Abstract
Aims/hypothesis
We aimed to evaluate whether genetically predicted HbA1c has an effect on the risk of cardiovascular diseases and investigate the shape of the relationship of genetically predicted HbA1c with cardiovascular diseases.
Methods
We performed linear univariable, multivariable and non-linear Mendelian randomisation analyses in 373,571 white British participants (mean age 56.9) from the UK Biobank.
Results
In univariable linear Mendelian randomisation analysis, a 1 mmol/mol increase in genetically predicted HbA1c was associated with higher risk of coronary artery disease (OR 1.03, 95% CI 1.02, 1.05), stroke (OR 1.02, 95% CI 1.00, 1.05) and hypertension (OR 1.02, 95% CI 1.01, 1.03). Multivariable Mendelian randomisation adjusted for the effect of haemoglobin gave a consistent conclusion for coronary artery disease. The associations with stroke and hypertension were directionally similar but with wider CI overlapping the null. Non-linear Mendelian randomisation indicated that the shape of the effect of genetically predicted HbA1c on cardiovascular outcomes was likely linear.
Conclusions/interpretation
The study suggests a detrimental effect of HbA1c on coronary artery disease in both men and women, and the effect is via a glycaemic characteristic. The shape of the genetic association of HbA1c with these cardiovascular outcomes, in particular coronary artery disease, is likely to be linear.
Graphical abstract

Similar content being viewed by others

Introduction
HbA1c, a biomarker indicating the past 3 months average blood glucose level, is routinely used in the diagnosis of type 2 diabetes [1]. Previous observational studies have suggested a positive association of HbA1c with cardiovascular disease (CVD) [2]. However, it is unclear whether these associations are linear. The Emerging Risk Factors Collaboration study suggested a J-shaped association of HbA1c with incident CVD [3], whilst another study suggests a threshold relationship of HbA1c (≥53 mmol/mol, 7.0%) with stroke [4]. Although a non-linear relationship of risk factors with cardiovascular outcomes is not impossible, such as for BMI [5], the presence of such a relationship could also be an indication of confounding or selection bias [6]. Better understanding of the shape of the relationship of HbA1c with cardiovascular outcomes may help determine whether the current recommendations about the HbA1c diagnostic threshold are appropriate for preventing cardiovascular complications [7].
Mendelian randomisation studies are more robust to confounding than conventional observational studies due to the use of genetic variants randomly allocated at conception [8]. Mendelian randomisation studies have increasingly been used to ascertain the causal role of HbA1c in CVD and related outcomes where they show HbA1c as causal in the development of coronary artery disease (CAD) [9,10,11] and hypertension [12]. Apart from the glycaemic property of HbA1c, a recent study suggested alternative, non-glycaemic pathways by which HbA1c conferred CAD risk, such as haemoglobin (Hgb) [11]. However, this study did not disentangle the effect of HbA1c independent of Hgb using multivariable Mendelian randomisation (MVMR) [11]. Non-linear Mendelian randomisation may shed light on the appropriateness of the current HbA1c guidelines, although relevant studies are scarce, and the only study is limited to CAD [13]. To further assess the effect of HbA1c on CVD, taking into account pleiotropic effects due to the erythrocytic properties of HbA1c, and potential non-linearity, we performed linear Mendelian randomisation allowing for Hgb using MVMR, and non-linear Mendelian randomisation in the UK Biobank. We also assessed sex-specific, genetically predicted effects of HbA1c in CVD, as differences by sex have previously been observed [14].
Methods
Assumptions of Mendelian randomisation
Mendelian randomisation relies on the three instrumental variable assumptions for valid causal inference [15]. First, the genetic instruments should be associated with the exposure, here HbA1c. Second, the genetic instruments should not be confounded by factors affecting the exposure-outcome relationship. Lastly, the genetic instruments should only affect the outcome via affecting the exposure (HbA1c), i.e. the exclusion restriction assumption (electronic supplementary material [ESM] Fig. 1).
