Abstract
Influenza A, influenza B, severe acute respiratory syndrome coronavirus 2, adenovirus, respiratory syncytial virus, Mycoplasma pneumoniae, and Chlamydophila pneumoniae are common pathogens that can cause severe pneumonia and other symptoms, resulting in acute lower respiratory tract infections. The objective of this study was to design and evaluate a sensitive and specific multiplex one-step reverse transcription PCR (RT-PCR)–dipstick chromatography method for simultaneous rapid detection of these seven pathogens. Streptavidin-coated blue latex particles were used to read out a positive signal. Based on the DNA–DNA hybridization of oligonucleotide sequences (Tag) for forward primer with the complementary oligonucleotide sequence (cTag) on the dipstick and biotin–streptavidin interactions, PCR products were able to be illuminated visually on the dipstick. The specificity and the limit of detection (LOD) were also evaluated. Moreover, the clinical performance of this method was compared with Sanger sequencing for 896 samples. No cross reaction with other pathogens was found, confirming the high specificity of this method. The LOD was 10 copies/µL for each of the tested pathogens, and the whole procedure took less than 40 min. Using 896 samples, the sensitivity and specificity were shown to be no lower than 94.5%. The positive predictive value was higher than 82.1%, and the negative predictive value was higher than 99.5%. The kappa value between the PCR–dipstick chromatography method and Sanger sequencing ranged from 0.869 to 0.940. In summary, our one-step RT-PCR–dipstick chromatography method is a sensitive and specific tool for rapidly detecting multiplex respiratory pathogens.
Similar content being viewed by others
Introduction
Acute lower respiratory tract infections (ALRTIs) such as pneumonia, bronchitis, and bronchiolitis are major causes of morbidity and mortality worldwide [1, 2]. Respiratory viruses and atypical pathogens are important drivers of ALRTIs, including adenovirus (ADV), influenza A (IFA), influenza B (IFB), respiratory syncytial virus (RSV), Mycoplasma pneumoniae (MP), and Chlamydophila pneumoniae (CP) [3,4,5]. The current coronavirus disease 2019 (COVID-19) epidemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), also an ALRTI pathogen, often leads to severe pneumonia [6, 7]. A large number of studies have shown that common respiratory viruses and atypical pathogens including SARS-CoV-2, IFA, IFB, RSV, ADV, MP, and CP are closely related to severe pneumonia [6,7,8,9]. Since the clinical symptoms of these pathogens are similar, it is often difficult to clinically ascertain the exact pathogens causing ALRTIs in patients [10]. Moreover, these pathogens are highly infectious, quickly transmitted and often have high mixed infection rates [5]. Therefore, accurate and rapid identification is crucial for treating and controlling respiratory infectious diseases.
The General Office of the National Health Commission of China has clearly stated that COVID-19 is mainly differentiated from other known viral pneumonia and bacterial pneumonia, such as pneumonia caused by IFA, ADV, RSV, and MP [11]. To distinguish COVID-19 from these respiratory pathogens is meaningful for the treatment and clinical management of the current COVID-2019 epidemic. Therefore, it is important to establish a sensitive and specific method to rapidly distinguish these seven pathogens.
Molecular detection, as a rapid, sensitive, and specific assay, has been developed in the laboratory and in clinics, and is beneficial for promoting the early diagnosis of diseases, improving prognosis and reducing unnecessary treatments [12, 13]. In just a few short decades, molecular detection has undergone a dramatic change from single to multiple detection, making it a highly efficient tool. Multiple PCR detection strategies for respiratory pathogens, such as nucleic acid sequence-based amplification (NASBA), transcription-mediated amplification (TMA), strand displacement amplification (SDA), loop-mediated isothermal amplification (LAMP), and rolling circle amplification (RCA), have all been demonstrated for pathogen detection in recent years [14]. Currently, many PCR methods for detecting respiratory viruses or atypical pathogens, including dual priming oligonucleotide system (DPO), multiplex ligation-dependent probe amplification (MLPA) [15], and a multiplex PCR based on advanced fragment analysis, have all been used to identify respiratory pathogens [16]. Multiple enriched real-time fluorescent quantitative PCR [17], target-specific extension (TSE) [18], and target-enriched multiplex PCR (TEM-PCR) [18] are also currently being used in clinical or scientific research on respiratory pathogens. However, most of these multiplex PCR technologies rely on expensive basic laboratory equipment such as fluorescence PCR instruments and skilled technicians that are required to perform a sequence of cumbersome operations, or require lengthy follow-up results analysis programs [16]. The PCR–dipstick chromatography method, however, has been developed and applied to several fields, making it a good candidate for such multiplex assays [19,20,21].
