.org/10.1007/s13555-020-00476-7
Byrd AL, Belkaid Y, Segre JA (2018) The human skin microbiome. Nat Rev Microbiol 16:143–155. https://doi.org/10.1038/nrmicro.2017.157
Belkaid Y, Segre JA (2014) Dialogue between skin microbiota and immunity. Science 346:954–959. https://doi.org/10.1126/science.1260144
Dréno B, Araviiskaia E, Berardesca E, Gontijo G, Sanchez Viera M, Xiang LF et al (2016) Microbiome in healthy skin, update for dermatologists. J Eur Acad Dermatol Venereol 30:2038–2047. https://doi.org/10.1111/jdv.13965
Friedrich AD, Paz ML, Leoni J, Maglio DHG (2017) Message in a bottle: dialog between intestine and skin modulated by probiotics. Int J Mol Sci MDPI AG 18. https://doi.org/10.3390/ijms18061067
Sanford JA, Gallo RL (2013) Functions of the skin microbiota in health and disease. Seminars in Immunology. Semin Immunol 25:370–377. https://doi.org/10.1016/j.smim.2013.09.005
Chiller K, Selkin BA, Murakawa GJ (2001) Skin microflora and bacterial infections of the skin. J Investig Dermatology Symp Proc 6(3):170–174. https://doi.org/10.1046/j.0022-202x.2001.00043.x
Nakamizo S, Egawa G, Honda T, Nakajima S, Belkaid Y, Kabashima K (2015) Commensal bacteria and cutaneous immunity. Semin Immunopathol 37:73–80. https://doi.org/10.1007/s00281-014-0452-6
Poretsky R, Rodriguez-R LM, Luo C, Tsementzi D, Konstantinidis KT (2014) Strengths and limitations of 16S rRNA gene amplicon sequencing in revealing temporal microbial community dynamics. PLoS One 9(4). https://doi.org/10.1371/journal.pone.0093827
Venter JC, Adams MD, Sutton GG, Kerlavage AR, Smith HO, Hunkapiller M (1998) Shotgun sequencing of the human genome. Science 280:1540–1542. https://doi.org/10.1126/science.280.5369.1540
Burton JP, Wescombe PA, Macklaim JM, Chai MHC, MacDonald K, Hale JDF et al (2013) Persistence of the oral probiotic Streptococcus salivarius M18 is dose dependent and megaplasmid transfer can augment their bacteriocin production and adhesion characteristics. PLoS One 8(6). https://doi.org/10.1371/journal.pone.0065991
Christensen GJM, Brüggemann H (2014) Bacterial skin commensals and their role as host guardians. Benef Microbes 5:201–215. https://doi.org/10.3920/BM2012.0062
Egert M, Simmering R, Riedel CU (2017) The association of the skin microbiota with health, immunity, and disease. Clin Pharmacol Ther 102(1):62–69. https://doi.org/10.1002/cpt.698
Nakatsuji T, Chen TH, Narala S, Chun KA, Two AM, Yun T et al (2017) Antimicrobials from human skin commensal bacteria protect against Staphylococcus aureus and are deficient in atopic dermatitis. Sci Transl Med 9(378). https://doi.org/10.1126/scitranslmed.aah4680
Kloos WE, Musselwhite MS (1975) Distribution and persistence of Staphylococcus and Micrococcus species and other aerobic bacteria on human skin. Appl Microbiol 30(3):381–385. https://doi.org/10.1128/am.30.3.381-395.1975
Clausen ML, Edslev SM, Andersen PS, Clemmensen K, Krogfelt KA, Agner T (2017) Staphylococcus aureus colonization in atopic eczema and its association with filaggrin gene mutations. Br J Dermatol 177(5):1394–400. https://doi.org/10.1111/bjd.15470
Rather IA, Bajpai VK, Kumar S, Lim J, Paek WK, Park YH (2016) Probiotics and atopic dermatitis: an overview. Front Microbiol 7:507. https://doi.org/10.3389/fmicb.2016.00507
Knackstedt R, Knackstedt T, Gatherwright J (2020) The role of topical probiotics in skin conditions: a systematic review of animal and human studies and implications for future therapies. Exp Dermatol 29:15–21. https://doi.org/10.1111/exd.14032
Noble SM, Gianetti BA, Witchley JN (2017) Candida albicans cell-type switching and functional plasticity in the mammalian host. Nat Rev Microbiol 15:96–108. https://doi.org/10.1038/nrmicro.2016.157