UK Biobank
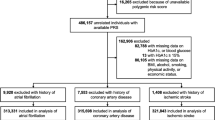
The UK Biobank recruited around 500,000 participants (aged 37–73) from 2006 to 2010 across 22 assessment centres in England, Scotland and Wales. Participants completed a series of physical assessments and questionnaires, such as socio-demographic, lifestyle and self-reported health conditions [16]. Participants also provided biological samples at baseline for biochemical assays and genotyping. Disease status and vital statistics are regularly updated via record linkage to national medical and mortality records, as described elsewhere [16]. HbA1c was measured in mmol/mol using HPLC (Bio-Rad Variant II Turbo analysers, Bio-Rad Laboratories, USA) and was converted to percentage using the equation (0.09148 × HbA1c in mmol/mol) + 2.152 [17]. Genotyping was performed using the Affymetrix UK BiLEVE Axiom array (USA) and Affymetrix UK Biobank Axiom array and imputation using a reference panel combining the UK10K haplotype and the Haplotype Reference Consortium panels [16]. To reduce confounding by population stratification, the analyses were restricted to participants who were of both self-reported and genetically verified white British ancestry. We also excluded participants who were extensively related (more than ten putative third-degree relatives in the kinship table), who had poor quality genotyping (i.e. missing rate ≥1.5%), who had sex chromosome aneuploidy, whose self-reported and genetic sex did not match, who had withdrawn (August 2020 update) or who were without data on HbA1c or genetic variants for HbA1c.
Outcomes
The primary outcomes were CAD, stroke and hypertension. The secondary outcomes were ischaemic stroke, haemorrhagic stroke, atrial fibrillation, heart failure and thromboembolism. Each outcome was defined based on self-reported health conditions and medication at baseline, and subsequent hospital admissions (primary and secondary diagnoses, ICD-9 and ICD-10 codes) or death registration (primary and contributory causes of death, ICD-10 codes) based on the December 2020 updates. As a sensitivity analysis, we also defined hypertension additionally based on BP measurement at baseline (systolic BP [SBP] ≥130 mmHg or diastolic BP [DBP] ≥80 mmHg according to the 2017 American College of Cardiology/American Heart Association guideline), as per our previous study [12]. Detailed information on the outcome definitions is described in ESM Table 1.
Genetic instruments of HbA1c
We selected all genetic variants which reached genome-wide significance (p < 5 × 10−8) as instrumental variables for HbA1c from an independent genome-wide association study (GWAS) of 123,665 participants of European ancestry (no overlap with the UK Biobank) [18]. The original GWAS investigator included participants without diabetes, as defined by clinical diagnosis, glucose-lowering medication use, or blood glucose measurement (HbA1c ≥47 mmol/mol [6.5%], or fasting glucose ≥7 mmol/l, or 2 h glucose ≥11.1 mmol/l) [18]. Of these 43 variants, 35 were uncorrelated (r2 < 0.001 within a 10,000 kb window) based on European descent participants from Phase 3 (Version 5) of the 1000 Genomes Project [19]. We excluded a variant on ABO (a well-known pleiotropic loci) [20] and a variant violating Hardy–Weinberg equilibrium (identified in our previous study) [10].
Genetic risk score of HbA1c
For each participant in the UK Biobank, we constructed an externally weighted genetic risk score (GRS) for HbA1c by summing the number of HbA1c increasing alleles each participant inherited at each variant, weighted by the variant-HbA1c coefficient effect derived from an independent study [18]. Provided that the variants are all valid, the use of externally weighted GRS improves statistical power [21]. The strength of the instrument was assessed from the F-statistic obtained from linear regression. Preliminary analyses suggested a significant association of the GRS derived from these 33 variants with BMI (p = 3 × 10−4) in the UK Biobank. As such, we additionally excluded four variants associated with BMI (p < 5.3 × 10−5) and hence 29 variants remained in the subsequent analyses. All these variants were related to HbA1c in the UK Biobank (p ranging from 5.4 × 10−4 to 8.9 × 10−287) as shown in ESM Table 2. Associations of the GRS with potential confounders were assessed using χ2 tests and linear regression.
Univariable Mendelian randomisation
Univariable Mendelian randomisation (UVMR) using the GRS was used to estimate the effect of genetically predicted HbA1c on each cardiovascular outcome using the Wald estimate, i.e. association of GRS with each cardiovascular outcome divided by the association of the GRS with HbA1c. We adjusted for sex (if relevant), age at baseline, genotyping array and the top 20 principal components of ancestry for genetic associations with both exposure and outcomes. We assessed differences by sex by comparing sex-specific estimates using a Z test [22]. To assess the robustness of the findings, we also performed sensitivity analyses using methods with different assumptions about horizontal pleiotropy, i.e. inverse-variance weighted (IVW) with a multiplicative random effects model [23], Mendelian randomisation-Egger (MR-Egger) [24] and the weighted median [25]. Whilst IVW assumes all variants are valid or there is balanced pleiotropy, the use of multiplicative random effects down-weights the effect of outlying variants (likely to be invalid variants) [23]. MR-Egger is an extension of IVW, where all variants are allowed to have pleiotropic effects assuming the instrument strength is independent of the direct effect (InSIDE assumption), however, the MR-Egger estimate is of low statistical power [24]. The MR-Egger intercept with p value <0.05 indicates the presence of overall horizontal pleiotropy (i.e. an invalid IVW estimate) [24]. We assessed the I2 (0 to 1) of the variant-exposure associations to indicate the instrument strength of MR-Egger. An I2 close to 1 suggests the MR-Egger estimate is unlikely to be biased by violation of the no measurement error assumption [26]. The weighted median measures the central tendency of these variant-specific estimates, assuming valid variants contribute at least half of the weight [25]. Apart from these analyses, we used Cochran’s Q statistic to assess heterogeneity of the Wald estimates across variants where high heterogeneity indicates the presence of invalid variants [27].