In this study, we intended to develop a rapid, highly sensitive, and specific multiplex detection method for SARS-CoV-2, IFA, IFB, RSV, ADV, MP, and CP. Our method was based on DNA–DNA hybridization between the oligonucleotide (Tag) from PCR amplicons and complementary oligonucleotide (cTag) on a dipstick strip [19, 22, 23], with PCR products being able to be illuminated visually within 5–10 min. Neither did it require tedious operations nor did it use complex or expensive instruments. Ours is the first PCR–dipstick chromatography method to achieve the simultaneous analysis of seven respiratory pathogens.
Materials and Methods
Pathogen Strains and Plasmids
Human respiratory syncytial virus (ATCC® VR-1580) was cultured on Hep-2 cells in culture solution incubated at 37 °C for 7 days in 5% CO2. Human adenovirus (ATCC® VR-847) was cultured on Hep-2 cells in culture solution incubated at 37 °C for 6 days in 5% CO2. Influenza A virus (ATCC® VR-1469) was cultured on MDCK cells in culture solution incubated at 37 °C for 5 days in 5% CO2. The culture solution was Dulbecco’s modified eagle medium (DMEM, Gibco, Guangzhou, China) containing 4% fetal bovine serum (Invitrogen, Beijing, China). Mycoplasma pneumoniae (ATCC® 29,342) were cultured on broth (Solarbio, Guangzhou, China) incubated at 37 ℃ for 6 days in 5% CO2. Influenza B virus genomic RNA (ATCC® VR1735D) was isolated from a preparation of cell lysate and supernatant from MDCK cells (ATCC® CCL3) infected with influenza B virus, which was suitable for use in RT-PCR or other molecular procedures. Human respiratory syncytial virus (ATCC® VR-1580), human adenovirus (ATCC® VR-847), influenza A virus (ATCC® VR-1469), and influenza B virus genomic RNA (ATCC® VR1735D) were acquired from the American Type Culture Collection (Manassas, VA, USA). SARS-CoV-2 and Chlamydophila pneumoniae were acquired from clinical residual samples in Guangdong Provincial Hospital of Chinese Medicine based on the results of Sanger sequencing performed by The Beijing Genomics Institute (BGI, Beijing, China). DNA/RNA was extracted from these pathogen strains using a virus RNA/DNA rapid extraction kit following the manufacturer’s protocol. Plasmids for SARS-CoV-2, IFA, IFB, RSV, ADV, MP, and CP were acquired from Sangon Biotech Co., Ltd. (Shanghai, China).
Materials for PCR–Dipstick Chromatography Method
RT enzyme mixture (Luna Universal Probe One-Step RT-qPCR Kit) was bought from New England Biolabs (Guangzhou, China). A 10 × PCR buffer, dU plus dNTP mixture, uracil-N-glycosylase (UNG), and Taq HS polymerase were bought from Takara (Beijing, China). (NH4)2SO4 (200 mM) and MgSO4 (100 mM) were bought from Sigma-Aldrich (Shanghai, China). Dipstick strips, eluent reagents (containing detergents, blocking agents, PBS, and salt solution), and streptavidin-coated blue latex particles suspension were purchased from Tohoku Bio-Array, Co., Ltd. (TBA, Sendai, Japan). A viral RNA/DNA rapid extraction kit was acquired from Guangzhou Biotron Technology Co., Ltd., China.
Clinical Samples
To evaluate the clinical performance of our assay, a total of 896 residual samples were collected from March 2019 to April 2020, including nose or pharynx swabs and sputum samples in Guangdong Provincial Hospital of Chinese Medicine.
Patients were enrolled in the study based on the following criteria: patients with respiratory symptoms such as cough, wheezing, acute fever with temperature above 37.5 °C, and normal or low leukocyte count. This consisted of 513 male cases and 383 female cases, with 293 being were under 5 years old, 232 cases between 5 and 18 years old, 151 cases from 19 to 60 years old, and 220 cases over 60 years of age. The detection rates of pathogens were compared and analyzed by gender and age using these clinical samples. The samples were taken in a tube containing 2 mL viral transport medium (Yocon biotechnology Co., Ltd., Beijing, China). DNA/RNA was extracted from these samples using a virus RNA/DNA rapid extraction kit following the manufacturer’s protocol. RNA/DNA extractions were stored at − 80 °C before use.
Primers and Probes
For each pathogen, primers for conserved sequences were designed using Primer Premier 5 and further tested using NCBI blast to ensure the specificity of these primers. The primers included those targeting the SARS-CoV-2 N and ORF1ab genes, IFA, IFB, RSV, ADV, MP, and CP. Primers for the N and ORF1ab genes were designed together to confirm an accurate result for SARS-CoV-2. Moreover, an internal control (internal control, IC) was indispensable to ensure the reliability of the results and to prevent the influence of samples, instruments, reagents, operations, etc. IC was a segment of the synthetic sequence (CAGAGCACAGAGACACCACTGACGTGCCTGAGATGCCTCACTCCAAGGGCCAGGGAGAGAGCGATCCTCTGGACCATGAGCCTGCCGTGTCTCCATTGCTCCCTCGAAAAGAGCGAGGTCCCCCGGAGGGCGGCCTGAATGAAGATGAGCGCC). The homology of IC with the target genes was extremely low, meaning this would not trigger cross reactions. A pair of primers were also designed for IC. The IC, primers (Supplemental Table 1), and probes (Supplemental Table 2) used here were synthesized by TBA.
