Abstract
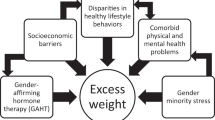
An increasing number of transgender and gender-diverse (TGD) youth (early pubertal through to late adolescent, typically 9–10 through to 18 years of age) are seeking medical services to bring their physical sex characteristics into alignment with their gender identity — their inner sense of self as male or female or somewhere on the gender spectrum. Compelling research has demonstrated the clear mental health — even life-saving — benefits of gender-affirming care, but current clinical practice guidelines and standards of care are based on only several short-term and a few medium-term outcomes studies complemented by expert opinion. Nevertheless, although the relative paucity of outcomes data raises concerns, the stance of not intervening until more is known is not a neutral option, and large observational studies evaluating current models of care are necessary and are now underway. This Review highlights key advances in our understanding of transgender and gender-diverse youth, the challenges of providing gender-affirming care, gaps in knowledge and priorities for research.
Key points
-
Being transgender or gender diverse (TGD) is not rare and is no longer considered pathological; it represents an example of human diversity.
-
Scientific evidence supports biological underpinnings to gender identity development.
-
Gender-affirming medical care has clear mental health benefits, some of which might even be life-saving.
-
Long-term safety and efficacy studies are necessary to optimize care for TGD youth.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Skordis, N., Butler, G., de Vries, M. C., Main, K. & Hannema, S. E. ESPE and PES international survey of centers and clinicians delivering specialist care for children and adolescents with gender dysphoria. Horm. Res. Paediatr. 90, 326–331 (2018).
Arnoldussen, M. et al. Re-evaluation of the Dutch approach: are recently referred transgender youth different compared to earlier referrals? Eur. Child. Adolesc. Psychiatry 29, 803–811 (2020).
Polderman, T. J. C. et al. The biological contributions to gender identity and gender diversity: bringing data to the table. Behav. Genet. 48, 95–108 (2018).
Hare, L. et al. Androgen receptor repeat length polymorphism associated with male-to-female transsexualism. Biol. Psychiatry 65, 93–96 (2009).
Foreman, M. et al. Genetic link between gender dysphoria and sex hormone signaling. J. Clin. Endocrinol. Metab. 104, 390–396 (2019).
Theisen, J. G. et al. The use of whole exome sequencing in a cohort of transgender individuals to identify rare genetic variants. Sci. Rep. 9, 20099 (2019).
Dessens, A. B., Slijper, F. M. & Drop, S. L. Gender dysphoria and gender change in chromosomal females with congenital adrenal hyperplasia. Arch. Sex. Behav. 34, 389–397 (2005).
Pasterski, V. et al. Increased cross-gender identification independent of gender role behavior in girls with congenital adrenal hyperplasia: results from a standardized assessment of 4- to 11-year-old children. Arch. Sex. Behav. 44, 1363–1375 (2015).
Meyer-Bahlburg, H. F., Dolezal, C., Baker, S. W., Ehrhardt, A. A. & New, M. I. Gender development in women with congenital adrenal hyperplasia as a function of disorder severity. Arch. Sex. Behav. 35, 667–684 (2006).
Luders, E. et al. Regional gray matter variation in male-to-female transsexualism. Neuroimage 46, 904–907 (2009).
Rametti, G. et al. White matter microstructure in female to male transsexuals before cross-sex hormonal treatment. A diffusion tensor imaging study. J. Psychiatr. Res. 45, 199–204 (2011).
Hoekzema, E. et al. Regional volumes and spatial volumetric distribution of gray matter in the gender dysphoric brain. Psychoneuroendocrinology 55, 59–71 (2015).
Mueller, S. C. et al. The neuroanatomy of transgender identity: mega-analytic findings from the ENIGMA transgender persons working group. J. Sex. Med. 18, 1122–1129 (2021).
Berglund, H., Lindstrom, P., Dhejne-Helmy, C. & Savic, I. Male-to-female transsexuals show sex-atypical hypothalamus activation when smelling odorous steroids. Cereb. Cortex 18, 1900–1908 (2008).
