Abstract
Introduction
Although the pneumococcal conjugate vaccine (PCV) has been introduced into select state immunization programs (SIPs) in India, many children remain unvaccinated. Recently, India’s Advisory Committee on Vaccines & Immunization Practices recommended PCV on the pediatric immunization schedule nationally. This study estimates the public health and economic impact of introducing either Pfizer’s 13-valent PCV (PCV13-PFE), GlaxoSmithKline’s 10-valent PCV (PCV10-GSK), or Serum Institute of India’s 10-valent PCV (PCV10-SII) into every pediatric SIP.
Methods
A model was developed to predict the disease cases, deaths, and costs associated with implementing PCV13-PFE, PCV10-GSK, or PCV10-SII in SIPs compared to no vaccination program across a 5-year period (2021–2025). State and national-level uptake rate and clinical and economic input parameters were collected from published literature. Disease outcomes included invasive pneumococcal disease, inpatient and outpatient pneumonia, and otitis media. Costs were estimated as vaccine-related costs and direct medical costs incurred to the healthcare system. Results were reported by individual state and aggregated nationally.
Results
Estimated over 5 years, implementing PCV13-PFE in SIPs could avert 12.1 million cases and save 626,512 lives among children under 5 years old compared to no vaccination. This corresponds to net national cost savings of over $1.0 billion. Both lower-valent PCVs are estimated to provide less economic savings than PCV13-PFE inclusive of vaccine-related costs. Compared with PCV13-PFE, implementing PCV10-GSK or PCV10-SII nationally is estimated to have a smaller public health impact, with PCV10-GSK averting 8.4 million cases (436,577 deaths) and PCV10-SII preventing 10.3 million cases (531,545 deaths) in India compared to no vaccination, respectively.
Conclusion
Implementation of PCV13-PFE throughout India is estimated to provide greater public health and economic benefits than PCV10-GSK or PCV10-SII SIPs. Our analysis highlights the substantial disease cases, deaths, and health system cost savings that may be realized from implementing PCV programs throughout India.
Similar content being viewed by others
Why carry out this study? |
India alone accounted for approximately 20% of all under-five deaths from pneumococcal disease globally in 2015. In efforts to address this, the 13-valent pneumococcal conjugate vaccine (PCV13-PFE) was introduced into select state immunization programs (SIPs) in 2017 and other lower-valent PCVs, PCV10-GSK and PCV10-SII, have been licensed for use. |
However, PCVs are not included in most SIPs and therefore decision-makers may be undervaluing the true public health and economic impact of pneumococcal disease prevention. We sought to estimate the public health and economic impact of introducing each of the three available PCVs among children under 5 years old in all of India’s SIPs. |
What was learned from the study? |
Implementing PCV SIPs throughout India would not only prevent a substantial amount of pneumococcal disease cases and consequent deaths but also lead to cost savings for the health system. |
Country-wide PCV13-PFE vaccination is estimated to provide a greater public health and economic impact than PCV10-GSK or PCV10-SII; thus, India should consider expanding access to PCV13-PFE in remaining SIPs. |
Introduction
Streptococcus pneumoniae (S. pneumoniae) infection can lead to non-invasive disease such as otitis media (OM) and non-bacteremic pneumonia, or invasive pneumococcal disease (IPD) including meningitis, bacteremia, and bacteremic pneumonia [1]. Diseases caused by S. pneumoniae are a leading cause of childhood morbidity and mortality worldwide, with the highest disease burden in Africa and Asia [1,2,3]. In 2015, India alone accounted for approximately 20% of all under-five deaths from pneumococcal disease globally [3, 4]. Pneumonia is estimated to be a leading cause of child mortality in India, responsible for 30.6% of postnatal deaths in children under 5 years old [5]. More specifically, an estimated 68,700 children under 5 years old were predicted to have died from S. pneumoniae infection nationally in 2015 [6].
