Abstract
Objectives
The objective of this study was to evaluate a US hospital’s cost implications and outcomes of cangrelor use in percutaneous coronary intervention (PCI) patients with two or more angiographic high-risk features (HRFs), including avoidance of oral P2Y12 inhibitor pretreatment in patients requiring cardiac surgery. Intravenous cangrelor provides direct, immediate onset and rapid-offset P2Y12 inhibition, which may reduce the necessity for oral P2Y12 pretreatment.
Methods
A decision analytic model was developed, estimating the annual impact over 3 years of cangrelor availability. Ischemic and bleeding events (48 h) from randomized clinical trial data were extrapolated to 30 days. Event costs were from the CHAMPION PHOENIX Economics substudy. Rates of coronary artery disease (CAD) presentation, PCI, oral P2Y12 pretreatment, and inpatient hospitalization costs were from published literature and clinical experts. Scenario analyses evaluated the impact of cangrelor availability on potential reduced P2Y12 pretreatment rates by 50–100%. Drug costs were 2019 wholesale acquisition costs and, where necessary, all costs were adjusted to 2019 dollars.
Results
In a hospital treating 1000 CAD PCI inpatients annually, increasing cangrelor use from 11 to 32% resulted in a reduction in 48-h ischemic events/year by 5.7%, while bleeding events increased by 2.9%. Total costs of $1,135,472 declined 12.8%, with a 50% reduction in P2Y12 pretreatment or 30% with no pretreatment. Savings were driven by a decrease in ischemic events, decrease in glycoprotein IIb/IIIa inhibitor use, and less need for and shorter oral P2Y12 inhibitor washout period for surgery patients.
Conclusion
Use of cangrelor in patients with two or more angiographic HRFs may improve outcomes and lower hospital budgets, mainly from avoiding surgery delays necessitated by oral P2Y12 inhibitor pretreatment.
Similar content being viewed by others
In patients with two or more angiographic high-risk features undergoing coronary revascularization, intravenous cangrelor provides potential cost savings at the hospital level by reducing periprocedural ischemic events while lowering the costs from delays in coronary artery bypass graft due to oral P2Y12 inhibitor pretreatment. |
Given these findings, as well as the lack of randomized data supporting P2Y12 inhibitor pretreatment in patients undergoing percutaneous coronary intervention (PCI), consideration should be given to the use of cangrelor during PCI in patients with high clinical or angiographic risk. |
1 Introduction
Clinical guidelines recommend combining anticoagulants with aspirin plus an oral P2Y12 inhibitor with or without glycoprotein IIb/IIIa inhibitors (GPI) during percutaneous coronary intervention (PCI) to reduce periprocedural ischemic events [1, 2]. However, oral P2Y12 inhibitors may exhibit slow onset of platelet inhibition and low response rates, especially among patients with acute coronary syndrome and ST-segment elevation myocardial infarction (STEMI) [3,4,5]. Delayed response may be due to high baseline platelet reactivity, reduced bioavailability of oral agents in STEMI patients, and delayed metabolism of thienopyridines into their active metabolites [5]. These issues are exacerbated with use of morphine or fentanyl [6, 7], which are often coadministered for chest pain and anxiety [3,4,5]. Consequently, prescribing information for oral P2Y12 inhibitors includes this risk of delayed and decreased absorption with concomitant opioid administration [8,9,10]. Recent guidance recommends against routine P2Y12 pretreatment of NSTEMI patients until the coronary anatomy is known. [1]. Patients may also have risk associated with lesion complexity, further underscoring the need for potent and prompt platelet inhibition. Immediate P2Y12 inhibition is important [3] but may not be achievable given mean PCI durations of < 20 min and rapid door-to-first-device times in STEMI [11].
Cangrelor, a novel, intravenous platelet P2Y12 receptor inhibitor, provides direct, immediate onset and rapid-offset P2Y12 inhibition for PCI. The safety and efficacy of cangrelor was evaluated in three trials: CHAMPION PHOENIX, CHAMPION PCI, and CHAMPION PLATFORM [11,12,13]. The significant reduction in ischemic events (major adverse cardiovascular event [MACE]: death, myocardial infarction (MI), ischemia-driven revascularization [IDR], or stent thrombosis [ST]) at 48 h versus clopidogrel in CHAMPION PHOENIX led to the approval of cangrelor. A pooled analysis of the CHAMPION trials confirmed that cangrelor was effective in reducing MACE [14]. Despite its demonstrated efficacy in an all-comers PCI population in CHAMPION PHOENIX, which was consistent in the US and non-US subgroups [15] and is included in recent clinical guidelines [1, 16, 17], in practice cangrelor may be restricted to subsets of PCI patients, such as those with high acuity presentation (STEMI, NSTEMI) and those who are unable to take oral antiplatelets. This limited use of cangrelor stems in part from its perceived impact on hospital budgets due to its acquisition cost compared with oral P2Y12 inhibitors.