Burke, S. M., Cohen-Kettenis, P. T., Veltman, D. J., Klink, D. T. & Bakker, J. Hypothalamic response to the chemo-signal androstadienone in gender dysphoric children and adolescents. Front. Endocrinol. 5, 60 (2014).
Burke, S. M. et al. Male-typical visuospatial functioning in gynephilic girls with gender dysphoria - organizational and activational effects of testosterone. J. Psychiatry Neurosci. 41, 395–404 (2016).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5) 5th edn (American Psychiatric Association Publishing, 2013).
de Vries, A. L. et al. Young adult psychological outcome after puberty suppression and gender reassignment. Pediatrics 134, 696–704 (2014).
Turban, J. L., King, D., Carswell, J. M. & Keuroghlian, A. S. Pubertal suppression for transgender youth and risk of suicidal ideation. Pediatrics 145, e20191725 (2020).
Costa, R. et al. Psychological support, puberty suppression, and psychosocial functioning in adolescents with gender dysphoria. J. Sex. Med. 12, 2206–2214 (2015).
Becker, I. et al. A cross-sectional multicenter study of multidimensional body image in adolescents and adults with gender dysphoria before and after transition-related medical interventions. Arch. Sex. Behav. 47, 2335–2347 (2018).
Achille, C. et al. Longitudinal impact of gender-affirming endocrine intervention on the mental health and well-being of transgender youths: preliminary results. Int. J. Pediatr. Endocrinol. 2020, 8 (2020).
Kuper, L. E., Stewart, S., Preston, S., Lau, M. & Lopez, X. Body dissatisfaction and mental health outcomes of youth on gender-affirming hormone therapy. Pediatrics 145, e20193006 (2020).
Coleman, E. et al. Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. Int. J. Transgend. 13, 165–232 (2012).
Hembree, W. C. et al. Endocrine treatment of gender-dysphoric/gender-incongruent persons: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 102, 3869–3903 (2017).
Cohen-Kettenis, P. T. & van Goozen, S. H. Sex reassignment of adolescent transsexuals: a follow-up study. J. Am. Acad. Child. Adolesc. Psychiatry 36, 263–271 (1997).
Cohen-Kettenis, P. T. & van Goozen, S. H. Pubertal delay as an aid in diagnosis and treatment of a transsexual adolescent. Eur. Child. Adolesc. Psychiatry 7, 246–248 (1998).
Smith, Y. L., Van Goozen, S. H., Kuiper, A. J. & Cohen-Kettenis, P. T. Sex reassignment: outcomes and predictors of treatment for adolescent and adult transsexuals. Psychol. Med. 35, 89–99 (2005).
Cohen-Kettenis, P. T., Delemarre-van de Waal, H. A. & Gooren, L. J. The treatment of adolescent transsexuals: changing insights. J. Sex. Med. 5, 1892–1897 (2008).
de Vries, A. L., Steensma, T. D., Doreleijers, T. A. & Cohen-Kettenis, P. T. Puberty suppression in adolescents with gender identity disorder: a prospective follow-up study. J. Sex. Med. 8, 2276–2283 (2011).
Klink, D., Caris, M., Heijboer, A., van Trotsenburg, M. & Rotteveel, J. Bone mass in young adulthood following gonadotropin-releasing hormone analog treatment and cross-sex hormone treatment in adolescents with gender dysphoria. J. Clin. Endocrinol. Metab. 100, E270–E275 (2015).
Staphorsius, A. S. et al. Puberty suppression and executive functioning: An fMRI-study in adolescents with gender dysphoria. Psychoneuroendocrinology 56, 190–199 (2015).
Cohen-Kettenis, P. T., Schagen, S. E., Steensma, T. D., de Vries, A. L. & Delemarre-van de Waal, H. A. Puberty suppression in a gender-dysphoric adolescent: a 22-year follow-up. Arch. Sex. Behav. 40, 843–847 (2011).
Reardon, S. Largest ever study of transgender teenagers set to kick off. Nature 531, 560 (2016).