Maguire M, Maguire G (2017) The role of microbiota, and probiotics and prebiotics in skin health. Arch Dermatol Res 309(6):411–421. https://doi.org/10.1007/s00403-017-1750-3
Neuman H, Forsythe P, Uzan A, Avni O, Koren O (2018) Antibiotics in early life: dysbiosis and the damage done. FEMS Microbiol Rev 42:489–499. https://doi.org/10.1093/femsre/fuy018
Vangay P, Ward T, Gerber JS, Knights D (2015) Antibiotics, pediatric dysbiosis, and disease. Cell Host Microbe 17:553–564. https://doi.org/10.1016/j.chom.2015.04.006
Kang BS, Seo JG, Lee GS, Kim JH, Kim SY, Han YW et al (2009) Antimicrobial activity of enterocins from Enterococcus faecalis SL-5 against Propionibacterium acnes, the causative agent in acne vulgaris, and its therapeutic effect. J Microbiol 47(1):101–109. https://doi.org/10.1007/s12275-008-0179-y
Flohr C, Pascoe D, Williams HC (2005) Atopic dermatitis and the “hygiene hypothesis”: too clean to be true? Br J Dermatol 152:202–216. https://doi.org/10.1111/j.1365-2133.2004.06436.x
Lee GR, Maarouf M, Hendricks AJ, Lee DE, Shi VY (2019) Topical probiotics: the unknowns behind their rising popularity. Dermatol 25(5). https://doi.org/10.5070/D3255044062
Ege MJ (2017) The hygiene hypothesis in the age of the microbiome. Ann Am Thorac Soc 14:S348–S353. https://doi.org/10.1513/AnnalsATS.201702-139AW
Gibbs S, Surridge H, Adamson R, Cohen B, Bentham G, Reading R (2004) Atopic dermatitis and the hygiene hypothesis: a case-control study. Int J Epidemiol 33(1):199–207. https://doi.org/10.1093/ije/dyg267
Milani C, Duranti S, Bottacini F, Casey E, Turroni F, Mahony J et al (2017) The first microbial colonizers of the human gut: composition, activities, and health implications of the infant gut microbiota. Microbiol Mol Biol Rev 81(4). https://doi.org/10.1128/mmbr.00036-17
Chu DM, Ma J, Prince AL, Antony KM, Seferovic MD, Aagaard KM (2017) Maturation of the infant microbiome community structure and function across multiple body sites and in relation to mode of delivery. Nat Med 23(3):314–326. https://doi.org/10.1038/nm.4272
Schneider AM, Nelson AM (2019) Skin microbiota: friend or foe in pediatric skin health and skin disease. Pediatr Dermatol 36:815–22. https://doi.org/10.1111/pde.13955
Kim SK, Guevarra RB, Kim YT, Kwon J, Kim H, Cho JH et al (2019) Role of probiotics in human gut microbiome-associated diseases. J Microbiol Biotechnol 29(9):1335–1340. https://doi.org/10.4014/jmb.1906.06064
Dunn AB, Jordan S, Baker BJ, Carlson NS (2017) The maternal infant microbiome: considerations for labor and birth. MCN Am J Matern Nurs 42(6):318–325. https://doi.org/10.1097/NMC.0000000000000373
Francino MP (2018) Birth mode-related differences in gut microbiota colonization and immune system development. Ann Nutr Metab 73:12–16. https://doi.org/10.1159/000490842
Reid G, Younes JA, Van Der Mei HC, Gloor GB, Knight R, Busscher HJ (2011) Microbiota restoration: natural and supplemented recovery of human microbial communities. Nat Rev Microbiol 9:27–38. https://doi.org/10.1038/nrmicro2473
Wallen-Russell C, Wallen-Russell S (2017) Meta analysis of skin microbiome: new link between skin microbiota diversity and skin health with proposal to use this as a future mechanism to determine whether cosmetic products damage the skin. Cosmetics 4. https://doi.org/10.3390/cosmetics4020014
Salverda JGW, Bragt PJC, De Wit-Bos L, Rustemeyer T, Coenraads PJ, Tupker RA et al (2013) Results of a cosmetovigilance survey in the Netherlands. Contact Dermatitis 68(3):139–148. https://doi.org/10.1111/cod.12005