One-Step Reverse Transcription PCR (RT- PCR)
One-step RT-PCR was performed in a total volume of 25 μL, which included 2.5 μL of 10 × PCR buffer, 2.5 μL of DNA template, 0.4 μL of (10 μM) forward primer, and 0.4 μL of (10 μM) reverse primer for SARS-CoV-2 N and ORF1ab gene, ADV, RSV, and CP, respectively; 0.35 μL of (10 μM) forward primer and 0.35 μL of (10 μM) reverse primer for IFA, IFB, and MP; 0.3 μL of (2 μM) IC forward primer and 0.3 μL of (2 μM) IC reverse primer, 1 μL of (1 nM) IC DNA, 1.2 μL of RT enzyme mixture, 1 μL of dU plus dNTP mixture, 0.02 μL of uracil-N-glycosylase (UNG), 0.3 μL of Taq HS polymerase, 0.2 μL of 100 mM MgSO4, and 1 μL of 200 mM (NH4)2SO4; and deionized water was added to make a total volume of 25 μL. PCR amplifications were carried out using the Veriti 96-Well Thermal Cycler system. The cycling condition included reverse transcription at 55 °C for 5 min and preincubation at 95 °C for 1 min, followed by an amplification program for a total of 35 cycles comprising denaturation, 95 °C for 5 s; annealing and extension, 60 °C for 20 s. The total run time was approximately 30 min.
Dipstick Chromatography
The structure of the dipstick strip (2 mm × 60 mm) (Supplemental Fig. 1) was as follows. The supporting substrate was polyvinyl chloride (PVC) membrane, and the main functional structure was an absorbent area and a sample application area. The absorbent area was made of absorbent filter paper, which facilitated the capillary action for chromatography. The sample application area was made of nitrocellulose (NC) membrane, with 4 red position lines, and 9 test lines on it. The cTag were immobilized on the test line. The multiplexing cTags on a dipstick strip ensured that multiplex detection on one dipstick strip simultaneously was feasible.
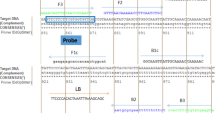
For each target, Tag was uniquely labeled at the 5′ terminus of forward primer with a phosphoramide spacer C3 [three-carbon spacer, (CH2)3]. This insertion was significant for the PCR amplification terminated at the insertion site, so that the Tag was isolated during the PCR reaction [24]. Reverse primers were all labeled with biotin. The cTag was complementary to the respective probe Tag immobilized on the dipstick strip for hybridization. Streptavidin-coated blue latex particles were set as the signal reporter to emit visible signal of the target through streptavidin–biotin interaction. After PCR, 10 μL of PCR amplicons, 1 μL of streptavidin-coated blue latex particles suspension, and 9 μL of eluent were mixed together to make a mixture (Fig. 1a). As the strip was inserted into the mixture, target DNA would be attached to the test line on the strip through the sequence complementarity of Tag and cTag (Fig. 1b). Meanwhile, the streptavidin-coated blue latex particles would attach to the test line through streptavidin–biotin interaction. As the blue latex particles accumulated, a blue test line appeared when there were target PCR amplicons present in the mixture (Fig. 1c). The run time was within 10 min.
Schematic diagram of the PCR–dipstick chromatography method. a Making a mixture. b Inserting a dipstick strip into the mixture. c A blue test line appeared on the dipstick strip. Tag: oligonucleotide; cTag: complementary; C3: C3 Spacer (linker); IC: Internal control; Arrow: chromatography direction (Color figure online)
Specificity of the PCR–Dipstick Chromatography Method
To confirm the specificity of the PCR–dipstick DNA chromatography method, 11 viruses that may cause similar symptoms or which were highly homologous with these seven pathogens were included in the verification of specificity. These consisted of Parainfluenza virus 1, 2, 3, 4, Coronavirus 229E, Coronavirus NL63, Coronavirus OC43 and Coronavirus HKU1, Metapneumovirus, Boca virus, and Rhinovirus.
Additionally, 12 organisms that may cause similar symptoms as these seven pathogens were included in the verification of specificity, including Escherichia coli, Staphylococcus aureus, Pseudomonas aeruginosa, Acinetobacter baumannii, Streptococcus pneumoniae, Streptococcus pyogenes, Staphylococcus epidermidis, Haemophilus, Klebsiella pneumoniae, Candida albicans, Legionella pneumophila, and Bordetella pertussis. All assays were performed in triplicate.