Olson-Kennedy, J. et al. Impact of early medical treatment for transgender youth: protocol for the longitudinal, observational trans youth care study. JMIR Res. Protoc. 8, e14434 (2019).
Tollit, M. A. et al. What are the health outcomes of trans and gender diverse young people in Australia? Study protocol for the Trans20 longitudinal cohort study. BMJ Open 9, e032151 (2019).
Richards, C. et al. Non-binary or genderqueer genders. Int. Rev. Psychiatry 28, 95–102 (2016).
Todd, K. et al. Demographic and behavioral profiles of nonbinary and binary transgender youth. Transgend Health 4, 254–261 (2019).
Twist, J. & de Graaf, N. M. Gender diversity and non-binary presentations in young people attending the United Kingdom’s National Gender Identity Development Service. Clin. Child. Psychol. Psychiatry 24, 277–290 (2019).
Chew, D. et al. Youths with a non-binary gender identity: a review of their sociodemographic and clinical profile. Lancet Child. Adolesc. Health 4, 322–330 (2020).
Cheung, A. S. et al. Non-binary and binary gender identity in australian trans and gender diverse individuals. Arch. Sex. Behav. 49, 2673–2681 (2020).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-4) 4th edn (American Psychiatric Association Publishing, 1994).
World Health Organization. WHO/Europe brief — Transgender Health in the Context of ICD-11. WHO https://www.euro.who.int/en/health-topics/health-determinants/gender/gender-definitions/whoeurope-brief-transgender-health-in-the-context-of-icd-11 (2021).
Bakker, A., van Kesteren, P. J., Gooren, L. J. & Bezemer, P. D. The prevalence of transsexualism in The Netherlands. Acta Psychiatr. Scand. 87, 237–238 (1993).
Herman, J. L., Flores, A. R., Brown, T. N. T., Wilson, B. D. M. & Conron, K. J. Age of Individuals Who Identify as Transgender in the United States (UCLA School of Law Williams Institute, 2017).
Rider, G. N., McMorris, B. J., Gower, A. L., Coleman, E. & Eisenberg, M. E. Health and care utilization of transgender and gender nonconforming youth: a population-based study. Pediatrics 141, e20171683 (2018).
Johns, M. M. et al. Transgender identity and experiences of violence victimization, substance use, suicide risk, and sexual risk behaviors among high school students - 19 states and large urban school districts, 2017. MMWR 68, 67–71 (2019).
Winter, S. et al. Transgender people: health at the margins of society. Lancet 388, 390–400 (2016).
Aitken, M. et al. Evidence for an altered sex ratio in clinic-referred adolescents with gender dysphoria. J. Sex. Med. 12, 756–763 (2015).
Chiniara, L. N., Bonifacio, H. J. & Palmert, M. R. Characteristics of adolescents referred to a gender clinic: are youth seen now different from those in initial reports? Horm. Res. Paediatr. 89, 434–441 (2018).
Fausto-Sterling, A. The dynamic development of gender variability. J. Homosex. 59, 398–421 (2012).
Martin, C. L., Ruble, D. N. & Szkrybalo, J. Cognitive theories of early gender development. Psychol. Bull. 128, 903–933 (2002).
Heylens, G. et al. Gender identity disorder in twins: a review of the case report literature. J. Sex. Med. 9, 751–757 (2012).
Henningsson, S. et al. Sex steroid-related genes and male-to-female transsexualism. Psychoneuroendocrinology 30, 657–664 (2005).
Ujike, H. et al. Association study of gender identity disorder and sex hormone-related genes. Prog. Neuropsychopharmacol. Biol. Psychiatry 33, 1241–1244 (2009).
Bentz, E. K. et al. A polymorphism of the CYP17 gene related to sex steroid metabolism is associated with female-to-male but not male-to-female transsexualism. Fertil. Steril. 90, 56–59 (2008).
White, P. C. Letter to the editor: “Genetic link between gender dysphoria and sex hormone signaling”. J. Clin. Endocrinol. Metab. 104, 4418–4419 (2019).
