Abstract
Purpose
To develop a non-contrast computed tomography-(CT)-based radiomics score for predicting the risk of hematoma early enlargement in spontaneous intracerebral hemorrhage.
Methods
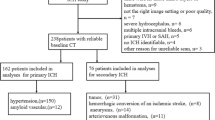
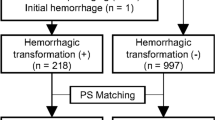
A total of 258 patients from a single-center database with acute spontaneous intracerebral parenchymal hemorrhage were collected. Radiomics software was explored to segment hematomas on baseline non-contrast CT images, and the texture features were extracted. Minimal Redundancy and Maximal Relevance (mRMR) and Least Absolute Shrinkage and Selection Operator (LASSO), were used to select optimized subset of features and radiomics score was calculated. The radiomics model (radiomics score-based), radiomics nomogram (radiomics score combined with clinical factors-based) and clinical model (clinical factors-based) were built in a training cohort and validated in a test cohort. The discrimination, calibration, and clinical usefulness of the models were evaluated. Finally, a subgroup analysis was performed to assess the predictive value of radiomics score in specific hemorrhage location.
Results
Radiomics score was composed of 12 radiomics features. The radiomics model and radiomics nomogram both showed good performance in predicting hematoma enlargement (area under the curve, AUC 0.83 [0.71–0.95], AUC 0.82 [0.72, 0.93]), and were both better than clinical model (AUC 0.66 [0.54–0.79]). The radiomics model and radiomics nomogram showed satisfactory calibration and clinical usefulness for detecting hematoma enlargement. For subgroup analysis, radiomics score also showed good predictive value for hematoma enlargement in different locations (AUC were 0.828, 0.940, 0.836 and 0.904, respectively, for supratentorial, subtentorial, deep and lobes).
Conclusion
A radiomics score based on non-contrast CT may be considered as a potential biomarker for prediction of hematoma enlargement in patients with spontaneous intracerebral hemorrhage (SICH), and it presented a high incremental value to clinical factors for hematoma enlargement prediction.









Similar content being viewed by others
References
Hemphill JC 3rd, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, Fung GL, Goldstein JN, Macdonald RL, Mitchell PH, Scott PA, Selim MH, Woo D; American Heart Association Stroke Council; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology. Guidelines for the Management of Spontaneous Intracerebral Hemorrhage: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2015;46:2032–60.
Fewel ME, Thompson BG Jr, Hoff JT. Spontaneous intracerebral hemorrhage: a review. Neurosurg Focus. 2003;15:E1.
Davis SM, Broderick J, Hennerici M, Brun NC, Diringer MN, Mayer SA, Begtrup K, Steiner T; Recombinant Activated Factor VII Intracerebral Hemorrhage Trial Investigators. Hematoma growth is a determinant of mortality and poor outcome after intracerebral hemorrhage. Neurology. 2006;66:1175–81.
Brott T, Broderick J, Kothari R, Barsan W, Tomsick T, Sauerbeck L, Spilker J, Duldner J, Khoury J. Early hemorrhage growth in patients with intracerebral hemorrhage. Stroke. 1997;28:1–5.
Cucchiara B, Messe S, Sansing L, Kasner S, Lyden P. Hematoma growth in oral anticoagulant related intracerebral hemorrhage. Stroke. 2008;39:2993–6.
Zhang D, Chen J, Guo J, Jiang Y, Dong Y, Ping-Chi Chen B, Wang J, Hou L. Hematoma Heterogeneity on Noncontrast Computed Tomography Predicts Intracerebral Hematoma Expansion: A Meta-Analysis. World Neurosurg. 2018;114:e663–76.
Li Q, Liu QJ, Yang WS, Wang XC, Zhao LB, Xiong X, Li R, Cao D, Zhu D, Wei X, Xie P. Island Sign: An Imaging Predictor for Early Hematoma Expansion and Poor Outcome in Patients With Intracerebral Hemorrhage. Stroke. 2017;48:3019–25.
Yu Z, Zheng J, He M, Guo R, Ma L, You C, Li H. Accuracy of swirl sign for predicting hematoma enlargement in intracerebral hemorrhage: a meta-analysis. J Neurol Sci. 2019;399:155–60.