In 2000, the first pneumococcal conjugate vaccine (PCV), a 7-valent pneumococcal conjugate vaccine (PCV7), was licensed and approved for use in children. This vaccine protected against seven of the most common pneumococcal disease-causing serotypes (4, 6B, 9V, 14, 18C, 19F, 23F). In 2009, two higher valent PCVs were licensed for use around the world, a 10-valent vaccine (PCV10-GSK; Synflorix™, GlaxoSmithKline) containing the PCV7 serotypes plus serotypes 1, 5, and 7F, and a 13-valent vaccine (PCV13-PFE; Prevenar13™, Pfizer), containing PCV10-GSK serotypes plus serotypes 3, 6A, and 19A. Over the last 10 years, PCV10-GSK and PCV13-PFE have demonstrated a substantial public health impact in reducing pneumococcal disease globally [7,8,9]. As a result of routine PCV infant immunization in many countries, pneumococcal deaths among children younger than 5 years old decreased between 2000 and 2015 by 51% worldwide [3].
Recently, another 10-valent vaccine (PCV10-SII; Pneumosil™, Serum Institute of India) received World Health Organization pre-qualification (WHO-PQ) and was licensed in India in 2020 following safety and immunogenicity clinical trials and a single noninferiority study compared to PCV10-GSK [10, 11]. In contrast to PCV13-PFE, PCV10-SII does not contain serotypes 3, 4, and 18C in its formulation. Unlike established PCVs, PCV10-SII has yet to demonstrate real-world effectiveness against pneumococcal disease or nasopharyngeal carriage of S. pneumoniae. Additionally, PCV10-SII is currently only indicated for use in children under 2 years old with a 3 + 1 or 3 + 0 schedule [10], differing from PCV10-GSK and PCV13-PFE which are additionally indicated for use in a 2 + 1 infant schedule and in children up to 5 years old and for all ages, respectively.
In 2016, the Government of India, Ministry of Health and Family Welfare, and Gavi, the Vaccine Alliance (Gavi), developed a plan to include PCVs into state immunization programs (SIPs) for all of India’s states and union territories [4]. With support from Gavi, the vaccine would be offered in phases beginning in 2017. States with the highest burden of pneumonia (Bihar, Himachal Pradesh, Madhya Pradesh, Rajasthan, and Uttar Pradesh) were first to introduce a PCV SIP, and Haryana soon followed with a state-funded program [12, 13]. In 2020, Goa secured support from the United Nations Children’s Fund (UNICEF) to implement their own state-level PCV program [14]. Despite these ambitious efforts, further scale-up to other SIPs has halted. As of 2021, most of India’s 36 states and union territories do not have a SIP and a large cohort of children under 5 years old remain at risk of pneumococcal disease. The Indian Academy of Pediatrics (IAP) Advisory Committee on Vaccines and Immunization Practices (ACVIP) has released new recommendations for vaccine introductions that include PCV, in an effort to continue progress for greater access and uptake nationally [15, 16].
According to a study by Farooqui et al. (2015), pneumococcal disease incidence rates vary substantially across states in India [17]. States with weaker healthcare infrastructure and socioeconomic status, such as Uttar Pradesh, Bihar, Madhya Pradesh, and Rajasthan, have higher incidence of severe pneumonia in children under 5 years old. In contrast, states where access to healthcare is stronger, including Kerala, Tamil Nadu, Sikkim, and Manipur, have lower incidence of pneumonia. A universal immunization program (UIP) in India would help improve social equity for children living in impoverished communities by providing access among the poorest of the population.