Foreman, M., Vilain, E. & Harley, V. Response to Letter to the Editor: “Genetic link between gender dysphoria and sex hormone signaling”. J. Clin. Endocrinol. Metab. 104, 4420 (2019).
Fernandez, R. et al. Analysis of four polymorphisms located at the promoter of the estrogen receptor alpha ESR1 gene in a population with gender incongruence. Sex. Med. 8, 490–500 (2020).
Gooren, L. The biology of human psychosexual differentiation. Horm. Behav. 50, 589–601 (2006).
Kreukels, B. P. C. et al. Gender dysphoria and gender change in disorders of sex development/intersex conditions: results from the dsd-LIFE study. J. Sex. Med. 15, 777–785 (2018).
Frisen, L. et al. Gender role behavior, sexuality, and psychosocial adaptation in women with congenital adrenal hyperplasia due to CYP21A2 deficiency. J. Clin. Endocrinol. Metab. 94, 3432–3439 (2009).
Meyer-Bahlburg, H. F., Dolezal, C., Baker, S. W. & New, M. I. Sexual orientation in women with classical or non-classical congenital adrenal hyperplasia as a function of degree of prenatal androgen excess. Arch. Sex. Behav. 37, 85–99 (2008).
Cohen-Kettenis, P. T. Gender change in 46,XY persons with 5α-reductase-2 deficiency and 17β-hydroxysteroid dehydrogenase-3 deficiency. Arch. Sex. Behav. 34, 399–410 2005).
Imperato-McGinley, J., Peterson, R. E., Gautier, T. & Sturla, E. Androgens and the evolution of male-gender identity among male pseudohermaphrodites with 5α-reductase deficiency. N. Engl. J. Med. 300, 1233–1237 (1979).
Rosler, A., Silverstein, S. & Abeliovich, D. A (R80Q) mutation in 17 beta-hydroxysteroid dehydrogenase type 3 gene among Arabs of Israel is associated with pseudohermaphroditism in males and normal asymptomatic females. J. Clin. Endocrinol. Metab. 81, 1827–1831 (1996).
Reiner, W. G. & Gearhart, J. P. Discordant sexual identity in some genetic males with cloacal exstrophy assigned to female sex at birth. N. Engl. J. Med. 350, 333–341 (2004).
Meyer-Bahlburg, H. F. Gender identity outcome in female-raised 46,XY persons with penile agenesis, cloacal exstrophy of the bladder, or penile ablation. Arch. Sex. Behav. 34, 423–438 (2005).
T’Sjoen, G. et al. Male gender identity in complete androgen insensitivity syndrome. Arch. Sex. Behav. 40, 635–638 (2011).
Burke, S. M., Menks, W. M., Cohen-Kettenis, P. T., Klink, D. T. & Bakker, J. Click-evoked otoacoustic emissions in children and adolescents with gender identity disorder. Arch. Sex. Behav. 43, 1515–1523 (2014).
Reisner, S. L. et al. Mental health of transgender youth in care at an adolescent urban community health center: a matched retrospective cohort study. J. Adolesc. Health 56, 274–279 (2015).
Kuper, L. E., Mathews, S. & Lau, M. Baseline mental health and psychosocial functioning of transgender adolescents seeking gender-affirming hormone therapy. J. Dev. Behav. Pediatr. 40, 589–596 (2019).
de Vries, A. L. & Cohen-Kettenis, P. T. Clinical management of gender dysphoria in children and adolescents: the Dutch approach. J. Homosex. 59, 301–320 (2012).
Spack, N. P. et al. Children and adolescents with gender identity disorder referred to a pediatric medical center. Pediatrics 129, 418–425 (2012).
Olson, J., Schrager, S. M., Belzer, M., Simons, L. K. & Clark, L. F. Baseline physiologic and psychosocial characteristics of transgender youth seeking care for gender dysphoria. J. Adolesc. Health 57, 374–380 (2015).