Limit of Detection (LOD) of the PCR–Dipstick Chromatography Method
To determine the LOD of the PCR–dipstick chromatography method, single detection of SARS-CoV-2, IFA, IFB, RSV, ADV, MP, and CP was carried out with mixed primers. Plasmids for SARS-CoV-2, IFA, IFB, RSV, ADV, MP, and CP were diluted with Tris–EDTA buffer (TE, Beyotime, Shanghai, China) to 105, 104, 103, 100, 10, 5 copies/µL, and then, the LOD of the dipstick strips were determined using visual inspection. All assays were performed in triplicate.
Clinical Performance
A total of 896 clinical samples were assessed to determine the efficacy of the PCR–dipstick chromatography method for detecting infectious pathogens on clinical nose or pharynx swabs and sputum samples. The sensitivity and specificity of the PCR–dipstick chromatography method were obtained by comparing with the results of Sanger sequencing. Sanger sequencing was performed as follows: 20 μL of the sequencing solution consisting of 5 μL of 5 × GoldStar PCR Buffer, 0.2 μL of (25 mM) dNTP Mixture, 0.3 μL of GoldStar DNA Polymerase, 1 μL of (10 µM) forward primer, 1 μL of (10 µM) reverse primer, 7.5 μL of RNase free water, and 10 μL of the target DNA was mixed together. The cycling condition included an initial denaturation at 95 °C for 5 min, followed by 32 cycles at 95 °C for 15 s, 55 °C for 30 s, 72 °C for 1 min, and a final extension at 72 °C for 5 min. A negative and a positive control were used for all sequencing reactions.
Data Analysis
SPSS 25 software was used to calculate statistics on all assay results. The test results for clinical performance were evaluated in comparison to Sanger sequencing results by the Cohen’s kappa coefficient test. A kappa value from 0.21 to 0.4 represents fair agreement, while from 0.41 to 0.6 represent moderate agreement and 0.61 to 0.8 and 0.81 to 0.99 indicate substantial and perfect agreement, respectively. The sensitivity = the number of true positive cases/[true positives + false negatives], the specificity = the number of true negative cases/[true negatives + false positives], positive predictive value (PPV) = the number of true positive cases/ [true positives + false positives], and negative predictive value (NPV) = the number of true negative cases/[true negatives + false negative cases]. Moreover, the detection rate of pathogens by gender and age using clinical samples was analyzed by the Pearson chi-square test since the total number of all the cells were above 40, and the expected values of each cell were above 5. In all tests, P < 0.01 was considered to be statistically significant.
Results
Methodological Validation of the Dipstick Chromatography Method
Blue-colored latex particles coated with streptavidin were able to be absorbed into the strip through capillary action. The IC was placed on the top of the dipstick strip to ensure the proper function and the reliability of all results and to capture excess latex particles, indicating that the amount of blue latex particles was available to all the PCR products [19]. The appearance of a blue line at the IC line demonstrated the validity of the results for this method. As shown in Fig. 2, dipstick strips with all seven target DNA were readily observed. No cross reactions appeared, indicating the reliability of this method.
Specificity of the PCR–Dipstick Chromatography Method
For addressing specificity, DNA templates for these seven target pathogens were next separated into two parts. The templates of positive control 1 consisted of DNA extraction mixture from SARS-CoV-2, IFA, and IFB, while the templates for positive control 2 consisted of DNA extraction mixture from RSV, ADV, MP, and CP.
As the results showed in Fig. 3, the 11 viruses Parainfluenza virus 1, 2, 3, 4, Coronavirus 229E, NL63, OC43 and HKU1, Metapneumovirus, Boca virus, and Rhinovirus were not detected, indicating that no cross reaction was observed with the seven target pathogens using the PCR–dipstick chromatography method.
Specificity of the PCR–dipstick chromatography method. PC1: multiplex detection of Severe acute respiratory syndrome coronavirus 2, Influenza A, and Influenza B; PC2: multiplex detection of Respiratory syncytial virus, Adenovirus, Mycoplasma pneumoniae, and Chlamydophila pneumoniae; 1. Parainfluenza virus 1; 2. Parainfluenza virus 2; 3. Parainfluenza virus 3; 4. Parainfluenza virus 4; 5. Coronavirus 229E; 6. Coronavirus NL63; 7. Coronavirus OC43; 8. Coronavirus HKU1; 9. Metapneumovirus; 10. Boca virus; 11. Rhinovirus; NC: Negative control
Additionally, 12 organisms that may cause similar symptoms or have high homology with these seven pathogens were also included in the verification of specificity, consisting of Escherichia coli, Staphylococcus aureus, Pseudomonas aeruginosa, Acinetobacter baumannii, Streptococcus pneumoniae, Streptococcus pyogenes, Staphylococcus epidermidis, Haemophilus, Klebsiella pneumoniae, Candida albicans, Legionella pneumophila, and Bordetella pertussis. As the results shown in Fig. 4, no cross reaction was observed on the dipstick strips.