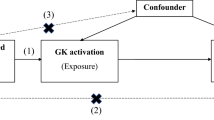
MVMR
MVMR was used to correct for possible horizontal pleiotropy due to Hgb, a key factor which correlates with HbA1c. Although MVMR is increasingly used to control for horizontal pleiotropy and can complement other analyses [28], MVMR is generally of lower statistical power compared with UVMR. We obtained genome-wide significant (p ≤ 5 × 10−8) and uncorrelated (r2 < 0.001) variants that associated with Hgb from the largest haematological GWAS conducted in 408,112 participants of European ancestry [29]. After exclusion of 15 variants associated with potential confounders, we obtained 141 uncorrelated variants that predicted either HbA1c or Hgb (ESM Table 3). Using these variants, we performed multivariable IVW and multivariable MR-Egger to obtain the independent causal effects of HbA1c on the cardiovascular outcomes [30]. We calculated the conditional F-statistics for exposures (HbA1c and Hgb) using the phenotypic correlation matrix from UK Biobank data. A larger conditional F-statistic (the rule-of-thumb of ten) indicates a lower risk of weak instrument bias [31].
Non-linear Mendelian randomisation
To obtain non-linear Mendelian randomisation estimates, fractional polynomials were used [32, 33]. We set the reference to an HbA1c of 39 mmol/mol (5.7%), the reference used to define individuals with prediabetes [34]. We estimated the localised average causal effect (LACE) based on the centiles of the instrumental variable-free exposure [32]. We visualised the best fitting using the derivative of the fractional polynomial models of degree 2 [33]. From this analysis, we reported (1) the p value for a trend test based on meta-regression which assessed whether a non-linear trend exists; and (2) the p value for a fractional polynomial non-linearity test which assessed whether a non-linear model fits across the LACE estimates in each stratum better than a linear model [33].
All statistical analyses were performed using R version 4.0.2 (R Development Core Team, Vienna, Austria). UVMR analyses were performed using TwoSampleMR package (v 0.5.5), MVMR analyses were performed using MendelianRandomization (0.5.0) and MVMR (0.2) packages. Non-linear Mendelian randomisation analyses were performed using nlmr package, available at https://github.com/jrs95/nlmr. The results were visualised using forestplot package (v1.10).
Ethics approval
The UK Biobank received ethics approval from the North West Multi-centre Research Ethics Committee (11/NW/0382), and all participants provided written informed consent before participation [16].
Results
Baseline characteristics
Of the 487,320 eligible UK Biobank participants, 373,571 white British remained after exclusions. Table 1 shows the baseline characteristics of the participants by sex. Of these, 36,752 had CAD (9.8%), 10,441 had stroke (2.8%) and 130,658 had hypertension (35%), with higher prevalence in men than women for these cardiovascular outcomes. The GRS was strongly associated with HbA1c overall and by sex where the GRS explained 1.4–1.7% of the variance of HbA1c. The GRS was not associated with any socioeconomic or lifestyle factors (ESM Table 4).
UVMR analyses of HbA1c on CAD, stroke and hypertension
In UVMR with an externally weighted GRS, genetically predicted higher HbA1c was associated with higher risk of CAD (OR 1.03 per mmol/mol increase in HbA1c, 95% CI 1.02, 1.05), stroke (OR 1.02, 95% CI 1.00, 1.05) and hypertension (OR 1.02, 95% CI 1.01, 1.03) (Fig. 1a). Sex-stratified analyses gave similar results (Fig. 1b, c). Repeating the analyses with a definition of hypertension including SBP and DBP measurement at baseline did not change the interpretation (ESM Table 5). I2GX of 0.94 indicated the MR-Egger estimates were unlikely biased by violation of no measurement error assumption. The Cochran’s Q suggested possible heterogeneity, but the MR-Egger intercept did not indicate possible horizontal pleiotropy (ESM Table 5).