An analysis from CHAMPION PHOENIX showed that angiographic high-risk features (HRFs) are a powerful predictor of 48-h MACE [18]. Angiographic HRFs include long lesions (> 20 mm), bifurcation (diameter of stenosis ≥ 50%), eccentric anatomy, tortuous (moderate/severe), angulated (moderate/severe), calcified (moderate/severe), left main (diameter of stenosis ≥ 50%), thrombotic lesions, or multi-lesion PCI [18]. Notably, a majority (56%) of patients presenting with stable angina undergoing PCI had two or more angiographic HRFs [18]. An analysis of CHAMPION PHOENIX evaluating timing of 48-h MACE found the vast majority of events, regardless of patient presentation, occurred within 2 h following randomization [19,20,21]. Thus, utilizing a potent, rapid-acting P2Y12 inhibitor during and immediately after PCI to reduce the risk of periprocedural ischemic events seems warranted [22]. Given cangrelor’s immediate (< 2 min) onset of action and its rapid (1 h post-discontinuation) offset, hospitals could decrease costs with cangrelor use by reducing the proportion of inpatients pretreated with oral P2Y12 inhibitors and thus potentially avoid prolonged hospitalization in patients who require delays to coronary artery bypass graft (CABG) surgery to allow for oral P2Y12 inhibitor washout.
The objective of the present study was to model the cost implications and outcomes from the perspective of a US hospital of using cangrelor in PCI patients with increasing numbers of angiographic HRFs, including the economic benefit of reducing oral P2Y12 inhibitor pretreatment and the subsequent delay to CABG in patients requiring surgery. The model was developed using Microsoft Excel 2016 software (Microsoft Corporation, Redmond, WA, USA).
2 Materials and Methods
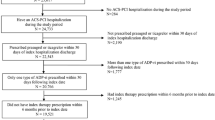
A decision analytic model was developed using Microsoft Excel (Fig. 1) to estimate annual costs and outcomes of treating an increasing number of angiographic HRF PCI patients with cangrelor and direct economic benefit from reduction in MACE, as well as the indirect economic benefit of reducing pretreatment with oral P2Y12 inhibitors, per the 2020 European Society of Cardiology (ESC) guidelines [1, 2]. The model adopted a 3-year time horizon, from the perspective of a US hospital, for coronary artery disease (CAD) patients requiring PCI or going directly to CABG. PCI patients were further stratified into four subgroups: those with none, one, two, or three or more angiographic HRFs. Since the angiographic HRFs are not known until after the angiogram, these levels were considered a reasonable proxy to represent the level of clinical risk in a patient about to undergo PCI. A similar proportion of patients across HRF subgroups were presumed to be pretreated before PCI with oral P2Y12 inhibitors. Periprocedural antiplatelet options were either cangrelor alone or clopidogrel with or without planned GPI (designated GPI use before PCI). It was assumed that a proportion of CABG patients pretreated with an oral P2Y12 inhibitor would also need antiplatelet or anticoagulant bridging therapy during the P2Y12 inhibitor washout period before surgery. We estimated outcomes and costs during the index admissions through 30 days for an annual population of CAD patients. Ethics approval was not required for this study since the analysis uses only published data from clinical trials.
Decision analytic model structure. CABG coronary artery bypass graft, CHD coronary heart disease, GPI glycoprotein IIb/IIIa inhibitors, NSTEMI non-ST segment elevation myocardial infarction, PCI percutaneous coronary intervention, SA stable angina, STEMI ST segment elevation myocardial infarction, UA unstable angina
3 Model Inputs
3.1 Target Population
Based on data from the Premier Hospital Database of inpatient charges, the proportion of CAD patients by diagnosis was 6%, 17%, and 77% for STEMI-ACS, NSTEMI/UA-ACS, and stable angina, respectively (Online Resource Table 1). Following angiography, 57% of patients had PCI and 5% went directly to CABG surgery. Of the patients designated for PCI, 99.8% received PCI and 0.2% received CABG surgery due to a complication during PCI [23]. In CHAMPION PHOENIX, among PCI patients, 17%, 32%, 27%, and 25% had none, one, two, or three or more angiographic HRFs, respectively. According to the literature, 33% of these patients received an oral P2Y12 inhibitor before PCI [24]. Due to its rapid onset of action, having cangrelor available could reduce the need to pretreat CAD patients. We simulated two scenarios where oral P2Y12 inhibitor pretreatment was reduced by 50% and 100%, respectively.
3.2 Utilization
Assumptions for base case and scenario analyses on the utilization of antiplatelet agents, illustrated in Table 1, were informed by clinical experts from the CHAMPION Executive Committee. We assumed low-risk patients (e.g. those with fewer than one angiographic HRF) were only treated with clopidogrel ± planned GPI, and high-risk patients (e.g. those with two or more angiographic HRFs) might be administered cangrelor. This model assumed an increasing proportion of high-risk patients received cangrelor over 3 years.