Given the dynamic PCV landscape and the varying disease burden in India, it is critical to estimate the public health and economic impact of PCV13-PFE, PCV10-GSK, or PCV10-SII implementation by state and union territory. However, previous studies have estimated the effect of introducing PCV13-PFE in India nationally or in select states. Ghia et al. (2018) estimated that a PCV13-PFE national immunization program (NIP) with an uptake rate of only 25% would avert approximately 1.9 million pneumococcal disease cases and 77,000 deaths in children under 5 years old annually [18]. Constenla and Liu (2019) modeled the impact of implementing PCV13-PFE both nationally and in four states, Bihar, Maharashtra, Tamil Nadu, and New Delhi [19]. Assuming a national vaccine uptake of 72%, the authors found that PCV13-PFE implementation could prevent 716,891 cases and 25,796 deaths in children under 5 years old and save $309.8 million in direct and indirect costs over 1 year in India. Most recently, Krishnamoorthy et al. (2019) published a cost-effectiveness analysis that found that over 10 years, a PCV13-PFE NIP is highly cost-effective from the government perspective at a cost of US $467 per disability-adjusted life year averted [20]. Thus, the objective of this study is to calculate the public health and economic impact of introducing the three PCVs currently licensed in India into every state and union territory’s immunization program in the country.
Methods
Model Structure
We expanded upon a previously developed decision analytic model created in Microsoft Excel to estimate the public health and economic impact of including either PCV13-PFE, PCV10-GSK, or PCV10-SII in immunization programs at state and national levels [21, 22]. The 35 states and union territories (cumulatively simplified to the term “states” for the remainder of this analysis) included in the study were those that were established at the time of the analysis.Footnote 1 The model estimated pneumococcal disease cases and deaths averted, and costs associated with implementing each PCV in every SIP compared to no vaccination for a birth cohort in India. All three vaccine programs assumed infants under 1 year old received the full schedule and we did not account for differences in dose timing because the model was based on full year cohorts. The cohort had a probability of transitioning to one of the following mutually exclusive health outcomes: no disease, IPD (including bacteremia and meningitis), community-acquired pneumonia (either inpatient or outpatient), or OM. If IPD or inpatient pneumonia was experienced, the health state carried the risk of death. Unlike previous iterations of this model, this version includes a time horizon of 5 years (2021–2025) and accounts for a scaled implementation of the UIP and SIPs over the 5-year period. Following calculations of disease cases and deaths, direct costs incurred from the healthcare system perspective were reported. Finally, this decision analytic model is informed by previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Epidemiological Inputs
State-specific population estimates for children under 5 years old were derived from the Government of India’s 2011 census along with an annual state population growth rate to forecast future birth cohort sizes (Supplementary Table S1) [23]. Immunization uptake rates were based on estimates of third dose of diphtheria, pertussis, tetanus (DPT3) vaccine coverage by state from UNICEF’s National Factsheet Coverage Evaluation Survey [24]. It was assumed that each state would take 3 years for coverage levels of PCV13-PFE to equal that of DPT3 based on a linear growth rate, after which vaccination coverage would remain constant until the end of the study period (Supplementary Table S1). The six states that introduced PCVs into their SIPs in 2017/18 were assumed to have PCV uptake equal to DPT3 coverage levels already in the first year.Footnote 2
The national IPD incidence rate and state-specific inpatient pneumonia incidence rates among children younger than 5 years were sourced from Farooqui et al. (2015) [17]. Inpatient pneumonia categorized as severe in the study was based on the prevalence of risk factors associated with fatality. The average national incidence was assumed for union territories that did not have specific incidence data on inpatient pneumonia (Supplementary Table S1).Footnote 3 State-specific outpatient pneumonia incidence rates were estimated by assuming a 30:70 ratio between severe and non-severe pneumonia based on nationally reported incidence in Rudan et al. (2013) [25]. Another study by Wahl et al. (2020) reported significantly higher state-specific pneumonia incidence rates [26]. Both studies derived state-specific incidence using mathematical models and therefore data were not observational regional surveillance estimates. Given the similarities between the two studies, we took a conservative approach and included lower estimates for pneumonia reported by Farooqui et al. (2015) for base case calculations. Uncertainty associated with this input parameter was tested in a scenario analyses using estimates from Wahl et al. (2020). OM incidence rate was from a prospective community-based hospital study in Vellore of 210 unvaccinated infants born in 2009, and estimated to be 29,000 per 100,000 children under 5 years old [27].