Yu Z, Zheng J, Ma L, Guo R, Li M, Wang X, Lin S, Li H, You C. The predictive accuracy of the black hole sign and the spot sign for hematoma expansion in patients with spontaneous intracerebral hemorrhage. Neurol Sci. 2017;38:1591–7.
Wang X, Arima H, Al-Shahi Salman R, Woodward M, Heeley E, Stapf C, Lavados PM, Robinson T, Huang Y, Wang J, Delcourt C, Anderson CS; INTERACT Investigators. Clinical prediction algorithm (BRAIN) to determine risk of hematoma growth in acute intracerebral hemorrhage. Stroke. 2015;46:376–81.
Al-Shahi Salman R, Frantzias J, Lee RJ, Lyden PD, Battey TWK, Ayres AM, Goldstein JN, Mayer SA, Steiner T, Wang X, Arima H, Hasegawa H, Oishi M, Godoy DA, Masotti L, Dowlatshahi D, Rodriguez-Luna D, Molina CA, Jang DK, Davalos A, Castillo J, Yao X, Claassen J, Volbers B, Kazui S, Okada Y, Fujimoto S, Toyoda K, Li Q, Khoury J, Delgado P, Sabín JÁ, Hernández-Guillamon M, Prats-Sánchez L, Cai C, Kate MP, McCourt R, Venkatasubramanian C, Diringer MN, Ikeda Y, Worthmann H, Ziai WC, d’Esterre CD, Aviv RI, Raab P, Murai Y, Zazulia AR, Butcher KS, Seyedsaadat SM, Grotta JC, Martí-Fàbregas J, Montaner J, Broderick J, Yamamoto H, Staykov D, Connolly ES, Selim M, Leira R, Moon BH, Demchuk AM, Di Napoli M, Fujii Y, Anderson CS, Rosand J; VISTA-ICH Collaboration; ICH Growth Individual Patient Data Meta-analysis Collaborators. Absolute risk and predictors of the growth of acute spontaneous intracerebral haemorrhage: a systematic review and meta-analysis of individual patient data. Lancet Neurol. 2018;17:885–94. Erratum in: Lancet Neurol. 2018 Sep 19
Morotti A, Dowlatshahi D, Boulouis G, Al-Ajlan F, Demchuk AM, Aviv RI, Yu L, Schwab K, Romero JM, Gurol ME, Viswanathan A, Anderson CD, Chang Y, Greenberg SM, Qureshi AI, Rosand J, Goldstein JN; ATACH-II, NETT, and PREDICT Investigators. Predicting Intracerebral Hemorrhage Expansion With Noncontrast Computed Tomography: The BAT Score. Stroke. 2018;49:1163–9. Erratum in: Stroke. 2018;49:e297.
Lambin P, Rios-Velazquez E, Leijenaar R, Carvalho S, van Stiphout RG, Granton P, Zegers CM, Gillies R, Boellard R, Dekker A, Aerts HJ. Radiomics: extracting more information from medical images using advanced feature analysis. Eur J Cancer. 2012;48:441–6.
Aerts HJ, Velazquez ER, Leijenaar RT, Parmar C, Grossmann P, Carvalho S, Bussink J, Monshouwer R, Haibe-Kains B, Rietveld D, Hoebers F, Rietbergen MM, Leemans CR, Dekker A, Quackenbush J, Gillies RJ, Lambin P. Decoding tumour phenotype by noninvasive imaging using a quantitative radiomics approach. Nat Commun. 2014;5:4006. Erratum in: Nat Commun. 2014;5:4644.
Gillies RJ, Kinahan PE, Hricak H. Radiomics: images are more than pictures, they are data. Radiology. 2016;278:563–77.
Brouwers HB, Chang Y, Falcone GJ, Cai X, Ayres AM, Battey TW, Vashkevich A, McNamara KA, Valant V, Schwab K, Orzell SC, Bresette LM, Feske SK, Rost NS, Romero JM, Viswanathan A, Chou SH, Greenberg SM, Rosand J, Goldstein JN. Predicting hematoma expansion after primary intracerebral hemorrhage. JAMA Neurol. 2014;71:158–64.