Lambers H, Piessens S, Bloem A, Pronk H, Finkel P (2006) Natural skin surface pH is on average below 5, which is beneficial for its resident flora. Int J Cosmet Sci 28(5):359–370. https://doi.org/10.1111/j.1467-2494.2006.00344.x
Scharschmidt TC, Fischbach MA (2013) What lives on our skin: ecology, genomics and therapeutic opportunities of the skin microbiome. Drug Discov Today Dis Mech 10. https://doi.org/10.1016/j.ddmec.2012.12.003
Xu H, Li H (2019) Acne, the skin microbiome, and antibiotic treatment. Am J Clin Dermatol 20:335–44. https://doi.org/10.1007/s40257-018-00417-3
Mottin VHM, Suyenaga ES (2018) An approach on the potential use of probiotics in the treatment of skin conditions: acne and atopic dermatitis. Int J Dermatol 57:1425–32. https://doi.org/10.1111/ijd.13972
Lolou V, Panayiotidis MI (2019) Functional role of probiotics and prebiotics on skin health and disease. Fermentation 5. https://doi.org/10.3390/fermentation5020041
Kobayashi T, Glatz M, Horiuchi K, Kawasaki H, Akiyama H, Kaplan DH et al (2015) Dysbiosis and Staphyloccus aureus colonization drives inflammation in atopic dermatitis. Immunity 42(4):756–766. https://doi.org/10.1016/j.immuni.2015.03.014
Pereira LB (2014) Impetigo - Review. Anais Brasileiros de Dermatologia. Sociedade Brasileira de Dermatologia 89:293–299. https://doi.org/10.1590/abd1806-4841.20142283
Callewaert C, Hutapea P, Van de Wiele T, Boon N (2014) Deodorants and antiperspirants affect the axillary bacterial community. Arch Dermatol Res 306(8):701–710. https://doi.org/10.1007/s00403-014-1487-1
Visser MJE, Kell DB, Pretorius E (2019) Bacterial dysbiosis and translocation in psoriasis vulgaris. Front Cell Infect Microbiol 9:7. https://doi.org/10.3389/fcimb.2019.00007
Benhadou F, Mintoff D, Schnebert B, Thio HB (2018) Psoriasis and microbiota: a systematic review. Dis (Basel, Switzerland) 6(2):47. https://doi.org/10.3390/diseases6020047
Natsch A (2015) What makes us smell: the biochemistry of body odour and the design of new deodorant ingredients. Chimia (Aarau) 69(7):414–420. https://doi.org/10.2533/chimia.2015.414
James AG, Austin CJ, Cox DS, Taylor D, Calvert R (2013) Microbiological and biochemical origins of human axillary odour. FEMS Microbiol Ecol 83:527–540. https://doi.org/10.1111/1574-6941.12054
Ilkit M, Durdu M (2015) Tinea pedis: the etiology and global epidemiology of a common fungal infection. Crit Rev Microbiol 41:374–88. https://doi.org/10.3109/1040841X.2013.856853
Liu X, Tan J, Yang H, Gao Z, Cai Q, Meng L et al (2019) Characterization of skin microbiome in tinea pedis. Indian J Microbiol 59(4):422–427. https://doi.org/10.1007/s12088-019-00816-y
Brown J, Shriner DL, Schwartz RA, Janniger CK (2003) Impetigo: an update. Int J Dermatol 251–255. https://doi.org/10.1046/j.1365-4362.2003.01647.x
Mackowiak PA (2013) Recycling Metchnikoff: probiotics, the intestinal microbiome and the quest for long life. Front Public Heal. https://doi.org/10.3389/fpubh.2013.00052
Wescombe PA, Burton JP, Cadieux PA, Klesse NA, Hyink O, Heng NC et al (2006) Megaplasmids encode differing combinations of lantibiotics in Streptococcus salivarius. Antonie Van Leeuwenhoek. https://doi.org/10.1007/s10482-006-9081-y
Lee DE, Huh CS, Ra J, Choi ID, Jeong JW, Kim SH et al (2015) Clinical evidence of effects of Lactobacillus plantarum HY7714 on skin aging: a randomized, double blind, placebo-controlled study. J Microbiol Biotechnol 25(12):2160–2168. https://doi.org/10.4014/jmb.1509.09021
Scariya L, Nagarathna DV, Varghese M (2015) Probiotics in periodontal therapy. Int J Pharma Bio Sci 6(1):P242–P250. https://doi.org/10.5455/musbed.20141106034910
Salminen S, Collado MC, Endo A, Hill C, Lebeer S, Quigley EMM et al (2021) The International Scientific Association of Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of postbiotics. Nat Rev Gastroenterol Hepatol. https://doi.org/10.1038/s41575-021-00440-6