The IPD case fatality rate was based on a study by Thomas et al. (1999) that examined the properties of invasive pneumonia infections and deaths over the course of 4 years in a prospective hospital-based study in India. They reported case fatality rates of 21% and 34% for bacteremia and meningitis, respectively [28]. We assumed that 80% of IPD occurs as a result of bacteremia and 20% occurs as a result of meningitis and weighted our overall IPD case fatality rate accordingly [18]. The inpatient pneumonia case fatality rate was calculated with the mortality and severe pneumonia incidence reported in Rudan et al. (2013), resulting in an estimate of 17.2% [25]. It was assumed that there was no risk of death associated with outpatient pneumonia or OM (Table 1).
PCV10-GSK, PCV10-SII, and PCV13-PFE serotype coverage was derived from a hospital-based surveillance study in south India [29]. In their study, Nisarga et al. (2015) reported serotype coverage for PCV10-GSK, PCV10-SII, and PCV13-PFE to be 63.9%, 77.8%, and 91.7%, respectively. It was assumed that the serotype distribution for non-invasive pneumococcal disease was the same as IPD.
Vaccine Effectiveness
Because clinical trial data exist for efficacy of PCV7 against IPD, we adjusted PCV7 efficacy for the additional serotypes covered in PCV10-GSK, PCV10-SII, and PCV13-PFE. The reported efficacy of PCV7 (94% against vaccine covered serotypes [30]) was applied to the proportion of serotypes covered by each of the PCVs to estimate their vaccine effectiveness against IPD. For each PCV’s direct effectiveness against inpatient pneumonia, outpatient pneumonia, and OM, we calculated the ratio of local PCV7 serotype coverage to local PCV10-GSK, PCV10-SII, and PCV13-PFE serotype coverage to estimate the direct effect of these higher valent vaccines in preventing disease manifestations. Direct effectiveness of PCV7 against inpatient and outpatient pneumonia was estimated to be 25.5% and 6.0%, respectively [31,32,33]. Thus, direct effectiveness of PCV13-PFE against inpatient pneumonia was 52.5% and 12.4% for outpatient pneumonia. Direct effectiveness of PCV7 was estimated to be 7.0% against clinical episodes of OM [33, 34], and therefore, we estimated that the direct effectiveness of PCV13-PFE against OM was 14.4%. The same method was used to calculate pneumonia and OM disease vaccine effectiveness for PCV10-GSK and PCV10-SII (Table 1).
Vaccination Costs
It was assumed that each child would receive three PCV doses at the Gavi, Advance Market Commitment (AMC) set single dose price of $3.05 for PCV10-GSK, $2.00 for PCV10-SII, and $2.90 for PCV13-PFE [35]. Vaccine administrative costs were assumed to be $1.25, which includes the cost of cold-chain, vaccine administration, and storage [36]. This amounted to a total vaccination cost per child of $12.90, $9.75, and $12.45 for PCV10-GSK, PCV10-SII, and PCV13-PFE, respectively.
Direct Health System Costs
Direct costs incurred by the healthcare system were estimated for each of the PCVs compared to no PCV SIP implementation, with costs reported in 2018 US dollars (Table 1). Inpatient and outpatient pneumonia treatment costs are sourced from Marfatia et al. (2015), a study conducted in Mumbai, India of direct medical costs incurred in both the public and private sector [37]. A weighted average was applied to these costs, acknowledging that the private sector in India accounts for approximately 60% of inpatient treatment [38, 39]. As a result, inpatient and outpatient pneumonia treatment costs were estimated to be $364.65 and $171.77, respectively. The cost of treating a case of OM was estimated using the reported generic outpatient cost in Constenla et al. (2019), averaging to $10.04 across the public and private sector [19]. As a result of a lack of treatment cost data differentiating bacteremia from meningitis, we assumed private and public sector treatment costs of $825.26 represent the cost borne by the healthcare system across all IPD manifestations [19].