MVMR analyses of HbA1c on CAD, stroke and hypertension
In MVMR, the conditional F-statistic for HbA1c was 8.6 and for Hgb was 47.2. After adjusting for the effect of Hgb, the direct effect of HbA1c was associated with higher risk of CAD overall (OR 1.08 per mmol/mol, 95% CI 1.04, 1.11), in men (OR 1.08, 95% CI 1.04, 1.12) and in women (OR 1.07, 95% CI 1.02, 1.11), whilst the direction for stroke and hypertension remained positive but with wide CI (Fig. 1). The multivariable MR-Egger method provided consistent results and did not suggest horizontal pleiotropy. Genetically predicted Hgb appeared associated with higher risk of CAD and hypertension in men only (ESM Table 6).
Non-linear Mendelian randomisation analyses of HbA1c on CAD, stroke and hypertension
In non-linear Mendelian randomisation, there was no evidence of non-linearity for the associations of genetically predicted HbA1c with CAD, stroke or hypertension (Fig. 2 and ESM Table 7). However, genetically predicted HbA1c appeared to have a J-shaped relationship with the risk of hypertension (p value of trend test = 0.07, Fig. 2c, ESM Table 7).
The effect of genetically predicted HbA1c (mmol/mol) on the risk of (a) CAD, (b) overall stroke and (c) hypertension in participants from the UK Biobank using non-linear Mendelian randomisation. The x-axis depicts HbA1c levels in mmol/mol. The y-axis depicts the OR, with respect to the reference, plotted on a natural logarithm scale. The reference is set to an HbA1c of 39 mmol/mol (5.7%), the reference used to define individuals with prediabetes. The black line represents the dose–response curve. The grey lines represent the 95% CI
Mendelian randomisation analyses of HbA1c on stroke subtypes, atrial fibrillation, heart failure and thromboembolism
In UVMR with an externally weighted GRS, we found genetically predicted HbA1c was associated with higher risk of heart failure (OR 1.04, 95% CI 1.01, 1.07) in men but not for the other secondary cardiovascular outcomes, i.e. stroke subtypes, atrial fibrillation and thromboembolism (ESM Fig. 2, ESM Table 5). Similar conclusions were observed based on MVMR analyses (ESM Fig. 2, ESM Table 6). Non-linear Mendelian randomisation analyses showed that participants with higher HbA1c appeared to have higher risk of these secondary outcomes in a linear manner (ESM Fig. 3).
Discussion
To the best of our knowledge, this is one of the first Mendelian randomisation studies comprehensively examining the sex-specific effect of genetically predicted HbA1c on cardiovascular outcomes whilst allowing for Hgb, as well as assessing potential non-linearity. Using an externally weighted GRS, which improves statistical power, and the most up to date data from the UK Biobank, we confirmed previous studies that provided evidence that genetically predicted HbA1c increased the risk of CAD, stroke and hypertension [9,10,11,12]. Our study builds on this by showing these associations are likely due to the glycaemic property of HbA1c, and there is no strong evidence for a sex difference despite including more participants than our previous study [10]. Lastly, there was no strong evidence for non-linearity regarding the genetic association of genetically predicted HbA1c with major CVD.
HbA1c impacts CAD, and our study shows that the relationship is likely to be linear, consistent with previous observational studies [35]. Higher HbA1c indicates hyperglycaemia and hence could impact arterial wall structure and subsequent risk of atherosclerosis [36]. Previous Mendelian randomisation studies suggest HbA1c may increase LDL-cholesterol (LDL-C) [11] and risk of hypertension [12], which may mediate the HbA1c-CAD relationship. Our finding also aligns with recent Mendelian randomisation findings that there were linear relationships of both SBP and DBP with CAD risk [37], as well as positive associations of type 2 diabetes with CAD risk in both sexes [14]. Our study found a lack of non-linearity concerning HbA1c on CAD, similar to a recent Mendelian randomisation study, although this study used a different approach for instrument selection, was restricted to participants without diabetes, and only considered incident CAD [13].
A previous Mendelian randomisation study also showed a positive relationship between HbA1c and CAD risk despite being restricted to instruments only associated with erythrocyte indices, not glycaemic traits [11], although selective exclusion of a large number of instruments may introduce bias and reduce statistical power. Our findings from MVMR suggest the positive association of HbA1c with CAD is not driven by the erythrocytic properties of HbA1c and thus confirm the aetiologic role of blood glucose in CAD. Although there were some changes in the estimates for HbA1c after adjusting for Hgb in the MVMR analyses (Fig. 1), this could be driven by weak instrument bias due to the low conditional F-statistics for HbA1c. Alternatively, Hgb may not comprehensively capture the relevant erythrocyte phenotype, which could be a specific aspect of iron metabolism.