Davey, A., Arcelus, J., Meyer, C. & Bouman, W. P. Self-injury among trans individuals and matched controls: prevalence and associated factors. Health Soc. Care Community 24, 485–494 (2016).
Veale, J. F., Watson, R. J., Peter, T. & Saewyc, E. M. Mental health disparities among Canadian transgender youth. J. Adolesc. Health 60, 44–49 (2017).
Sorbara, J. C., Chiniara, L. N., Thompson, S. & Palmert, M. R. Mental health and timing of gender-affirming care. Pediatrics 146, e20193600 (2020).
Chen, D. et al. Psychosocial characteristics of transgender youth seeking gender-affirming medical treatment: baseline findings from the Trans Youth Care Study. J. Adolesc. Health 68, 1104–1111 (2021).
Travers, R. et al. Impacts of strong parental support for trans youth: a report prepared for Children’s Aid Society of Toronto and Delisle Youth Services. TransPULSE https://transpulseproject.ca/research/impacts-of-strong-parental-support-for-trans-youth/ (2012).
de Vries, A. L., Noens, I. L., Cohen-Kettenis, P. T., van Berckelaer-Onnes, I. A. & Doreleijers, T. A. Autism spectrum disorders in gender dysphoric children and adolescents. J. Autism Dev. Disord. 40, 930–936 (2010).
Strang, J. F. et al. Increased gender variance in autism spectrum disorders and attention deficit hyperactivity disorder. Arch. Sex. Behav. 43, 1525–1533 (2014).
Shumer, D. E., Reisner, S. L., Edwards-Leeper, L. & Tishelman, A. Evaluation of asperger syndrome in youth presenting to a gender dysphoria clinic. LGBT Health 3, 387–390 (2016).
Strang, J. F. et al. Initial clinical guidelines for co-occurring autism spectrum disorder and gender dysphoria or incongruence in adolescents. J. Clin. Child. Adolesc. Psychol. 47, 105–115 (2018).
Nabbijohn, A. N. et al. Gender variance and the autism spectrum: an examination of children ages 6-12 years. J. Autism Dev. Disord. 49, 1570–1585 (2019).
Neyman, A., Fuqua, J. S. & Eugster, E. A. Bicalutamide as an androgen blocker with secondary effect of promoting feminization in male-to-female transgender adolescents. J. Adolesc. Health 64, 544–546 (2019).
O’Bryant, C. L., Flaig, T. W. & Utz, K. J. Bicalutamide-associated fulminant hepatotoxicity. Pharmacotherapy 28, 1071–1075 (2008).
T’Sjoen, G., Arcelus, J., Gooren, L., Klink, D. T. & Tangpricha, V. Endocrinology of transgender medicine. Endocr. Rev. 40, 97–117 (2019).
Jockenhovel, F. et al. Pharmacokinetics and pharmacodynamics of subcutaneous testosterone implants in hypogonadal men. Clin. Endocrinol. 45, 61–71 (1996).
Brik, T., Vrouenraets, L., de Vries, M. C. & Hannema, S. E. Trajectories of adolescents treated with gonadotropin-releasing hormone analogues for gender dysphoria. Arch. Sex. Behav. 49, 2611–2618 (2020).
Turban, J. L., Carswell, J. & Keuroghlian, A. S. Understanding pediatric patients who discontinue gender-affirming hormonal interventions. JAMA Pediatr. 172, 903–904 (2018).
Wiepjes, C. M. et al. The Amsterdam Cohort of Gender Dysphoria study (1972-2015): trends in prevalence, treatment, and regrets. J. Sex. Med. 15, 582–590 (2018).
Vlot, M. C. et al. Effect of pubertal suppression and cross-sex hormone therapy on bone turnover markers and bone mineral apparent density (BMAD) in transgender adolescents. Bone 95, 11–19 (2017).
Stoffers, I. E., de Vries, M. C. & Hannema, S. E. Physical changes, laboratory parameters, and bone mineral density during testosterone treatment in adolescents with gender dysphoria. J. Sex. Med. 16, 1459–1468 (2019).