Blanchet-Réthoré S, Bourdès V, Mercenier A, Haddar CH, Verhoeven PO, Andres P (2017) Effect of a lotion containing the heat-treated probiotic strain Lactobacillus johnsonii NCC 533 on Staphylococcus aureus colonization in atopic dermatitis. Clin Cosmet Investig Dermatol 10:249–257. https://doi.org/10.2147/CCID.S135529
Lebeer S, Oerlemans E, Claes I, Wuyts S, Henkens T, Spacova I et al (2018) Topical cream with live lactobacilli modulates the skin microbiome and reduce acne symptoms. bioRxiv 463307. https://doi.org/10.1101/463307
Lopes EG, Moreira DA, Gullón P, Gullón B, Cardelle-Cobas A, Tavaria FK (2017) Topical application of probiotics in skin: adhesion, antimicrobial and antibiofilm in vitro assays. J Appl Microbiol 122(2):450–461. https://doi.org/10.1111/jam.13349
Karska-Wysocki B, Bazo M, Smoragiewicz W (2010) Antibacterial activity of Lactobacillus acidophilus and Lactobacillus casei against methicillin-resistant Staphylococcus aureus (MRSA). Microbiol Res 165(8):674–686. https://doi.org/10.1016/j.micres.2009.11.008
Benic GZ, Farella M, Morgan XC, Viswam J, Heng NC, Cannon RD et al (2019) Oral probiotics reduce halitosis in patients wearing orthodontic braces: a randomized, triple-blind, placebo-controlled trial. J Breath Res 13(3):36010. https://doi.org/10.1016/j.micres.2009.11.008
Gibson GR, Hutkins R, Sanders ME, Prescott SL, Reimer RA, Salminen SJ et al (2017) Expert consensus document: the International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of prebiotics. Nat Rev Gastroenterol Hepatol 14(8):491–502. https://doi.org/10.1038/nrgastro.2017.75
Wegh CAM, Geerlings SY, Knol J, Roeselers G, Belzer C (2019) Postbiotics and their potential applications in early life nutrition and beyond. Int J Mol Sci 20. https://doi.org/10.3390/ijms20194673
Akter S, Park JH, Jung HK (2020) Potential health-promoting benefits of paraprobiotics, inactivated probiotic cells. J Microbiol Biotechnol 30:477–481. https://doi.org/10.4014/JMB.1911.11019
Osborne DW, Tan PI, Varma T, Carbol J (2018) Formulating topical products containing live microorganisms as the active ingredient. Pharm Technol 42(3):32–36
Dolan KE, Pizano JM, Gossard CM, Williamson CB, Burns CM, Gasta MG et al (2017) Probiotics and disease: a comprehensive summary-part 6, skin health. Integr Med 16(4):32–41
Marto J, Ascenso A, Simoes S, Almeida AJ, Ribeiro HM (2016) Pickering emulsions: challenges and opportunities in topical delivery. Expert Opin Drug Deliv 13:1093–107. https://doi.org/10.1080/17425247.2016.1182489
Sreeja V, Prajapati JB (2013) Probiotic formulations: application and status as pharmaceuticals-a review. Probiotics Antimicrob Proteins 5(2):81–91. https://doi.org/10.1080/17425247.2016.1182489
Makinen K, Berger B, Bel-Rhlid R, Ananta E (2012) Science and technology for the mastership of probiotic applications in food products. J Biotechnol 162(4):356–365. https://doi.org/10.1016/j.jbiotec.2012.07.006
Acknowledgements
The authors acknowledge that the figures were created with Biorender.com.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
I.J.M. and E.M.W. were interns at Blis Technologies, the manufacturer of a skin probiotic.
R.J., J.R.T. and J.D.F.H. are employees of Blis Technologies.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
McLoughlin, I.J., Wright, E.M., Tagg, J.R. et al. Skin Microbiome—The Next Frontier for Probiotic Intervention. Probiotics & Antimicro. Prot. 14, 630–647 (2022). https://doi.org/10.1007/s12602-021-09824-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12602-021-09824-1