3.3 Ischemic Outcomes
Forty-eight-hour MACE rates by the subgroups of angiographic HRFs for cangrelor and clopidogrel patients were estimated from the literature [18]. According to Vaduganathan et al., the relative increase in 48-h ischemic events for patients treated with clopidogrel + planned GPI, compared with those treated with cangrelor, was 26.9% [25]. With this assumption, 48-h MACE for clopidogrel + planned GPI patients were extrapolated within each subgroup by applying the 26.9% increase relative to the rate for cangrelor patients. The stratification of 48-h MACE rates into individual MACE events for cangrelor, clopidogrel, and clopidogrel + planned GPI patients was based on an analysis by Cavender et al. [19,20,21]. The proportions were then multiplied by the 48-h MACE rates to obtain the individual ischemic events within subgroups and by treatment.
Based on the CHAMPION trials, increases in MACE of approximately 37% and 26% were observed from 48-h until 30 days among cangrelor- and clopidogrel-treated patients, respectively. The percentage increase for each treatment was then applied to the individual 48-h event rates estimated earlier to extrapolate the individual 30-day event rates. The individual 30-day ischemic event rates for clopidogrel + planned GPI patients were extrapolated relative to the cangrelor rates by the same approach. Table 2 illustrates both the 48-h and 30-day outcomes for death, MI, IDR, and ST events across angiographic HRF subgroups.
3.4 Bleeding Events
The 48-h combined (cangrelor alone and clopidogrel ± planned GPI) bleeding rates by angiographic HRFs from the CHAMPION PHOENIX trial were taken from the study by Stone et al. [18]. Events for two bleeding scales were reported: severe/moderate Global Strategies for Opening Occluded Coronary Arteries (GUSTO) and major/minor Thrombolysis in Myocardial Infarction (TIMI). The GUSTO bleeding definition uses clinical acuity and impact to categorize patients into severe or life-threatening, moderate, or mild categories, whereas the TIMI bleeding definition is based on laboratory values of hematocrit or hemoglobin after adjusting for blood transfusions to categorize bleeding severity as major, minor, or minimal [26]. Based on the relative ratio of bleeding rates reported in a pooled analysis of the CHAMPION trials (cangrelor versus clopidogrel) and in a propensity-matched analysis of cangrelor versus clopidogrel + planned GPI, the rates for each angiographic HRF subgroup were estimated by antiplatelet treatment (i.e. cangrelor alone, clopidogrel alone, and clopidogrel + planned GPI) [14, 25].
The MATRIX trial used heparin as an anticoagulant and demonstrated an increase of approximately 90% in Bleeding Academic Research Consortium (BARC 3 and 5) bleeding from day 2 (0.7%) to day 30 (1.33%) post PCI [26]. In CHAMPION PHOENIX, heparin was used as the predominant anticoagulant and therefore it was assumed that the same extent of increase could be used as a proxy for both GUSTO moderate/severe and TIMI major/minor bleeding. Therefore, the 90% increase was applied to the 48-h GUSTO and TIMI bleeding rates to estimate the corresponding 30-day bleeding rates. Table 2 illustrates both the 48-h and 30-day outcomes for death, MI, IDR, ST, and bleeding events across angiographic HRF subgroups.
3.5 Glycoprotein IIb/IIIa Inhibitor Bailout
GPI bailout is defined as the unplanned use of a GPI after the procedure start. In CHAMPION PHOENIX, the rate of GPI bailout was significantly lower among patients treated with cangrelor compared with clopidogrel [11].
3.6 P2Y12 Inhibitor Washout
Regardless of presentation, inpatients requiring CABG (either patients going direct to surgery following angiography, or cases during or following the index PCI procedure) who have previously been treated with an oral P2Y12 inhibitor may require ‘washing-out’ of the antiplatelet effect of these oral agents to reduce the risk of perioperative bleeding. This approach is recommended in practice guidelines as well as the package inserts for each of the oral P2Y12 inhibitors (7–9). An intravenous antiplatelet and/or intravenous anticoagulant may be initiated during the washout period to avoid ischemic events. The proportion of patients by duration of washout for each P2Y12 antiplatelet regimen was based on a Premier Database analysis of inpatient stays (Online Resource Table 3). In this model, it was assumed that clopidogrel + planned GPI has the same duration of washout as clopidogrel alone. In addition, as a simplifying assumption for washout costs, it was assumed patients taking an oral P2Y12 inhibitor would be switched to an intravenous antiplatelet during washout [17, 27]. We assumed the GPI would be stopped approximately 4 h before starting CABG surgery.
3.7 Economic Inputs
Ischemic event costs for MI, IDR, and ST were informed by the CHAMPION PHOENIX substudy (Online Resource Table 2). Published inpatient per diem cost was applied to the washout time [28]. Where necessary, all costs were adjusted to 2019 dollars using the medical component of the Bureau of Labor Statistics Consumer Price Index [29].