Specificity of the PCR–dipstick chromatography method. PC1: multiplex detection of Severe acute respiratory syndrome coronavirus 2, Influenza A, and Influenza B; PC2: multiplex detection of Respiratory syncytial virus, Adenovirus, Mycoplasma pneumoniae, and Chlamydophila pneumoniae; 1. Escherichia coli; 2. Staphylococcus aureus; 3. Pseudomonas aeruginosa; 4. Acinetobacter baumannii; 5. Streptococcus pneumoniae; 6. Streptococcus pyogenes; 7. Staphylococcus epidermidis; 8. Haemophilus; 9. Klebsiella pneumoniae; 10. Candida albicans; 11. Legionella pneumophila; 12. Bordetella pertussis; NC: Negative control
Limit of Detection Determination of the PCR–Dipstick Chromatography Method
The LOD of the PCR–dipstick chromatography method was evaluated using plasmids for each pathogen, so as to eliminate the impact of the templates of pathogen strains or samples, as well as to evaluate the LOD accurately. As shown in Fig. 5, the LOD of the PCR–dipstick chromatography method was 10 copies/µL for SARS-CoV-2, IFA, IFB, RSV, ADV, MP, and CP.
Limit of detection determination of the PCR–dipstick chromatography method. a Severe acute respiratory syndrome coronavirus 2; b Influenza A, c Influenza B; d Respiratory syncytial virus; e Adenovirus; f Mycoplasma pneumoniae; g Chlamydophila pneumoniae. The concentration of plasmids 1–6 were 105, 104, 103, 100, 10, 5 copies/μL, and negative control (NC)
Clinical Performance
Results from the PCR–dipstick chromatography method were next compared with Sanger sequencing, as Sanger sequencing was the gold standard for many clinical research with its high accuracy. Cases of SARS-CoV-2, IFA, IFB, RSV, ADV, MP, and CP detected using the PCR–dipstick chromatography method among the 896 samples tested are shown in Table 1. Co-infection cases included 3 with IFA and IFB, 1 with IFA and ADV, 3 with IFA and MP, 1 with IFB and ADV, 3 with IFB and MP, 1 with IFB and RSV, 6 with RSV and ADV, 1 with RSV and MP, 9 with ADV and MP, and 2 with IFB, ADV, and MP. The sensitivity and specificity as well as PPV and NPV comparing between the PCR–dipstick chromatography method and Sanger sequencing are also shown in Table 1. The kappa value between them ranged from 0.869 to 0.940.
Additionally, differences of detection rate were compared by gender and ages. The results showed that there were no statistically significant differences (P > 0.01) in gender distribution between male and female for each pathogen (Table 2).
As for the differences in detection rate by age (Table 3), there were no statistically significant differences (P > 0.01) for IFA and CP, but there were statistically significant differences (P < 0.01) for SARS-CoV-2, IFB, RSV, ADV, and MP. The detection rate was highest in the age group from 19 to 60 years of age, followed by the age group of over 60 years for SARS-CoV-2. As for IFB, the detection rate was higher in the ≤ 18 years old group than in the ≥ 19 age groups. When it came to RSV and ADV, the age group under 5 years old had the highest detection rate. The age group from 5 to 18 presented the highest detection rate for MP.
Discussion
In this study, we designed a multiplex PCR–dipstick chromatography method for simultaneously detecting seven common respiratory viruses and atypical pathogens. The following respiratory viruses and atypical pathogens were selected: SARS-CoV-2, IFA, IFB, RSV, ADV, MP, and CP, as they can cause severe pneumonia. In addition, distinguishing IFA, IFB, RSV, ADV, MP, and CP from SARS-CoV-2 was of great significance for differential diagnosis during the current global outbreak of COVID-19. At present, there has been no research on the application of this method to the multiplex detection of respiratory pathogens, as well as the combined detection of these seven pathogens. Early and accurate diagnosis of the causative pathogens in respiratory infections is essential for the appropriate administration of antiviral or antibacterial therapies, initiating effective infection control measures and reducing the length of hospital stays, as well as controlling health care costs [25, 26].
No cross reaction was observed with 11 viruses as well as 12 respiratory organisms using the PCR–dipstick chromatography method. This confirmed the high specificity of the PCR–dipstick chromatography method. The LOD of the PCR–dipstick chromatography method was 10 copies/μL, showing that the PCR–dipstick chromatography method was highly sensitive and specific. To evaluate the clinical performance of this method, 896 samples were tested, and the results were compared with Sanger sequencing. The PPV was higher than 82.1%, and the NPV was higher than 99.5%, which indicated that the accuracy of our method was high. However, as can be seen from the results, the sensitivity and specificity of ADV were lower than other pathogens, possibly because the primer of ADV was slightly less inclusive. Further study should optimize the primer of ADV.
