Abstract
Background and aims
Whether herbal and dietary supplements (HDS) are safer than Western conventional drugs is controversial. The aim of this study was to explore the characteristics and risk factors for HDS-induced liver injury (HILI) in Taiwan.
Methods
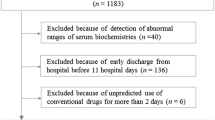
This is a 9-year multi-center prospective study conducted in Taiwan from 2011 to 2019. Patients with HILI were compared to those with conventional drug-induced liver injury (CILI).
Results
A total of 1,297 patients were enrolled, of whom 285 (22.0%) had HILI and 1,012 (78.0%) had CILI. Compared to the CILI group, the HILI group had higher initial serum alanine aminotransferase, alkaline phosphatase (ALP), peak ALP and bilirubin levels, and higher rates of jaundice, ascites, encephalopathy, coagulopathy, sepsis and acute liver failure. In addition, the HILI group had a higher mortality rate than the CILI group (12.6 vs. 8.0%, p = 0.016). Hepatitis B carrier status, elevated baseline liver biochemical tests and the use of crude herbs (without processing) were associated with an increased risk of HILI-related mortality (adjusted hazard ratios [95% confidence intervals]: 2.90 [1.43–5.99], 2.40 [1.01–5.68] and 2.94 [1.45–5.97], respectively).
Conclusions
HDS are popular and incriminated in more than one-fifth of drug-induced liver injuries in Taiwan. The patients with HILI were more severe than those with CILI in terms of liver biochemical tests, complications and mortality. Hepatitis B carriers, those with elevated baseline liver tests and crude herb users may have a higher risk of HILI-related mortality. The prudent use of HDS is suggested in these high-risk subjects.


Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Devarbhavi H, Aithal G, Treeprasertsuk S, et al. Drug-induced liver injury: Asia Pacific Association of Study of Liver consensus guidelines. Hepatol Int 2021;15:258–282
Devarbhavi H, Choudhury AK, Sharma MK, APASL ACLF working party, et al. Drug-induced acute-on-chronic liver failure in Asian patients. Am J Gastroenterol 2019;114:929–937
Devarbhavi H, Patil M, Reddy VV, et al. Drug-induced acute liver failure in children and adults: results of a single-centre study of 128 patients. Liver Int 2018;38:1322–1329
Navarro VJ, Lucena MI. Hepatotoxicity induced by herbal and dietary supplements. Semin Liver Dis 2014;34:172–193
Navarro VJ, Barnhart H, Bonkovsky HL, et al. Liver injury from herbals and dietary supplements in the US drug-induced liver injury network. Hepatology 2014;60:1399–1408
Seeff LB, Bonkovsky HL, Navarro VJ, et al. Herbal products and the liver: a review of adverse effects and mechanisms. Gastroenterology 2015;148:517–532
Teschke R, Andrade RJ. Drug, herb, and dietary supplement hepatotoxicity. Int J Mol Sci 2016;17(9):1488
Navarro VJ, Khan I, Björnsson E, et al. Liver injury from herbal and dietary supplements. Hepatology 2017;65:363–373
Teschke R, Danan G. Worldwide use of RUCAM for causality assessment in 81,856 idiosyncratic DILI and 14,029 HILI cases published 1993-Mid 2020: a comprehensive analysis. Medicines (Basel) 2020;79(10):62
Jing J, Teschke R. Traditional Chinese medicine and herb-induced liver injury: comparison with drug-induced liver injury. J Clin Transl Hepatol 2018;6:57–68
Teschke R, Zhu Y, Jing J. Herb-induced liver injury in Asia and current role of RUCAM for causality assessment in 11,160 published cases. J Clin Transl Hepatol 2020;8:200–214
Chalasani N, Bonkovsky HL, Fontana R, et al. Features and outcomes of 899 patients with drug-induced liver injury: the DILIN prospective study. Gastroenterology 2015;148:1340–1352
Shen T, Liu Y, Shang J, et al. Incidence and etiology of drug-induced liver injury in mainland China. Gastroenterology 2019;156:2230–2241
Chih LH, On AWF, Huang YS. Correlation of anti-tuberculosis drug-related liver injury and liver function monitoring: a 12 years’ experience in Taiwan Drug Relieve Foundation. J Food Drug Anal 2014;22:356–362
Fontana RJ, Watkins PB, Bonkovsky HL, DILIN Study Group. Drug-Induced Liver Injury Network (DILIN) prospective study: rationale, design and conduct. Drug Saf 2009;32:55–68
Danan G, Benichou C. Causality assessment of adverse reactions to drugs—I. A novel method based on the conclusions of international consensus meeting: application to drug-induced liver injuries. J Clin Epidemiol 1993;46:1323–1330
Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology 2018;67:328–357
Sterling RK, Lissen E, Clumeck N, et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology 2006;43:1317–1325
Wendon J, Cordoba J, Dhawan A, et al. EASL clinical practical guidelines on the management of acute (fulminant) liver failure. J Hepatol 2017;66:1047–1081
Arroyo V, Moreau R, Jalan R, EASL-CLIF Consortium CANONIC Study, et al. Acute-on-chronic liver failure: a new syndrome that will re-classify cirrhosis. J Hepatol 2015;62(1 Suppl):S131−S143