Consistent with a recent Mendelian randomisation study using MEGASTROKE data [38], we found suggestive evidence in the UK Biobank that HbA1c increases the risk of stroke [10]. Our study is also consistent with previous observational studies showing a positive relation between HbA1c and hypertension [39]. Possible mechanisms may include insulin resistance, beta cell dysfunction [38], increased oxidative stress and inflammatory mechanisms mediated by interleukins [40].
The relationship between genetically elevated HbA1c with the secondary outcomes were less clear, with relatively wide 95% CI due to lower case numbers (ESM Fig. 2), although we found evidence of a detrimental impact on heart failure among men. Some previous observational studies suggested that higher HbA1c is associated with higher risk of atrial fibrillation [41] and heart failure [42], although a Mendelian randomisation study did not provide strong evidence for an effect of HbA1c in atrial fibrillation [43]. Given these diseases usually manifest in later life, we could not rule out the possibility of these specific null findings being driven by selection bias, due to inevitably selecting survivors of both higher HbA1c and any competing risk of earlier onset CVD, which can negate or reverse estimates [44]. Whether HbA1c also plays an aetiologic role in these other cardiovascular outcomes should be evaluated in alternative designs, which are less open to selection bias from selecting survivors, such as randomised controlled trials.
The study has several limitations. First, although we used MVMR to obtain the effect of HbA1c in cardiovascular outcomes controlling for Hgb, MVMR generally gave wider 95% CI. A conditional F-statistic for HbA1c of 8.6 may also indicate risk of a weak instrument, which may explain the larger estimates in MVMR compared with UVMR, although with overlapping CI [45]. However, a recent Mendelian randomisation study that excluded variants of HbA1c associated with erythrocytes also supports the hypothesis that the detrimental effects of genetically predicted HbA1c on cardiovascular risk is via glycaemic properties, suggesting our study should be valid [38]. Second, our study assessed the shape of genetically predicted HbA1c on cardiovascular outcomes using fractional polynomials, which enables division of the population into stratums [33]. A proper stratification is crucial for smoothing LACE estimates to properly characterise the overall shape of potential causal association because higher heterogeneity of the LACE at the end of spectrum may distort the overall shape [33]. We cross-checked the results by using different stratum numbers (e.g. n = 50) and the overall shape of the relationship remained similar. Third, we used the genetic predictors of HbA1c in sex-combined GWAS and applied them to derive sex-specific genetic association with each outcome. However, the study is unlikely to be affected as there is high concordance of each genetic association with HbA1c across sexes (r = 0.99) in the UK Biobank. Fourth, we removed potential genetic instruments for HbA1c that also predicted BMI, as BMI causes CVD and hence could be a horizontal pleiotropic effect. Nevertheless, conclusions remain unchanged when we included these instruments (data not shown). Fifth, the genetic instruments for HbA1c were from people without diabetes, so our findings might be most relevant to these groups. Sixth, whilst our study provided genetic evidence that HbA1c impacts CVD risk, a phenome-wide Mendelian randomisation study in the UK Biobank would be useful to uncover possible mediating pathways in which HbA1c may impact CVD, as some (12 out of 29) of the HbA1c variants were related to biochemical traits, such as LDL-C and testosterone (ESM Fig. 4). Seventh, although we cannot rule out the possibility of violation of the exclusion restriction assumption, we have conducted multiple sensitivity analyses (e.g. MR-Egger, weighted median and MVMR) with different underlying assumptions, which gave similar conclusions.
Improving an individual’s glycaemic profile remains one of the central goals of effective diabetes management, minimising morbidity and mortality by reducing the risk of diabetes-related cardiovascular complications [7]. Consistent with a previous Mendelian randomisation study [13], our study adds genetic evidence that lowering HbA1c in participants, even in those with a normal spectrum of HbA1c (<39 mmol/mol [5.7%]), can reduce cardiovascular risk in a dose-dependent manner, implying potential cardioprotective effects of controlling blood glucose levels before impaired glucose regulation occurs in the general population. However, further investigation into the role of glycaemic control or the choice of glucose-lowering medications in different sub-populations may be warranted, especially as some trials showed intensive glycaemic control may not reduce CVD risk amongst people with type 2 diabetes [46, 47]. Additionally, the joint role of HbA1c in cardiovascular risk along with other aspects of glucose metabolism including insulin resistance and pancreatic beta cell dysfunction should be explored further.