Joseph, T., Ting, J. & Butler, G. The effect of GnRH analogue treatment on bone mineral density in young adolescents with gender dysphoria: findings from a large national cohort. J. Pediatr. Endocrinol. Metab. 32, 1077–1081 (2019).
Zemel, B. S. et al. Revised reference curves for bone mineral content and areal bone mineral density according to age and sex for black and non-black children: results of the bone mineral density in childhood study. J. Clin. Endocrinol. Metab. 96, 3160–3169 (2011).
Lee, J. Y. Low bone mineral density in early pubertal transgender/gender diverse youth: findings from the Trans Youth Care Study. J. Endocr. Soc. 4, bvaa065 (2020).
Schagen, S. E. E., Wouters, F. M., Cohen-Kettenis, P. T., Gooren, L. J. & Hannema, S. E. Bone development in transgender adolescents treated with GnRH analogues and subsequent gender-affirming hormones. J. Clin. Endocrinol. Metab. 105, e4252–e4263 (2020).
Finlayson, C. et al. Proceedings of the working group session on fertility preservation for individuals with gender and sex diversity. Transgend Health 1, 99–107 (2016).
Johnson, E. K. et al. Fertility preservation for pediatric patients: current state and future possibilities. J. Urol. 198, 186–194 (2017).
Lai, T. C., McDougall, R., Feldman, D., Elder, C. V. & Pang, K. C. Fertility counseling for transgender adolescents: a review. J. Adolesc. Health 66, 658–665 (2020).
Rothenberg, S. S., Witchel, S. F. & Menke, M. N. Oocyte cryopreservation in a transgender male adolescent. N. Engl. J. Med. 380, 886–887 (2019).
Chen, D., Simons, L., Johnson, E. K., Lockart, B. A. & Finlayson, C. Fertility preservation for transgender adolescents. J. Adolesc. Health 61, 120–123 (2017).
Nahata, L., Tishelman, A. C., Caltabellotta, N. M. & Quinn, G. P. Low fertility preservation utilization among transgender youth. J. Adolesc. Health 61, 40–44 (2017).
Chiniara, L. N., Viner, C., Palmert, M. & Bonifacio, H. Perspectives on fertility preservation and parenthood among transgender youth and their parents. Arch. Dis. Child. 104, 739–744 (2019).
Brik, T. et al. Use of fertility preservation among a cohort of transgirls in the Netherlands. J. Adolesc. Health 64, 589–593 (2019).
Pang, K. C. et al. Rates of fertility preservation use among transgender adolescents. JAMA Pediatr. 174, 890–891 (2020).
Schneider, M. A. et al. Brain maturation, cognition and voice pattern in a gender dysphoria case under pubertal suppression. Front. Hum. Neurosci. 11, 528 (2017).
Schagen, S. E., Cohen-Kettenis, P. T., Delemarre-van de Waal, H. A. & Hannema, S. E. Efficacy and safety of gonadotropin-releasing hormone agonist treatment to suppress puberty in gender dysphoric adolescents. J. Sex. Med. 13, 1125–1132 (2016).
Khatchadourian, K., Amed, S. & Metzger, D. L. Clinical management of youth with gender dysphoria in Vancouver. J. Pediatr. 164, 906–911 (2014).
Nokoff, N. J. et al. Body composition and markers of cardiometabolic health in transgender youth compared with cisgender youth. J. Clin. Endocrinol. Metab. 105, e704–e714 (2020).
Klaver, M. et al. Hormonal treatment and cardiovascular risk profile in transgender adolescents. Pediatrics 145, e20190741 (2020).
Millington, K. et al. Physiological and metabolic characteristics of a cohort of transgender and gender-diverse youth in the united states. J. Adolesc. Health 67, 376–383 (2020).
Millington, K. et al. Association of high-density lipoprotein cholesterol with sex steroid treatment in transgender and gender-diverse youth. JAMA Pediatr. 175, 520–521 (2021).
Jarin, J. et al. Cross-sex hormones and metabolic parameters in adolescents with gender dysphoria. Pediatrics 139, e20193653 (2017).