Huynh TJ, Aviv RI, Dowlatshahi D, Gladstone DJ, Laupacis A, Kiss A, Hill MD, Molina CA, Rodriguez-Luna D, Dzialowski I, Silva Y, Kobayashi A, Lum C, Boulanger JM, Gubitz G, Bhatia R, Padma V, Roy J, Kase CS, Symons SP, Demchuk AM; PREDICT/Sunnybrook CTA Investigators. Validation of the 9-Point and 24-Point Hematoma Expansion Prediction Scores and Derivation of the PREDICT A/B Scores. Stroke. 2015;46:3105–10.
Huang YQ, Liang CH, He L, Tian J, Liang CS, Chen X, Ma ZL, Liu ZY. Development and Validation of a Radiomics Nomogram for Preoperative Prediction of Lymph Node Metastasis in Colorectal Cancer. J Clin Oncol. 2016;34:2157–64. Erratum in: J Clin Oncol. 2016;34:2436.
Li H, Xie Y, Wang X, Chen F, Sun J, Jiang X. Radiomics features on non-contrast computed tomography predict early enlargement of spontaneous intracerebral hemorrhage. Clin Neurol Neurosurg. 2019;185:105491.
Duan C, Chaovalitwongse WA, Bai F, Hippe DS, Wang S, Thammasorn P, Pierce LA, Liu X, You J, Miyaoka RS, Vesselle HJ, Kinahan PE, Rengan R, Zeng J, Bowen SR. Sensitivity analysis of FDG PET tumor voxel cluster radiomics and dosimetry for predicting mid-chemoradiation regional response of locally advanced lung cancer. Phys Med Biol. 2020;65:205007.
Ekert K, Hinterleitner C, Baumgartner K, Fritz J, Horger M. Extended Texture Analysis of Non-Enhanced Whole-Body MRI Image Data for Response Assessment in Multiple Myeloma Patients Undergoing Systemic Therapy. Cancers (Basel). 2020;12:761.
Lovinfosse P, Polus M, Van Daele D, Martinive P, Daenen F, Hatt M, Visvikis D, Koopmansch B, Lambert F, Coimbra C, Seidel L, Albert A, Delvenne P, Hustinx R. FDG PET/CT radiomics for predicting the outcome of locally advanced rectal cancer. Eur J Nucl Med Mol Imaging. 2018;45:365–75.
Ito H, Maeda M, Uehara T, Yamamoto S, Tamura M, Takashima T. Attenuation values of chronic subdural haematoma and subdural effusion in CT scans. Acta Neurochir (Wien). 1984;72:211–7.
Stein J, Huerta K. When looking at a non-contrast head CT, what actually appears white in an acute hemorrhagic stroke? Cal J Emerg Med. 2002;3:70–1.
Xiong X, Li Q, Yang WS, Wei X, Hu X, Wang XC, Zhu D, Li R, Cao D, Xie P. Comparison of Swirl Sign and Black Hole Sign in Predicting Early Hematoma Growth in Patients with Spontaneous Intracerebral Hemorrhage. Med Sci Monit. 2018;24:567–73.
He GN, Guo HZ, Han X, Wang EF, Zhang YQ. Comparison of CT black hole sign and other CT features in predicting hematoma expansion in patients with ICH. J Neurol. 2018;265:1883–90.
Xu W, Ding Z, Shan Y, Chen W, Feng Z, Pang P, Shen Q. A Nomogram Model of Radiomics and Satellite Sign Number as Imaging Predictor for Intracranial Hematoma Expansion. Front Neurosci. 2020;14:491.
Ma C, Zhang Y, Niyazi T, Wei J, Guocai G, Liu J, Liang S, Liang F, Yan P, Wang K, Jiang C. Radiomics for predicting hematoma expansion in patients with hypertensive intraparenchymal hematomas. Eur J Radiol. 2019;115:10–5.
Flaherty ML, Haverbusch M, Sekar P, Kissela B, Kleindorfer D, Moomaw CJ, Sauerbeck L, Schneider A, Broderick JP, Woo D. Long-term mortality after intracerebral hemorrhage. Neurology. 2006;66:1182–6.