This Mendelian randomisation study suggests genetically predicted HbA1c impacts CAD, and probably stroke and hypertension. The shape of the genetic association of HbA1c with these cardiovascular outcomes, in particular CAD, is likely linear.
Data availability
This research has been conducted using the UK Biobank Resource (application 14,864), which is available on request (https://www.ukbiobank.ac.uk/enable-your-research/apply-for-access). The genetic variants used as instrumental variable are provided in ESM Tables 2 and 3.
Abbreviations
- CAD:
-
Coronary artery disease
- CVD:
-
Cardiovascular disease
- DBP:
-
Diastolic BP
- GRS:
-
Genetic risk score
- GWAS:
-
Genome-wide association study
- Hgb:
-
Haemoglobin
- IVW:
-
Inverse-variance weighted
- LACE:
-
Localised average causal effect
- LDL-C:
-
Low density lipoprotein cholesterol
- MR-Egger:
-
Mendelian randomisation-Egger
- MVMR:
-
Multivariable Mendelian randomisation
- SBP:
-
Systolic BP
- UVMR:
-
Univariable Mendelian randomisation
References
American Diabetes Association (2020) 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2020. Diabetes Care 43(Suppl 1):S14–S31. https://doi.org/10.2337/dc20-S002
Cavero-Redondo I, Peleteiro B, Alvarez-Bueno C, Rodriguez-Artalejo F, Martinez-Vizcaino V (2017) Glycated haemoglobin A1c as a risk factor of cardiovascular outcomes and all-cause mortality in diabetic and non-diabetic populations: a systematic review and meta-analysis. BMJ Open 7(7):e015949. https://doi.org/10.1136/bmjopen-2017-015949
Emerging Risk Factors C, Di Angelantonio E, Gao P et al (2014) Glycated hemoglobin measurement and prediction of cardiovascular disease. JAMA 311(12):1225–1233. https://doi.org/10.1001/jama.2014.1873
Myint PK, Sinha S, Wareham NJ et al (2007) Glycated hemoglobin and risk of stroke in people without known diabetes in the European Prospective Investigation into Cancer (EPIC)-Norfolk prospective population study: a threshold relationship? Stroke 38(2):271–275. https://doi.org/10.1161/01.STR.0000254549.75763.5f
Sun YQ, Burgess S, Staley JR et al (2019) Body mass index and all cause mortality in HUNT and UK Biobank studies: linear and non-linear mendelian randomisation analyses. BMJ 364:l1042. https://doi.org/10.1136/bmj.l1042
Carslake D, Davey Smith G, Gunnell D, Davies N, Nilsen TIL, Romundstad P (2018) Confounding by ill health in the observed association between BMI and mortality: evidence from the HUNT Study using offspring BMI as an instrument. Int J Epidemiol 47(3):760–770. https://doi.org/10.1093/ije/dyx246
American Diabetes Association (2020) 6. Glycemic targets: standards of medical care in diabetes-2020. Diabetes Care 43(Suppl 1):S66–S76. https://doi.org/10.2337/dc20-S006
Lawlor DA, Harbord RM, Sterne JA, Timpson N, Davey Smith G (2008) Mendelian randomization: using genes as instruments for making causal inferences in epidemiology. Stat Med 27(8):1133–1163. https://doi.org/10.1002/sim.3034
Ross S, Gerstein HC, Eikelboom J, Anand SS, Yusuf S, Pare G (2015) Mendelian randomization analysis supports the causal role of dysglycaemia and diabetes in the risk of coronary artery disease. Eur Heart J 36(23):1454–1462. https://doi.org/10.1093/eurheartj/ehv083
Au Yeung SL, Luo S, Schooling CM (2018) The impact of glycated hemoglobin (HbA1c) on cardiovascular disease risk: a Mendelian randomization study using UK Biobank. Diabetes Care 41(9):1991–1997. https://doi.org/10.2337/dc18-0289
Leong A, Chen J, Wheeler E et al (2019) Mendelian randomization analysis of hemoglobin A1c as a risk factor for coronary artery disease. Diabetes Care. https://doi.org/10.2337/dc18-1712
Au Yeung SL, Luo S, Schooling CM (2020) The impact of glycated hemoglobin on risk of hypertension: a Mendelian randomization study using UK Biobank. J Hypertens 38(1):38–44. https://doi.org/10.1097/HJH.0000000000002210
Burgess S, Malik R, Liu B et al (2021) Dose-response relationship between genetically proxied average blood glucose levels and incident coronary heart disease in individuals without diabetes mellitus. Diabetologia. https://doi.org/10.1007/s00125-020-05377-0