Hannema, S. E., Schagen, S. E. E., Cohen-Kettenis, P. T. & Delemarre-van de Waal, H. A. Efficacy and safety of pubertal induction using 17β-estradiol in transgirls. J. Clin. Endocrinol. Metab. 102, 2356–2363 (2017).
Olson-Kennedy, J., Okonta, V., Clark, L. F. & Belzer, M. Physiologic response to gender-affirming hormones among transgender youth. J. Adolesc. Health 62, 397–401 (2018).
Vance, S. R. Jr., Halpern-Felsher, B. L. & Rosenthal, S. M. Health care providers’ comfort with and barriers to care of transgender youth. J. Adolesc. Health 56, 251–253 (2015).
van de Grift, T. C. et al. Timing of puberty suppression and surgical options for transgender youth. Pediatrics 146, (2020).
Ault, A. Docs spurn attempts to criminalize treatment of transgender kids. Medscape https://www.medscape.com/viewarticle/925608 (2020).
Walch, A. et al. Proper care of transgender and gender diverse persons in the setting of proposed discrimination: a policy perspective. J. Clin. Endocrinol. Metab. 106, 305–308 (2021).
Dyer, C. Puberty blockers: children under 16 should not be referred without court order, says NHS England. BMJ 371, m4717 (2020).
WPATH, EPATH, USPATH, AsiaPATH, CPATH, AusPATH, PATHA. Response to Bell v. Tavistock Judgment. Statement regarding medical affirming treatment including puberty blockers for transgender adolescents. WPATH https://www.wpath.org/media/cms/Documents/Public%20Policies/2020/FINAL%20Statement%20Regarding%20Informed%20Consent%20Court%20Case_Dec%2016%202020.docx.pdf?_t=1608225376 (2020).
Topping, A. High court grants leave to appeal to UK gender identity service. The Guardian https://www.theguardian.com/world/2021/jan/19/high-court-grants-leave-to-appeal-to-uk-gender-identity-service (2021).
Drescher, J. & Byne, W. Gender dysphoric/gender variant (GD/GV) children and adolescents: summarizing what we know and what we have yet to learn. J. Homosex. 59, 501–510 (2012).
Littman, L. Parent reports of adolescents and young adults perceived to show signs of a rapid onset of gender dysphoria. PLoS ONE 13, e0202330 (2018).
Wadman, M. ‘Rapid onset’ of transgender identity ignites storm. Science 361, 958–959 (2018).
Littman, L. Correction: Parent reports of adolescents and young adults perceived to show signs of a rapid onset of gender dysphoria. PLoS ONE 14, e0214157 (2019).
Acknowledgements
The author is grateful to and inspired by his patients, their families and his colleagues, from whom he has learned so much. He is also grateful to the National Institutes of Health/Eunice Kennedy Shriver National Institute of Child Health and Human Development for their support of our research on “The Impact of Early Medical Treatment in Transgender Youth” (R01HD082554).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author declares no competing interests.
Additional information
Peer review information
Nature Reviews Endocrinology thanks J. Carswell and X. Lopez for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rosenthal, S.M. Challenges in the care of transgender and gender-diverse youth: an endocrinologist’s view. Nat Rev Endocrinol 17, 581–591 (2021). https://doi.org/10.1038/s41574-021-00535-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41574-021-00535-9
This article is cited by
-
Puberty Suppression for Pediatric Gender Dysphoria and the Child’s Right to an Open Future
Archives of Sexual Behavior (2024)
-
Transition Regret and Detransition: Meanings and Uncertainties
Archives of Sexual Behavior (2023)
-
Current Concerns About Gender-Affirming Therapy in Adolescents
Current Sexual Health Reports (2023)
-
The Detransition Rate Is Unknown
Archives of Sexual Behavior (2023)
-
Gender-Affirming Treatment of Gender Dysphoria in Youth: A Perfect Storm Environment for the Placebo Effect—The Implications for Research and Clinical Practice
Archives of Sexual Behavior (2023)