By combining one-step RT-PCR with the dipstick chromatography, this method currently realized multiplex detection within 40 min. This was a very time-saving method, taking less time than other molecular diagnostic methods, and it cost much less than other molecular detection methods such as real-time PCR [21]. During the current COVID-19 epidemic, this test can be deployed to distinguish between COVID-19 and common pneumonia quickly, which is hugely significant. Existing PCR methods require either analysis of the PCR products using agarose gel electrophoresis or high infrastructure requirements, meaning it can only be used in large clinical laboratories or those with specialized clinicians, and often several hours are needed for the outcomes [27]. In contrast to this, our PCR–dipstick chromatography method has a minimum requirement for instruments, requiring only a thermocycler, which is especially significant in hospitals with small-scale clinical laboratories where no advanced equipment is available [19]. Thus, the performances of detection of the PCR–dipstick chromatography method and other multiplex PCR detection methods were compared, shown in supplementary Table 3. The LOD of the PCR–dipstick chromatography method is higher than other multiplex PCR methods, while the analytical specificity was all high. However, the diagnostic specificity was higher than MLPA, TSE, and real-time PCR, but lower than TEM-PCR, and the diagnostic sensitivity was higher than MLPA, TEM-PCR, TSE, and real-time PCR. When it came to test turnaround time, the PCR–dipstick chromatography method was quicker than any other multiplex PCR method mentioned here.
In addition, previous studies have shown that the PCR–dipstick chromatography method is more sensitive than gel electrophoresis [19, 28].
The major drawback of this study was the limited number of positive samples for several pathogens, such SARS-CoV-2 and CP. This affected the evaluation results of clinical performance. Additional positive samples should be assessed in future studies to further explore the accuracy of detection using this method.
Conclusion
In summary, the PCR–dipstick chromatography method is an easy alternative molecular diagnostic method and can help to manage infections in remote settings, as it decreases the result turnaround time and can be used to diagnose and treat positive patients in a timely manner. As a rapid detection method with high sensitivity and specificity, the PCR–dipstick chromatography method has a bright application future in PCR post-analysis in many additional fields.
Data Availability
All data and material were transparent in the study.
Code Availability
IBM SPSS Statistics 25 (Version 25.0.0.0, IBM Armonk, NY: Corp.)
References
Nair H, Simoes EA, Rudan I, Gessner BD, Azziz-Baumgartner E, Zhang J, Feikin DR, Mackenzie GA, Moiisi JC, Roca A, Baggett HC, Zaman SM, Singleton RJ, Lucero MG, Chandran A, Gentile A, Cohen C, Krishnan A, Bhutta ZA, Arguedas A, Clara AW, Andrade AL, Ope M, Ruvinsky RO, Hortal M, Mccracken JP, Madhi SA, Bruce N, Qazi SA, Morris SS, El AS, Weber MW, Scott J, Brooks WA, Breiman RF, Campbell H (2013) Global and regional burden of hospital admissions for severe acute lower respiratory infections in young children in 2010: a systematic analysis. Lancet 381(9875):1380–1390. https://doi.org/10.1016/S0140-6736(12)61901-1
Collaborators GDAI (2016) Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388(10053):1545–1602. https://doi.org/10.1016/S0140-6736(16)31678-6
Jain S, Williams DJ, Arnold SR, Ampofo K, Bramley AM, Reed C, Stockmann C, Anderson EJ, Grijalva CG, Self WH, Zhu Y, Patel A, Hymas W, Chappell JD, Kaufman RA, Kan JH, Dansie D, Lenny N, Hillyard DR, Haynes LM, Levine M, Lindstrom S, Winchell JM, Katz JM, Erdman D, Schneider E, Hicks LA, Wunderink RG, Edwards KM, Pavia AT, Mccullers JA, Finelli L (2015) Community-acquired pneumonia requiring hospitalization among U.S. Children. New Engl J Med 372(9):835–845. https://doi.org/10.1056/NEJMoa1405870
Prina E, Ranzani OT, Torres A (2015) Community-acquired pneumonia. Lancet 386(9998):1097–1108. https://doi.org/10.1016/S0140-6736(15)60733-4
Ruuskanen O, Lahti E, Jennings LC, Murdoch DR (2011) Viral pneumonia. Lancet 377(9773):1264–1275. https://doi.org/10.1016/S0140-6736(10)61459-6