Peters TM, Holmes MV, Richards JB et al (2020) Sex differences in the risk of coronary heart disease associated with type 2 diabetes: a Mendelian randomization analysis. Diabetes Care. https://doi.org/10.2337/dc20-1137
Davies NM, Holmes MV, Davey Smith G (2018) Reading Mendelian randomisation studies: a guide, glossary, and checklist for clinicians. BMJ 362:k601. https://doi.org/10.1136/bmj.k601
Bycroft C, Freeman C, Petkova D et al (2018) The UK Biobank resource with deep phenotyping and genomic data. Nature 562(7726):203–209. https://doi.org/10.1038/s41586-018-0579-z
English E, Lenters-Westra E (2018) HbA1c method performance: the great success story of global standardization. Crit Rev Clin Lab Sci 55(6):408–419. https://doi.org/10.1080/10408363.2018.1480591
Wheeler E, Leong A, Liu CT et al (2017) Impact of common genetic determinants of hemoglobin A1c on type 2 diabetes risk and diagnosis in ancestrally diverse populations: a transethnic genome-wide meta-analysis. PLoS Med 14(9):e1002383. https://doi.org/10.1371/journal.pmed.1002383
Genomes Project Consortium, Abecasis GR, Auton A et al (2012) An integrated map of genetic variation from 1,092 human genomes. Nature 491(7422):56–65. https://doi.org/10.1038/nature11632
Sun BB, Maranville JC, Peters JE et al (2018) Genomic atlas of the human plasma proteome. Nature 558(7708):73–79. https://doi.org/10.1038/s41586-018-0175-2
Burgess S, Dudbridge F, Thompson SG (2016) Combining information on multiple instrumental variables in Mendelian randomization: comparison of allele score and summarized data methods. Stat Med 35(11):1880–1906. https://doi.org/10.1002/sim.6835
Altman DG, Bland JM (2003) Statistics Notes - interaction revisited: the difference between two estimates. Bmj-Brit Med J 326(7382):219–219. https://doi.org/10.1136/bmj.326.7382.219
Bowden J, Del Greco MF, Minelli C, Davey Smith G, Sheehan N, Thompson J (2017) A framework for the investigation of pleiotropy in two-sample summary data Mendelian randomization. Stat Med 36(11):1783–1802. https://doi.org/10.1002/sim.7221
Bowden J, Davey Smith G, Burgess S (2015) Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol 44(2):512–525. https://doi.org/10.1093/ije/dyv080
Bowden J, Davey Smith G, Haycock PC, Burgess S (2016) Consistent estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol 40(4):304–314. https://doi.org/10.1002/gepi.21965
Bowden J, Del Greco MF, Minelli C, Davey Smith G, Sheehan NA, Thompson JR (2016) Assessing the suitability of summary data for two-sample Mendelian randomization analyses using MR-Egger regression: the role of the I2 statistic. Int J Epidemiol 45(6):1961–1974. https://doi.org/10.1093/ije/dyw220
Greco MF, Minelli C, Sheehan NA, Thompson JR (2015) Detecting pleiotropy in Mendelian randomisation studies with summary data and a continuous outcome. Stat Med 34(21):2926–2940. https://doi.org/10.1002/sim.6522
Au Yeung SL, Borges MC, Lawlor DA, Schooling CM (2021) Impact of lung function on cardiovascular diseases and cardiovascular risk factors: a two sample bidirectional Mendelian randomisation study. Thorax. https://doi.org/10.1136/thoraxjnl-2020-215600
Vuckovic D, Bao EL, Akbari P et al (2020) The polygenic and monogenic basis of blood traits and diseases. Cell 182(5):1214–1231 e1211. https://doi.org/10.1016/j.cell.2020.08.008
Rees JMB, Wood AM, Burgess S (2017) Extending the MR-Egger method for multivariable Mendelian randomization to correct for both measured and unmeasured pleiotropy. Stat Med 36(29):4705–4718. https://doi.org/10.1002/sim.7492
Burgess S, Thompson SG (2011) Bias in causal estimates from Mendelian randomization studies with weak instruments. Stat Med 30(11):1312–1323. https://doi.org/10.1002/sim.4197
Burgess S, Davies NM, Thompson SG, Consortium EP-I (2014) Instrumental variable analysis with a nonlinear exposure-outcome relationship. Epidemiology 25(6):877–885. https://doi.org/10.1097/EDE.0000000000000161
Staley JR, Burgess S (2017) Semiparametric methods for estimation of a nonlinear exposure-outcome relationship using instrumental variables with application to Mendelian randomization. Genet Epidemiol 41(4):341–352. https://doi.org/10.1002/gepi.22041
American Diabetes Association (2021) 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2021. Diabetes Care 44(Suppl 1):S15–S33. https://doi.org/10.2337/dc21-S002