Medina-Caliz I, Garcia-Cortes M, Gonzalez-Jimenez A, et al. Herbal and dietary supplement-induced liver injuries in the Spanish DILI Registry. Clin Gastroenterol Hepatol 2018;16:1495–1502
Stephens C, Robles-Diaz M, Medina-Caliz I, et al. Comprehensive analysis and insights gained from long-term experience of the Spanish DILI Registry. J Hepatol 2021;75:86–97
Bessone F, García-Cortés M, Medina-Caliz I, et al. Herbal and dietary supplements-induced liver injury in Latin America: Experience from the Latindili Network. Clin Gastroenterol Hepatol 2021. (Epub ahead of print)
Devarbhavi H, Joseph T, Sunil Kumar N, The Indian Network of Drug-Induced Liver Injury, et al. Etiology, clinical features, outcome and prognostic markers in 1288 patients. J Clin Exp Hepatol 2021;11:288–298
Suk KT, Kim DJ, Kim CH, et al. A prospective nationwide study of drug-induced liver injury in Korea. Am J Gastroenterol 2012;107:1380–1387
Radimer K, Bindewald B, Hughes J, et al. Dietary supplement use by US adults: data from the National Health and Nutrition Examination Survey, 1999–2000. Am J Epidemiol 2004;160:339–349
Wong WM, Wu PC, Yuen MF, et al. Antituberculosis drug-related liver dysfunction in chronic hepatitis B infection. Hepatology 2000;31:201–206
Wang NT, Huang YS, Lin MH, et al. Chronic hepatitis B infection and risk of anti-tuberculosis drug-induced liver injury: systematic review and meta-analysis. J Chin Med Assoc 2016;79:368–374
Philips CA, Paramaguru R, Joy AK, et al. Clinical outcomes, histopathological patterns, and chemical analysis of Ayurveda and herbal medicine associated with severe liver injury—a single-center experience from southern India. Indian J Gastroenterol 2018;37:9–17
Philips CA, Paramaguru R, Augustine P, et al. A single-center experience on outcomes of complementary and alternative medicine use among patients with cirrhosis. Hepatol Commun 2019;3:1001–1012
Sarin SK, Choudhury A, Sharma MK, APASL ACLF Research Consortium (AARC) for APASL ACLF working Party, et al. Acute-on-chronic liver failure: consensus recommendations of the Asian Pacific association for the study of the liver (APASL): an update. Hepatol Int 2019;13:353–390
Davern TJ, Chalasani N, Fontana RJ, Drug-Induced Liver Injury Network (DILIN), et al. Acute hepatitis E infection accounts for some cases of suspected drug-induced liver injury. Gastroenterology 2011;141:1665–1672
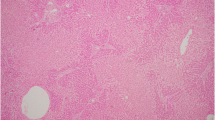
Acknowledgements
The authors thanks Yi-Chen Yeh, MD, and Fen-Yau Li, MD, Department of Pathology and Laboratory Medicine, Taipei Veterans General Hospital, for their reading and interpretation of the liver pathology.
Funding
The study was supported by the Grants from Taiwan Food and Drug Administration (TFDA), Ministry of Health and Welfare, Taiwan (DOH100-99TFDA-P-092 and DOH101-FDA-41103), and Taipei Veterans General Hospital, Taiwan (V110C-022).
Author information
Authors and Affiliations
Contributions
YSH: study concept and design, data collection and interpretation, statistical analysis, and drafting manuscript. TTC: study concept and design, data collection and interpretation, and manuscript editing for important intellectual contents. CYP: data collection and interpretation, and manuscript editing for important intellectual contents. GHL: data collection and interpretation, and manuscript editing for important intellectual contents. CWH: data collection and interpretation, and manuscript editing for important intellectual contents. CTH: data collection and interpretation, and manuscript editing for important intellectual contents. YHH: manuscript review for important intellectual contents. All authors were responsible for reading and approving the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Yi-Shin Huang, Ting-Tsung Chang, Cheng-Yuan Peng, Gin-Ho Lo, Chao-Wei Hsu, Chi-Tan Hu, and Yi-Hsiang Huang declare that they have no conflict of interest.
Animal research (ethics)
The present study is not an animal research.
Consent to participate (ethics)
Our research complies with the guidelines for human studies and has been conducted ethically in accordance with the World Medical Association Declaration of Helsinki. This study was approved by the Institutional Review Board of each participating hospital for all the data collection and analysis.
Consent to publish (ethics)
Not applicable.
Plant reproducibility
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Huang, YS., Chang, TT., Peng, CY. et al. Herbal and dietary supplement-induced liver injury in Taiwan: comparison with conventional drug-induced liver injury. Hepatol Int 15, 1456–1465 (2021). https://doi.org/10.1007/s12072-021-10241-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-021-10241-3