Naidech AM, Jovanovic B, Liebling S, Garg RK, Bassin SL, Bendok BR, Bernstein RA, Alberts MJ, Batjer HH. Reduced platelet activity is associated with early clot growth and worse 3-month outcome after intracerebral hemorrhage. Stroke. 2009;40:2398–401.
Sansing LH, Messe SR, Cucchiara BL, Cohen SN, Lyden PD, Kasner SE; CHANT Investigators. Prior antiplatelet use does not affect hemorrhage growth or outcome after ICH. Neurology. 2009;72:1397–402.
Emiru T, Bershad EM, Zantek ND, Datta YH, Rao GH, Hartley EW, Divani AA. Intracerebral hemorrhage: a review of coagulation function. Clin Appl Thromb Hemost. 2013;19:652–62.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
H. Li, Y. Xie, H. Liu and X. Wang declare that they have no competing interests.
Ethical standards
For this article no studies with human participants or animals were performed by any of the authors. All studies performed were in accordance with the ethical standards indicated in each case. The study was approved by the local medical ethics committee of Wuhan Central Hospital (NO.[2021]013). This study was a retrospective research and the informed consent was waived.
Funding
This work was supported by a fund from Wuhan Municipal Health Commission (WX21B15).
Additional information
Hui Li and Yuanliang Xie contributed equally to this work.
Appendix
Appendix
Appendix A1: The Process of Building Radiomics Score Formula
The baseline brain NCCT images of all cases were exported from picture archiving and communication system (PACS) with a uniform window position of 35 HU and a window width of 90 HU and imported into the radiomics software. Each hematoma on the image was segmented layer by layer by semi-automatic segmentation method to obtain a three-dimensional volume of interest (VOI) of hematoma, and texture features of three-dimensional VOI calculated by software were saved.
Two feature selection methods, mRMR and LASSO were used to select features. At first, mRMR was performed to eliminate the redundant and irrelevant features, 30 features were retained. Then the LASSO algorithm was used to choose the regular parameter λ and determine the number of the feature, the 10-fold cross-validation was adopted to avoid overfitting. The most predictive subset of feature was chosen, and the corresponding coefficients were evaluated. Radiomics score formula was generated using the selected features according to the formula as follows: radiomics score = (∑βi * Xi) + Intercept (i = 0, 1, 2, 3 …) Where Xi represented the ith selected feature and βi was its coefficient.
Appendix A2: The Process of Models Construction, Calibration and Validation
All patients were randomly divided into training cohort and test cohort according to the ratio of 7:3, models were established in the training cohort and then validated by test cohort. Three models were established: radiomics model (radiomics score-based), clinical model (clinical factors-based) and radiomics nomogram (radiomics score combined with clinical factors-based).
Model Construction
Radiomics Model
HE or non-HE was used as dichotomy criterion, The predictive model based on radiomics scores was built in training cohort using the following univariate logistic regression equations: logit πradiomics score = 0.457 + 1.537 × radiomics score.
Clinical Model
For clinical factors, we adopted univariate and multivariate logistic regression analysis to screen independent risk factors. Then, multivariate logistic regression model based on independent clinical risk factors was constructed in training cohort.
Radiomics Nomogram
Based on radiomics score and independent clinical risk factors, we established a radiomics nomogram to predict HE in training cohort.
Models Calibration
Discrimination
The ROC curves were plotted and the AUCs under ROCs were used to evaluate the performances of radiomics model, clinical model and radiomics nomogram in discriminating patients with HE from those with non-HE in training cohort.
Calibration
Hosmer-Lemeshow test was performed to test the calibration and decision curve analysis (DCA) to evaluate the clinical net benefit of the models in training cohort.
Model Validation
Radiomics model, clinical model and radiomics nomogram established in training cohort were introduced into test cohort to validate and the same process as training cohort of performances assessment with the ROC analysis and the calibration curve were also carried out in test cohort.
Appendix A3: The Radiomics Score Formula
Rights and permissions
About this article
Cite this article
Li, H., Xie, Y., Liu, H. et al. Non-Contrast CT-Based Radiomics Score for Predicting Hematoma Enlargement in Spontaneous Intracerebral Hemorrhage. Clin Neuroradiol 32, 517–528 (2022). https://doi.org/10.1007/s00062-021-01062-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-021-01062-w