Ellinghaus D, Degenhardt F, Bujanda L, Buti M, Albillos A, Invernizzi P, Fernández J, Prati D, Baselli G, Asselta R, Grimsrud MM, Milani C, Aziz F, Kässens J, May S, Wendorff M, Wienbrandt L, Uellendahl-Werth F, Zheng T, Yi X, de Pablo R, Chercoles AG, Palom A, Garcia-Fernandez A, Rodriguez-Frias F, Zanella A, Bandera A, Protti A, Aghemo A, Lleo A, Biondi A, Caballero-Garralda A, Gori A, Tanck A, Carreras Nolla A, Latiano A, Fracanzani AL, Peschuck A, Julià A, Pesenti A, Voza A, Jiménez D, Mateos B, Nafria Jimenez B, Quereda C, Paccapelo C, Gassner C, Angelini C, Cea C, Solier A, Pestaña D, Muñiz-Diaz E, Sandoval E, Paraboschi EM, Navas E, García Sánchez F, Ceriotti F, Martinelli-Boneschi F, Peyvandi F, Blasi F, Téllez L, Blanco-Grau A, Hemmrich-Stanisak G, Grasselli G, Costantino G, Cardamone G, Foti G, Aneli S, Kurihara H, Elabd H, My I, Galván-Femenia I, Martín J, Erdmann J, Ferrusquía-Acosta J, Garcia-Etxebarria K, Izquierdo-Sanchez L, Bettini LR, Sumoy L, Terranova L, Moreira L, Santoro L, Scudeller L, Mesonero F, Roade L, Rühlemann MC, Schaefer M, Carrabba M, Riveiro-Barciela M, Figuera Basso ME, Valsecchi MG, Hernandez-Tejero M, Acosta-Herrera M, Angiò MD, Baldini M, Cazzaniga M, Schulzky M, Cecconi M, Wittig M, Ciccarelli M (2020) Genomewide Association Study of severe Covid-19 with respiratory failure. New Engl J Med 383(16):1522–1534. https://doi.org/10.1056/NEJMoa2020283
Qiu H, Wu J, Hong L, Luo Y, Song Q, Chen D (2020) Clinical and epidemiological features of 36 children with coronavirus disease 2019 (COVID-19) in Zhejiang, China: an observational cohort study. Lancet Infect Dis 20(6):689–696. https://doi.org/10.1016/S1473-3099(20)30198-5
Berlin DA, Gulick RM, Martinez FJ (2020) Severe Covid-19. New Engl J Med 383(25):2451–2460. https://doi.org/10.1056/NEJMcp2009575
Berkley JA et al (2010) Viral etiology of severe pneumonia among Kenyan infants and children. JAMA 303(20):2051–2057. https://doi.org/10.1001/jama.2010.675
Hodinka RL (2016) Respiratory RNA viruses. Microbiol Spectr 4(4):H2–H28. https://doi.org/10.1128/microbiolspec.DMIH2-0028-2016
General Office of National Health Commission of the People’s Republic Of China OONA (2020) Diagnosis and treatment of corona virus disease-19 (7th trial edition)[J]. China Med 15(6):801–805. https://doi.org/10.3760/j.issn.1673-4777.2020.06.001
Yarbrough ML, Burnham CD, Anderson NW, Banerjee R, Ginocchio CC, Hanson KE, Uyeki TM (2018) Influence of molecular testing on influenza diagnosis. Clin Chem 64(11):1560–1566. https://doi.org/10.1373/clinchem.2018.289363
Akers IE, Weber R, Sax H, Böni J, Trkola A, Kuster SP (2017) Influence of time to diagnosis of severe influenza on antibiotic use, length of stay, isolation precautions, and mortality: a retrospective study. Influenza Other Respir Viruses 11(4):337–344. https://doi.org/10.1111/irv.12454
Das S, Dunbar S, Tang Y (2018) Laboratory diagnosis of respiratory tract infections in children – the state of the art. Front Microbiol. https://doi.org/10.3389/fmicb.2018.02478
Li H, Mccormac MA, Estes RW, Sefers SE, Dare RK, Chappell JD, Erdman DD, Wright PF, Tang YW (2007) Simultaneous detection and high-throughput identification of a panel of RNA viruses causing respiratory tract infections. J Clin Microbiol 45(7):2105–2109. https://doi.org/10.1128/JCM.00210-07
Reijans M, Dingemans G, Klaassen CH, Meis JF, Keijdener J, Mulders B, Eadie K, van Leeuwen W, van Belkum A, Horrevorts AM, Simons G (2008) RespiFinder: a new multiparameter test to differentially identify fifteen respiratory viruses. J Clin Microbiol 46(4):1232–1240. https://doi.org/10.1128/JCM.02294-07
Malhotra B, Swamy MA, Reddy PVJ, Kumar N, Tiwari JK (2016) Evaluation of custom multiplex real - time RT-PCR in comparison to fast-track diagnostics respiratory 21 pathogens kit for detection of multiple respiratory viruses. Virol J 13(91):1–7. https://doi.org/10.1186/s12985-016-0549-8
Lee WM, Grindle K, Pappas T, Marshall DJ, Moser MJ, Beaty EL, Shult PA, Prudent JR, Gern JE (2007) High-throughput, sensitive, and accurate multiplex PCR-microsphere flow cytometry system for large-scale comprehensive detection of respiratory viruses. J Clin Microbiol 45(8):2626–2634. https://doi.org/10.1128/JCM.02501-06
Tian L, Sato T, Niwa K, Kawase M, Tanner ACR, Takahashi N (2014) Rapid and sensitive PCR-dipstick DNA chromatography for multiplex analysis of the oral microbiota. Biomed Res Int. https://doi.org/10.1155/2014/180323