Scenario Analysis
To account for the uncertainty in the clinical and cost inputs, scenario analyses were conducted in which base case estimates were adjusted for the national level analysis. A recent state-specific modeling analysis by Wahl et al. (2020) predicted pneumonia incidence rates that are twice as high for severe pneumonia and four times as high for non-severe pneumonia compared with our base case incidence rates [17, 26]. Therefore, we conducted a scenario analysis using the higher inpatient and outpatient pneumonia estimates and calculated the resulting impact. Additional scenario analyses were conducted to test parameter uncertainty and effects on results. All pneumococcal disease incidence estimates, associated health system costs, and case fatality rates were varied by ± 20%.
Results
Base Case Results: Universal Immunization Program (UIP)
Table 2 describes the estimated clinical and economic impact of implementing a PCV program in all of India assuming a national DPT3 uptake level of 71.5% by 2023. Compared to no vaccination, implementing PCV13-PFE nationally is estimated to prevent 12,055,216 cases of IPD, pneumonia, and OM and save 626,512 deaths between 2021 and 2025 in children under 5 years old. The $1.87 billion in medical cost savings from averted disease cases and deaths would offset the $827.73 million in PCV13-PFE vaccine costs, providing overall cost savings to India’s healthcare system of $1.04 billion across 5 years. A similar analysis of PCV10-GSK versus no vaccination estimated 8,400,527 disease cases and 436,577 deaths among children below the age of 5 to be prevented nationally over 5 years. Incurred vaccine costs ($857.65 million) would be offset from direct medical cost savings from PCV10-GSK vaccination ($1.30 billion), resulting in overall savings of $445.48 million. Meanwhile, national implementation of PCV10-SII is estimated to prevent 10,277,872 total IPD, pneumonia, and OM cases and 531,545 consequent deaths compared to no PCV vaccination over a 5-year period. PCV10-SII’s vaccine procurement cost of $648.22 million and direct medical cost savings of $1.59 billion result in net cost savings of $938.37 million.
Base Case Results: State Immunization Programs (SIPs)
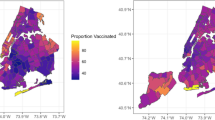
Tables 3 and 4 show the estimated pneumococcal disease cases and deaths averted and the costs saved with the three different PCVs compared to no vaccination across the 5-year period. The clinical and budget impact in each state and union territory varies widely depending on population size, burden of disease, and vaccine uptake. Across all states and union territories, introducing PCV13-PFE would prevent the greatest number of pneumococcal disease cases and save most lives of the three PCV programs, followed by PCV10-SII and PCV10-GSK, respectively (Table 3). Because of the incremental clinical impact of this higher valent vaccine, PCV13-PFE provides the greatest medical cost savings in all states and union territories (Table 4). As a result of this cost offset, PCV13-PFE SIP implementation would provide larger net health system savings than PCV10-GSK and PCV10-SII for many states and union territories in India.
Scenario Analysis Results
PCV13-PFE provides the greatest national reductions in disease cases and deaths compared to PCV10-GSK or PCV10-SII in each scenario analysis in which parameters of uncertainty were adjusted (Table 5). Varying all pneumococcal disease incidences, direct disease costs, and case fatality rates by ± 20% consistently determined PCV13-PFE as the most cost-saving PCV when compared to no vaccination program. When less conservative inpatient and outpatient pneumonia incidence rates reported in Wahl et al. (2020) were tested in the analysis, twice as many disease cases and deaths are estimated to be prevented and triple the cost savings are predicted to be attained by India’s health system as compared to base case estimates.
Discussion
This study estimated the potential public health and economic impact of including PCVs in every state and union territory’s immunization program in India. The three currently available PCVs in India, PCV13-PFE, PCV10-GSK, and PCV10-SII, were each compared to no vaccination program, given that most states have yet to introduce a PCV SIP. We modeled the number of cases and deaths averted and the potential budget impact of implementing routine infant PCV immunization at both a national and state level over a 5-year period (2021–2025).