Potential GPI options for PCI included abciximab, eptifibatide, and tirofiban. The mix of GPI utilization was from the CHAMPION PCI trial. The GPI utilization mix applied in the washout period was adjusted to reflect the practice that only eptifibatide and tirofiban are employed for bridging. Drug costs were based on dosing regimens from the prescribing information of each drug and 2019 wholesale acquisition costs [30]. Table 3 contains the economic inputs used in the model.
3.8 Sensitivity Analyses
A deterministic sensitivity analysis (DSA) was performed to systematically examine the impact of each model parameter on the base-case model results. Parameter estimates varied by ± 20%, where possible; 100% was used as the maximum upper range where the 20% parameter variation could not be applied (i.e. if a parameter estimate was 90%, it would not have been possible to increase that parameter estimate by 18% [20% of 90%], as a percentage cannot exceed 100%).
4 Results
For a hypothetical hospital treating 1000 inpatient CAD patients, approximately 565 patients were expected to undergo PCI and 50 were expected to undergo CABG surgery each year. The remainder of patients were managed medically and were thus excluded from the cost analysis. Among the patients in whom PCI was planned, 99.8% (n = 564) received PCI, while 0.2% (1 patient) received CABG surgery during the index PCI admission (Online Resource Table 1) [23].
In the base case, oral P2Y12 pretreatment was assumed to be 33% and cangrelor use was 22% in patients with two or more angiographic HRFs (or 11% in all PCI patients). In other scenarios, oral P2Y12 pretreatment was assumed to be 17.5% (50% less than the base case) or 0% (no pretreatment at all), and cangrelor use in patients with two or more angiographic HRFs increased from 28% in year 1 to 62% in year 3 (or 15% in year 1 to 32% in year 3 in all PCI patients, while planned GPI use was reduced from 9% to 6% over the same time (Table 1).
The total annual number of 48-h MACEs was reduced from the base case of 32.5 to 30.7 by year 3 in the scenario (Fig. 2a). This percentage reduction versus base case was 1.1% in year 1 and 5.7% in year 3. A similar trend in reduction was seen for 30-day MACE (Fig. 2b).
(A) 48-hour ischemic events; (B) 30-day ischemic events; (C) 48-hour bleeding events; and (D) 30-day bleeding events. GUSTO Global Use of Strategies to Open Occluded Arteries, IDR ischemia-driven revascularization, MI myocardial infarction, ST stent thrombosis, TIMI thrombolysis in myocardial infarction
The total annual number of GUSTO severe/moderate bleeding events was increased from 0.65 (48-h) and 1.23 (30-day) in the base case to 0.67 (48-h) and 1.27 (30-day) by year 3 in the scenario. However, 48-h and 30-day TIMI major/minor bleeding events were similar for the base case and scenario (48-h = 0.24, 30-day = 0.45) (Fig. 2c, d). Using the GUSTO definition, bleeding event costs for 30-days remained flat (approximately $14,500–$15,000 per year, or < 2% of total costs) over the 3-year period.
Figure 3a, b show the total costs by category with reduced P2Y12 pretreatment (and no pretreatment) and increased cangrelor use over the 3-year period. The annual costs were projected to decline from $1,135,472 in the base case to $990,533 ($811,823 with no pretreatment) in year 3. With ischemic events comprising the majority of total costs (69.6% in the base case and 52.6% by year 3), costs decreased from $597,647 in the base case to $565,040 in year 3. A similar trend was observed in GPI bailout cost but at a smaller magnitude. Washout costs declined by 47%, from $380,752 in the base case to $199,934 ($21,224 with no pretreatment) in the scenario.
Total drug acquisition cost was the second-largest cost driver. Drug cost increased from $112,844 in the base case to $181,677 by year 3, representing an increase of 61%. The overall budget impact for years 1, 2, and 3 was −$179,947, −$162,883, and −$145,819, respectively, in the case of 50% reduced P2Y12 pretreatment, and −$358,278, −$340,964, and −$323,649 for years 1–3 when no P2Y12 pretreatment was simulated.
A DSA was performed by varying each point estimate by ±20%, where possible. The DSA demonstrated the model was most susceptible to epidemiology assumptions, including the proportion of patients in whom PCI was planned and the proportion of patients who were pretreated with oral P2Y12 inhibitors, impacting the model results by 20–50%. General ward costs impacted results by about 19%. All other parameters had a < 5% impact on model results. Figure 4 illustrates the top 10 inputs with greatest impact on the budget.