Ohshiro T, Miyagi C, Tamaki Y, Mizuno T, Ezaki T (2016) Development of a rapid diagnostic method for identification of Staphylococcus aureus and antimicrobial resistance in positive blood culture bottles using a PCR-DNA-chromatography method. J Infect Chemother 22(6):372–376. https://doi.org/10.1016/j.jiac.2016.02.013
Shanmugakani RK, Akeda Y, Yamamoto N, Sakamoto N, Hagiya H, Yoshida H, Takeuchi D, Sugawara Y, Kodera T, Kawase M, Laolerd W, Chaihongsa N, Santanirand P, Ishii Y, Hamada S, Tomono K (2017) PCR-dipstick chromatography for differential detection of carbapenemase genes directly in stool specimens. Antimicrob Agents Chemother 61(6):e17–e67. https://doi.org/10.1128/AAC.00067-17
Monden Y, Takasaki K, Futo S, Niwa K, Kawase M, Akitake H, Tahara M (2014) A rapid and enhanced DNA detection method for crop cultivar discrimination. J Biotechnol 185:57–62. https://doi.org/10.1016/j.jbiotec.2014.06.013
Kalogianni DP, Litos IK, Christopoulos TK, Ioannou PC (2009) Dipstick-type biosensor for visual detection of DNA with oligonucleotide-decorated colored polystyrene microspheres as reporters. Biosens Bioelectron 24(6):1811–1815. https://doi.org/10.1016/j.bios.2008.08.056
Niwa K, Oribe A, Okumura H, Shimono M, Nagai K, Hirota T, Yasue H, Kawase M (2014) Tag/hybridization-based sensitive detection of polymerase chain reaction products. Anal Biochem 464:12–16. https://doi.org/10.1016/j.ab.2014.07.010
Wertheim H, Nadjm B, Thomas S, Agustiningsih MS, Nguyen D, Vu D, Van Nguyen K, Van Nguyen CV, Nguyen LT, Tran ST, Phung T, Nguyen TV, Hien TT, Nguyen UH, Taylor W, Truong KH, Ha TM, Chokephaibulkit K, Farrar J, Wolbers M, de Jong MD, van Doorn HR, Puthavathana P (2015) Viral and atypical bacterial aetiologies of infection in hospitalised patients admitted with clinical suspicion of influenza in Thailand, Vietnam and Indonesia. Influenza Other Respir Viruses 9(6):315–322. https://doi.org/10.1111/irv.12326
Luchsinger V, Ruiz M, Zunino E, Martínez MA, Machado C, Piedra PA, Fasce R, Ulloa MT, Fink MC, Lara P, Gebauer M, Chávez F, Avendaño LF (2013) Community-acquired pneumonia in Chile: the clinical relevance in the detection of viruses and atypical bacteria. Thorax 68(11):1000–1006. https://doi.org/10.1136/thoraxjnl-2013-203551
Talbot HK, Falsey AR (2010) The diagnosis of viral respiratory disease in older adults. Clin Infect Dis. https://doi.org/10.1086/650486
Koiwai K, Kodera T, Thawonsuwan J, Kawase M, Kondo H, Hirono I (2018) A rapid method for simultaneously diagnosing four shrimp diseases using PCR-DNA chromatography method. J Fish Dis 41(2):395–399. https://doi.org/10.1111/jfd.12732
Acknowledgements
We thank Guangzhou Science and Technology plan project [grant number 202002020038, and 202103000025] and Chinese Medicine Science and Technology Research Project of Guangdong Provincial Hospital of Chinese Medicine [grant number YN2019QL05] for their financial funding.
Funding
This work was supported by Guangzhou Science and Technology Plan Project [grant number 202002020038, and 202103000025] and Chinese Medicine Science and Technology Research Project of Guangdong Provincial Hospital of Chinese Medicine [grant number YN2019QL05].
Author information
Authors and Affiliations
Contributions
This work was initiated by NX, HX, XSY, and LL; the acquisition data were made by NX, HX, LL, QMC, XZH, and QL; Qiang Luo, SQ, ZJL, Qiong Li, and SLZ were major providers of clinical material and details; data analysis or interpretation and preparation of the manuscript were carried out by LL, NX, HX, PFK, and QMC. All authors approved the final version and endorsed the guidance.
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Ethical Approval
All aspects of the study were performed in accordance with the ethical standards of the institutional research committee and in line with the 1964 Helsinki Declaration, and the study was approved by the Ethics Committee of Guangdong Provincial of Chinese Medicine (Approval Notice number: YE2020-079-01).
Consent to Participate
Not applicable.
Consent for Publication
We confirm that this work is original and has not been published elsewhere nor is currently under consideration for publication elsewhere.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Luo, L., Chen, Q., Qin, S. et al. Design and Evaluation of Multiplex One-Step Reverse Transcription PCR–Dipstick Chromatography Method for the Analysis of Seven Respiratory Pathogens. Curr Microbiol 78, 3656–3666 (2021). https://doi.org/10.1007/s00284-021-02621-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00284-021-02621-7