This is the first study to estimate the public health and budget impact of all three PCVs, including the newest PCV licensed in India, PCV10-SII. These results can be used to inform future decisions on which vaccine should be implemented in both the pediatric UIP and SIPs in India. Furthermore, this study adds to the existing body of evidence by estimating the state-specific clinical and economic impact of PCV introduction based on available, state-specific pneumonia incidence and vaccine uptake data. Previous studies have considered the vaccine implementation at the national level, or selected a few states to estimate impact [19, 20, 40]. Because each PCV program will be implemented and monitored at the state level, our subnational analysis may highlight opportunities for disease prevention and economic savings to help inform future SIP introduction.
This study demonstrated that the greatest reduction in under-five morbidity and mortality is consistently predicted to occur with a PCV13-PFE immunization program as compared to PCV10-GSK or PCV10-SII in every state and union territory. Over 5 years, as many as 12.1 million pneumococcal disease episodes could be averted and 627,000 child lives could be saved if PCV13-PFE were nationally implemented. Of note, our estimated public health impact of PCV vaccination in India may be conservative, as a newly published paper modeling pneumonia incidence by state reported severe pneumonia to be twice as high and non-severe pneumonia to be four times as high as the incidence reported by Farooqui et al. (2015) [17, 26]. Moreover, our results show economic benefits from averted pneumococcal disease episodes, with the three PCVs providing between $1.30 billion and $1.87 billion in direct medical cost savings over a 5-year period. In all states and union territories, PCV13-PFE is estimated to provide the most medical cost savings, therefore generating the greatest net savings for most state health systems when vaccine acquisition costs are accounted for.
India’s Multi-Year Plan for immunization emphasized the need for “accelerated introduction of new and underutilized vaccines against diseases with significant morbidity and mortality in India” [41]. Despite this ambitious goal and PCVs being licensed in India since 2006, PCVs are currently not included in the majority of India’s SIPs. States with high disease burden, including Bihar, Uttar Pradesh, Madhya Pradesh, Rajasthan, Haryana, and Himachal Pradesh, began rolling out PCV13-PFE as a part of the UIP in 2017/18 [12, 13]. Our analysis suggests that other states would also avert a substantial amount of disease cases, deaths, and associated medical costs with the implementation of a PCV SIP, resulting in overall cost savings to their health system. Notably, introducing a PCV13-PFE vaccination program in Maharashtra, West Bengal, Andhra Pradesh, Karnataka, Gujarat, Tamil Nadu, Jharkhand, and Odisha could alone avert over five million cases of disease in children under 5 years old over a 5-year period.
Our results support previous work in which authors found that the inclusion of PCV13-PFE in India’s NIP is cost-effective [20, 40]. In a study by Megiddo et al. (2018), the authors examined the impact of implementing PCV13-PFE into India’s NIP at DPT3 coverage levels and concluded that there would be a substantial reduction in disease burden, financially protecting the poorest sector of the population from catastrophic medical costs [40]. Another economic evaluation determined that even in an unfavorable scenario for PCV implementation in terms of disease incidence and health system costs, introducing PCV13-PFE is still cost-effective in India [20]. However, Krishnamoorthy et al. (2019) highlights that the Indian government currently spends only 2% of the healthcare budget on immunization programs, and therefore vaccination spending will need to increase to maintain any ongoing or future PCV programs [20]. This finding is consistent with other countries where vaccine spending often lags behind overall health spending, limiting access to critical preventative health measures [42].
It is important to keep in mind when interpreting these results that PCV10-SII has limited data to inform health economic analyses. At present there are no clinical studies or real-world data evaluating the direct effects of PCV10-SII on pneumococcal disease or nasopharyngeal carriage. In this study, direct effects for PCV10-SII were assumed using commonly employed methods in PCV cost-effectiveness analyses by adjusting PCV7 efficacy values for additional serotypes covered in PCV10-SII. Derivation of the direct effects for PCV10-SII in this analysis should be interpreted with caution because as of licensure there is only one published phase 3 noninferiority study for PCV10-SII using PCV10-GSK as the comparator [43]. Data are therefore missing regarding a direct matched immune response for 6A and 19A, and extrapolation for direct effectiveness from this single study may not be warranted. Furthermore, as of 2021 there are no clinical trials ascertaining PCV10-SII’s effectiveness against non-invasive pneumococcal disease and the label in India does not contain an indication for OM [16]. Considering these clinical parameter uncertainties, results for the PCV10-SII arm in this study should be interpreted with caution until trial-based evidence or real-world outcomes data become available for carriage and pneumococcal disease manifestations.