Deterministic sensitivity analysis on the 3-year cumulative budget impact (top 10 most influential model parameters). The values on the bars represent the low and high parameter estimate used for the sensitivity analysis. The size of the bar indicates the calculated 3-year cumulative budget impact with the respective low (input reduced by 20%) or high (input increased by 20%) parameter estimate. The base 3-year cumulative budget impact is −$102,289. CHD coronary heart disease, Clopi clopidogrel, GPI glycoprotein IIb/IIIa inhibitors, MACE major adverse cardiovascular event, MI myocardial infarction, PCI percutaneous coronary intervention
5 Discussion
The present analysis is the first health economic evaluation developed to estimate the clinical and economic impact of using antiplatelet agents in PCI patients and considering subgroups of increasing angiographic risk. This model suggests the budget of a hospital with a constant level of PCI procedures may decline by 13–30% (assuming a 50–100% reduction in P2Y12 pretreatment rate) by year 3 if the utilization of cangrelor is increased from 22% in the base case to 62% in year 3 in PCI patients with two or more angiographic HRFs.
The cost savings are driven by three main benefits: (1) reduction in ischemic events; (2) reduction in GPI bailout use; and (3) reduced costs for washout of oral P2Y12 inhibitors due to reduced pretreatment. Cost savings from these benefits offset the increase in drug cost and bleeding costs, leading to a decrease in cumulative 3-year costs of $488,649 (14.3%) or $1,022,891 (30%) for the scenarios of 50% reduced pretreatment and no pretreatment, respectively.
The CHAMPION PHOENIX angiographic core laboratory analysis indicated improved clinical outcomes with cangrelor for all PCI patients, but greater absolute ischemic benefit was seen in the patients with two or more angiographic HRFs; thus, this was the patient population for which we simulated increased use of cangrelor. This benefit was quantified in the model as a reduction in MACE, translating into cost savings of approximately 5.5% by year 3. Patients treated with cangrelor compared with clopidogrel also experienced lower GPI bailout rates, which led to cost savings in GPI bailout of about 2.6% by year 3.
Moreover, having cangrelor available for PCI may affect the proportion of CAD patients pretreated with an oral P2Y12 inhibitor. Patients receiving cangrelor would not require pretreatment with an oral P2Y12 inhibitor prior to angiography due to the immediate onset of action of cangrelor. Should these patients require surgery post angiography and remain hospitalized, the rapid offset of cangrelor would not impact scheduling of surgery, and thus be expected to reduce the length of stay prior to surgery. The washout period [2, 8,9,10] increases the length of stay in these patients, thereby increasing costs (e.g. > 50% of cangrelor patients were able to have surgery within 1 day post PCI) (Fig. 4). If pretreatment is reduced by 50% with the use of cangrelor, washout costs by year 3 are expected to be reduced by $180,818 (47.5%) or $359,529 (94%) with no pretreatment. Similar savings might be realized for hospitals implementing the 2020 NSTEMI ESC guidelines [1].
The use of cangrelor for PCI has been shown to result in a slightly increased incidence of non-severe bleeding compared with clopidogrel, which may lead to higher bleeding event costs [14]. Consistent with published sources, the bleeding events estimated in the model also showed a very slight increase in GUSTO major/moderate bleeding with higher utilization of cangrelor, and therefore bleeding event costs increased only nominally or were similar using the TIMI bleeding definition.
The sensitivity analysis indicated the model was most sensitive to the proportion of patients in whom PCI was planned, which is not surprising since they represent over 90% of the patients simulated. The model is also sensitive to the inputs relating to the patients requiring washout, such as the proportion of pretreatment and general ward costs that a hospital might incur from pretreating CABG patients.
These results provide insights about the potential benefits of increasing use of cangrelor among patients with two or more angiographic HRFs. This study also highlights a potential need in stable angina patients. Traditionally, patients with stable angina are perceived to be low-risk as many of these patients receive elective PCI procedures and therefore are typically not considered to be candidates for cangrelor. However, as more than half of the stable angina patients undergoing PCI procedures have two or more angiographic HRFs and are typically managed as outpatients, there may be opportunity for improvement in periprocedural ischemic outcomes, reduction in need for GPI bailout, and shorter duration of washout in this population [18]. Reduction in the need for GPI, whether routine or bailout, may also reduce bleeding, thereby further reducing the cost of acute care [31].
The model has a number of limitations. First, due to the short duration of cangrelor use periprocedurally, cangrelor affects outcomes predominantly in the first 48 hs, whereas the events occurring after the first 48 h may be attributable to the oral P2Y12 inhibitor prescribed for secondary prevention of cardiovascular events. However, the early reduction in ischemic events associated with cangrelor use is preserved out to 30 days [14]. In the model, the 48-h clinical outcomes were extrapolated to 30 days as 30-day outcomes are commonly used as quality metrics [32]. The model quantifies the hospitalization costs of washout and bridging, but ignores any harms associated with antiplatelet therapy during washout. However, this simplifying assumption is expected to lead to an underestimate of the total savings in the scenario with lower use of oral P2Y12 pretreatment. This model exclusively evaluated cangrelor and clopidogrel ± planned GPI use. In contemporary practice, prasugrel or ticagrelor are often used in ACS, but these agents were excluded from the analysis because they have not been extensively studied in the periprocedural setting (i.e. with 48-h endpoints). Nevertheless, the impact of using the newer oral P2Y12 inhibitors on results of this model should be minimal as the effect of cangrelor is observed within the first few hours [33]. The added cost of these agents during the 30-day period in this model would also be minimal, and events after the 48-h period would be attributable to the oral P2Y12 agent prescribed, which, in this study, is consistent across all patients. Moreover, the washout duration required with these agents is similar or longer than with clopidogrel.