Schottker B, Rathmann W, Herder C et al (2016) HbA1c levels in non-diabetic older adults - no J-shaped associations with primary cardiovascular events, cardiovascular and all-cause mortality after adjustment for confounders in a meta-analysis of individual participant data from six cohort studies. BMC Med 14:26. https://doi.org/10.1186/s12916-016-0570-1
Kozakova M, Palombo C (2016) Diabetes mellitus, arterial wall, and cardiovascular risk assessment. Int J Environ Res Public Health 13(2):201. https://doi.org/10.3390/ijerph13020201
Arvanitis M, Qi G, Bhatt DL et al (2020) A linear and non-linear Mendelian randomization analysis of the association between diastolic blood pressure and cardiovascular events: the J curve revisited. Circulation. https://doi.org/10.1161/CIRCULATIONAHA.120.049819
Georgakis MK, Harshfield EL, Malik R et al (2021) Diabetes mellitus, glycemic traits, and cerebrovascular disease: a Mendelian randomization study. Neurology. https://doi.org/10.1212/WNL.0000000000011555
Bower JK, Appel LJ, Matsushita K et al (2012) Glycated hemoglobin and risk of hypertension in the atherosclerosis risk in communities study. Diabetes Care 35(5):1031–1037. https://doi.org/10.2337/dc11-2248
Fisman EZ, Motro M, Tenenbaum A (2003) Cardiovascular diabetology in the core of a novel interleukins classification: the bad, the good and the aloof. Cardiovasc Diabetol 2:11. https://doi.org/10.1186/1475-2840-2-11
Iguchi Y, Kimura K, Shibazaki K et al (2012) HbA1c and atrial fibrillation: a cross-sectional study in Japan. Int J Cardiol 156(2):156–159. https://doi.org/10.1016/j.ijcard.2010.10.039
Erqou S, Lee CTC, Suffoletto M et al (2013) Association between glycated haemoglobin and the risk of congestive heart failure in diabetes mellitus: systematic review and meta-analysis. Eur J Heart Fail 15(2):185–193. https://doi.org/10.1093/eurjhf/hfs156
Harati H, Zanetti D, Rao A et al (2019) No evidence of a causal association of type 2 diabetes and glucose metabolism with atrial fibrillation. Diabetologia 62(5):800–804. https://doi.org/10.1007/s00125-019-4836-y
Schooling CM, Lopez PM, Yang Z, Zhao JV, Yeung SLA, Huang JV (2021) Use of multivariable Mendelian randomization to address biases due to competing risk before recruitment. Front Genet 11:ARTN 610852. https://doi.org/10.3389/fgene.2020.610852
Sanderson E, Spiller W, Bowden J (2020) Testing and correcting for weak and pleiotropic instruments in two-sample multivariable Mendelian randomisation. Hum Hered 84(4–5):223–223
Boussageon R, Bejan-Angoulvant T, Saadatian-Elahi M et al (2011) Effect of intensive glucose lowering treatment on all cause mortality, cardiovascular death, and microvascular events in type 2 diabetes: meta-analysis of randomised controlled trials. BMJ 343:d4169. https://doi.org/10.1136/bmj.d4169
Goldfine AB (2008) Assessing the cardiovascular safety of diabetes therapies. N Engl J Med 359(11):1092–1095. https://doi.org/10.1056/NEJMp0805758
Authors’ relationships and activities
The authors declare that there are no relationships or activities that might bias, or be perceived to bias, their work.
Funding
This study was funded by the Small Project Funding, the University of Hong Kong (#201409176231). The funder had no role in the design, analyses, interpretation of results or writing of the paper.
Author information
Authors and Affiliations
Contributions
SLAY and SL designed the study. SLAY and SL wrote the analysis plan. SL undertook analyses with feedback from SLAY and CMS. SLAY and SL drafted the manuscript with critical feedback and revisions from CMS. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. All authors gave final approval of the version to be published. SL is the guarantor of this study, as such, had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM
(PDF 706 kb)
Rights and permissions
About this article
Cite this article
Luo, S., Au Yeung, S.L. & Schooling, C.M. Assessing the linear and non-linear association of HbA1c with cardiovascular disease: a Mendelian randomisation study. Diabetologia 64, 2502–2510 (2021). https://doi.org/10.1007/s00125-021-05537-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-021-05537-w