The model also only quantified the cost consequences for CAD patients planned for PCI procedures and patients managed directly with CABG surgery, and excluded patients managed medically. Excluding these patients may have underestimated CAD events occurring during the model time horizon. Finally, several methodological assumptions were made to simplify model calculations used in lieu of available clinical trial or real-world data. Sensitivity analyses assessed the top 20 parameters and indicated that some of these assumptions are more impactful to the model results than others. Therefore, the exact impact of these inputs and assumptions is not certain, and further studies are needed to validate the results of this analysis.
6 Conclusion
The model presented in this study was used to study the cost consequences of using cangrelor in PCI patients with two or more angiographic HRFs and avoidance of P2Y12 inhibitor pretreatment in patients managed in hospital with CABG surgery. This analysis suggests having cangrelor available for use in PCI patients with two or more angiographic HRFs may be associated with improved clinical outcomes while providing potential savings to the hospital from fewer CAD events and minimizing P2Y12 inhibitor washout costs by decreasing pretreatment rates.
References
Collet JP, Thiele H, Barbato E, Barthelemy O, Bauersachs J, Bhatt DL, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021;42(14):1289–367.
Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011;58(24):e44-122.
Johnson TW, Mumford AD, Scott LJ, Mundell S, Butler M, Strange JW. A Study of Platelet Inhibition, Using a ‘Point of Care’ Platelet Function Test, following Primary Percutaneous Coronary Intervention for ST-Elevation Myocardial Infarction [PINPOINT-PPCI]. PLoS ONE. 2015;10(12):e0144984.
Kubica J, Adamski P, Ostrowska M, Sikora J, Kubica JM, Sroka WD. Morphine delays and attenuates ticagrelor exposure and action in patients with myocardial infarction: the randomized, double-blind, placebo-controlled IMPRESSION trial. Eur Heart J. 2016;37(3):245–52.
Silvain J, Storey RF, Cayla G, Esteve JB, Dillinger JG, Rousseau H. P2Y12 receptor inhibition and effect of morphine in patients undergoing primary PCI for ST-segment elevation myocardial infarction. The PRIVATE-ATLANTIC study. Thromb Haemost. 2016;116(2):369–78.
McEvoy JW, Ibrahim K, Kickler TS, Clarke WA, Hasan RK, Czarny MJ, et al. Effect of intravenous fentanyl on ticagrelor absorption and platelet inhibition among patients undergoing percutaneous coronary intervention. Circulation. 2018;137(3):307–9.
Goli RR, Ibrahim K, Shah R, Kickler TS, Clarke WA, Resar JR, et al. The dose and timing of fentanyl impacts on ticagrelor absorption and platelet inhibition during percutaneous coronary intervention: the PACIFY randomized clinical trial. J Invasive Cardiol. 2019;31(9):265–71.
PLAVIX (clopidogrel bisulfate) tablets, for oral use. 1997 May 2019. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/020839s070lbl.pdf. Accessed 30 July 2019
EFFIENT (prasugrel) tablets. 2009 September 2011. https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/022307s003lbl.pdf. Accessed 30 July 2019
BRILINTA (ticagrelor) tablets, for oral use. 2011 September 2016. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/022433s020lbl.pdf. Accessed 30 July 2019
Bhatt DL, Stone GW, Mahaffey KW, Gibson CM, Steg PG, Hamm CW. Effect of platelet inhibition with cangrelor during PCI on ischemic events. N Engl J Med. 2013;368(14):1303–13.
Bhatt DL, Lincoff AM, Gibson CM, Stone GW, McNulty S, Montalescot G. Intravenous platelet blockade with cangrelor during PCI. N Engl J Med. 2009;361(24):2330–41.
Harrington RA, Stone GW, McNulty S, White HD, Lincoff AM, Gibson CM. Platelet inhibition with cangrelor in patients undergoing PCI. N Engl J Med. 2009;361(24):2318–29.
Steg PG, Bhatt DL, Hamm CW, Stone GW, Gibson CM, Mahaffey KW. Effect of cangrelor on periprocedural outcomes in percutaneous coronary interventions: a pooled analysis of patient-level data. Lancet. 2013;382(9909):1981–92.
Vaduganathan M, Harrington RA, Stone GW, Steg PG, Gibson CM, Hamm CW, et al. Variation in patient profiles and outcomes in US and non-US subgroups of the cangrelor versus standard therapy to achieve optimal management of platelet inhibition (CHAMPION) PHOENIX trial. Circ Cardiovasc Interv. 2016;9(6):e003612-e.
Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–77.
Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40(2):87–165.
Stone GW, Genereux P, Harrington RA, White HD, Gibson CM, Steg PG, et al. Impact of lesion complexity on peri-procedural adverse events and the benefit of potent intravenous platelet adenosine diphosphate receptor inhibition after percutaneous coronary intervention: core laboratory analysis from 10 854 patients from the CHAMPION PHOENIX trial. Eur Heart J. 2018;39(46):4112–21.
Cavender M, Harrington R, Stone G, Deliargyris E, Steg P, Gibson C. Ischemic events occur early in patients undergoing PCI and are reduced with cangrelor: findings from CHAMPION PHOENIX. J Am Coll Cardiol. 2017;69(11 Suppl):25.
Cavender MA, Bhatt DL, Stone GW, White HD, Steg PG, Gibson CM, et al. Consistent reduction in periprocedural myocardial infarction with cangrelor as assessed by multiple definitions: findings from CHAMPION PHOENIX (cangrelor versus standard therapy to achieve optimal management of platelet inhibition). Circulation. 2016;134(10):723–33.
Jatene T, Harrington RA, Stone GW, Steg PG, Gibson CM, Hamm CW, et al. Investigator-reported bleeding versus post hoc adjudication of bleeding: lessons from the CHAMPION PHOENIX trial. J Am Coll Cardiol. 2016;67(5):596–8.
Qamar A, Bhatt DL. Optimizing the use of cangrelor in the real world. Am J Cardiovasc Drugs. 2017;17(1):5–16.
Stone GW, McLaurin BT, Cox DA, Bertrand ME, Lincoff AM, Moses JW. Bivalirudin for patients with acute coronary syndromes. N Engl J Med. 2006;355(21):2203–16.
Badri M, Abdelbaky A, Li S, Chiswell K, Wang TY. Precatheterization use of P2Y12 inhibitors in non-ST-elevation myocardial infarction patients undergoing early cardiac catheterization and in-hospital coronary artery bypass grafting: insights from the National Cardiovascular Data Registry®. J Am Heart Assoc. 2017;6(9):e006508.
Vaduganathan M, Harrington RA, Stone GW, Deliargyris EN, Steg PG, Gibson CM. Evaluation of ischemic and bleeding risks associated with 2 parenteral antiplatelet strategies comparing cangrelor with glycoprotein IIb/IIIa inhibitors: an exploratory analysis from the CHAMPION trials. JAMA Cardiol. 2017;2(2):127–35.
Mehran R, Rao SV, Bhatt DL, Gibson CM, Caixeta A, Eikelboom J, et al. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation. 2011;123(23):2736–47.
Ben Morrison T, Horst BM, Brown MJ, Bell MR, Daniels PR. Bridging with glycoprotein IIb/IIIa inhibitors for periprocedural management of antiplatelet therapy in patients with drug eluting stents. Catheter Cardiovasc Interv. 2012;79(4):575–82.
Dressler R, Dryer MM, Coletti C, Mahoney D, Doorey AJ. Altering overuse of cardiac telemetry in non-intensive care unit settings by hardwiring the use of American Heart Association guidelines. JAMA Intern Med. 2014;174(11):1852–4.
Bureau of Labor Statistics. Medical Care Consumer Price Index. 2018. http://www.bls.gov/data/. Accessed 30 Aug 2019
AnalySource Database. 2019. https://www.analysource.com/. Accessed 30 Oct 2019
Vaduganathan M, Harrington RA, Stone GW, Deliargyris EN, Steg PG, Gibson CM, et al. Cangrelor with and without glycoprotein IIb/IIIa inhibitors in patients undergoing percutaneous coronary intervention. J Am Coll Cardiol. 2017;69(2):176–85.
US Centers for Medicare & Medicaid Services. Outcome Measures. 2018. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/OutcomeMeasures.html. Accessed 5 Sep 2019
Franchi F, Rollini F, Rivas A, Wali M, Briceno M, Agarwal M, et al. Platelet inhibition with cangrelor and crushed ticagrelor in patients with ST-s. Circulation. 2019;139(14):1661–70.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Availability of data and material
The assumptions used for the model are all from published sources and referenced throughout the manuscript. The results from the model are reported in the tables. No other data or materials are available from this analysis.
Funding
This manuscript was funded by Chiesi, Inc. The authors approved all content and results reported in this manuscript.
Conflict of interest
Ivar S. Jensen, Elizabeth Wu, and Philip L. Cyr are employees of PrecisionHEOR, which provides consulting services to the pharmaceutical industry, including Chiesi, Inc. Marc Claussen and Khalid Salahuddin are employees of Chiesi, Inc.; Thomas Winkler was an employee of Chiesi at the time of developing this analysis; and Jayne Prats is a consultant to Chiesi, Inc. Kenneth W. Mahaffey’s financial disclosures can be viewed at http://med.stanford.edu/profiles/kenneth-mahaffey. C. Michael Gibson receives research support and consulting fees from Janssen and Johnson & Johnson, and also receives consulting fees from Bayer. Gabriel Steg discloses the following relationships: research grant from Amarin, Bayer, Sanofi, and Servier, and speaking or consulting fees from Amarin, Amgen, AstraZeneca, Bayer/Janssen, Boehringer-Ingelheim, Bristol-Myers-Squibb, Chiesi, Idorsia, Myokardia, Novartis, Novo-Nordisk, Pfizer, Regeneron, Sanofi, Servier, and The Medicines Company. Gregg W. Stone has received speaker or other honoraria from Cook, Terumo, QOOL Therapeutics, and Orchestra Biomed, and has served as a consultant to Valfix, TherOx, Vascular Dynamics, Robocath, HeartFlow, Gore, Ablative Solutions, Miracor, Neovasc, V-Wave, Abiomed, Ancora, and MAIA. Deepak L. Bhatt discloses the following relationships: Advisory Board: Cardax, CellProthera, Cereno Scientific, Elsevier Practice Update Cardiology, Janssen, Level Ex, Medscape Cardiology, MyoKardia, NirvaMed, Novo Nordisk, PhaseBio, PLx Pharma, and Regado Biosciences; Board of Directors: Boston VA Research Institute, Society of Cardiovascular Patient Care, and TobeSoft; Chair: American Heart Association Quality Oversight Committee; Data Monitoring Committees: Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute, for the PORTICO trial, funded by St. Jude Medical, now Abbott), Cleveland Clinic (including for the ExCEED trial, funded by Edwards), Contego Medical (Chair, PERFORMANCE 2), Duke Clinical Research Institute, Mayo Clinic, Mount Sinai School of Medicine (for the ENVISAGE trial, funded by Daiichi Sankyo), and Population Health Research Institute; Honoraria: American College of Cardiology (Senior Associate Editor, Clinical Trials and News, ACC.org; Chair, ACC Accreditation Committee), Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute; RE-DUAL PCI Clinical Trial Steering Committee funded by Boehringer Ingelheim; AEGIS-II executive committee funded by CSL Behring), Belvoir Publications (Editor in Chief, Harvard Heart Letter), Canadian Medical and Surgical Knowledge Translation Research Group (Clinical Trial Steering Committees), Duke Clinical Research Institute (Clinical Trial Steering Committees, including for the PRONOUNCE trial, funded by Ferring Pharmaceuticals), HMP Global (Editor in Chief, Journal of Invasive Cardiology), Journal of the American College of Cardiology (Guest Editor, Associate Editor), K2P (Co-Chair, interdisciplinary curriculum), Level Ex, Medtelligence/ReachMD (CME steering committees), MJH Life Sciences, Population Health Research Institute (for the COMPASS Operations Committee, Publications Committee, Steering Committee, and USA national co-leader, funded by Bayer), Slack Publications (Chief Medical Editor, Cardiology Today’s Intervention), Society of Cardiovascular Patient Care (Secretary/Treasurer), WebMD (CME Steering Committees); Other: Clinical Cardiology (Deputy Editor), NCDR-ACTION Registry Steering Committee (Chair), VA CART Research and Publications Committee (Chair); Research Funding: Abbott, Afimmune, Amarin, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Cardax, CellProthera, Cereno Scientific, Chiesi, CSL Behring, Eisai, Ethicon, Ferring Pharmaceuticals, Forest Laboratories, Fractyl, Garmin, HLS Therapeutics, Idorsia, Ironwood, Ischemix, Janssen, Lexicon, Lilly, Medtronic, MyoKardia, NirvaMed, Novartis, Novo Nordisk, Owkin, Pfizer, PhaseBio, PLx Pharma, Regeneron, Roche, Sanofi, Synaptic, The Medicines Company, and 89Bio; Royalties: Elsevier (Editor, Cardiovascular Intervention: A Companion to Braunwald’s Heart Disease); Site Co-Investigator: Abbott, Biotronik, Boston Scientific, CSI, St. Jude Medical (now Abbott), Svelte; Trustee: American College of Cardiology; and Unfunded Research: FlowCo, Merck, Takeda.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Author contributions
ISJ, EW: Conceptualization, methodology, model programming, writing, review, and editing. PLC, MC, TW, KS, JP: Conceptualization, methodology, validation, writing, review and editing. KWM, CMG, GS, GWS, and DLB: Validation, writing, review, and editing.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Jensen, I.S., Wu, E., Cyr, P.L. et al. Cost-Consequence Analysis of Using Cangrelor in High Angiographic Risk Percutaneous Coronary Intervention Patients: A US Hospital Perspective. Am J Cardiovasc Drugs 22, 93–104 (2022). https://doi.org/10.1007/s40256-021-00491-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-021-00491-9