Limitations
This study has several limitations that should be considered when interpreting the results. First, we did not consider the impact of serotype replacement in this analysis. This may have impacted the results, given that multiple countries implementing PCV pediatric programs with high vaccine uptake observe a large reduction in vaccine-type disease and a corresponding increase in non-vaccine serotypes [44, 45]. Some level of serotype replacement resulting in a small increase in disease incidence may have led to overestimations of impact in states with high PCV uptake, but overall this should have marginal impact on our study results. In certain settings, introducing lower valent PCVs in NIPs has resulted in rising disease cases attributable to unprotected serotypes. For example, after Belgium transitioned from PCV13-PFE to PCV10-GSK in the pediatric immunization program, 37 serotype 19A IPD cases in children under 2 years of age were recorded by 2018, an increase of 1750% from the 2 cases in 2015 [46]. With the implementation of PCV10-GSK or PCV10-SII in India, an increase in pneumococcal disease cases attributable to serotypes 3, 6A, and 19A or 3, 4, and 18C, respectively, may similarly occur. Therefore, future assessments should consider the impact of serotype replacement or re-emergence, especially if considering the use of lower valent PCVs.
Gavi has only guaranteed funding for PCVs in India until 2021, after which the Indian government may need to take on the cost of the vaccine for the public health system [13]. Given that our analysis assumed consistent uptake from 2021 to 2025 and does not consider government negotiated vaccine procurement, PCV programs may not be implemented as quickly as estimated if India does not continue financial support after Gavi funding ceases. Furthermore, this study does not consider the use of PCVs in the private market in India. A study conducted in 2012 found that private market PCV uptake in India was approximately 0.33% [47]. Because PCV vaccination in the private market is low, we did not include this factor in our analysis as the impact would likely be negligible.
A source of underestimation in our public health impact calculations is the broader societal value provided by PCV vaccination. Because of the short time horizon of this study and the uncertainty of a UIP with country-wide coverage, we did not include indirect effects of PCVs. Across a number of countries, high rates of PCV uptake have been shown to reduce pneumococcal disease in unvaccinated children and adults through indirect protection [48,49,50]. Additionally, PCVs provide other broader clinical benefits not captured in this analysis, such as reducing the need for antibiotic prescribing and lessening the occurrence of antimicrobial-resistant strains of S. pneumoniae [51]. Moreover, societal effects (productivity gains of parents/caregivers, improved social equity, and overall population quality of life gains) were not accounted for. If these broader benefits were included in this analysis, all PCVs would result in even more cost savings compared to no vaccination. Relatively, PCV13-PFE may result in even larger cost savings than PCV10-GSK or PCV10-SII, given the greater disease reduction and societal impact from broader serotype coverage.
Finally, surveillance systems in India are still being established and therefore limited state-specific data on serotype distribution, incidence, and associated costs of pneumococcal disease are available. Although estimates of pneumonia incidence are reported by state and union territory, this analysis was limited to national-level IPD and OM incidence and case fatality rates. Similarly, there are no state-level pneumococcal disease costing studies and therefore costs of disease episodes were based on most current and nationally representative data. However, when these estimates were rigorously tested in scenario analyses, PCV13-PFE consistently provided the greatest clinical and economic benefit.
Conclusion
This study was the first to estimate the public health and economic impact of the three currently licensed PCVs in India and report results by state and union territory. Because immunization programs are executed at the state level, our subnational analysis can inform each state of the local impact from introducing a PCV program in their SIP. Our findings demonstrate that implementation of PCV SIPs throughout India would lead to substantial public health and economic benefits compared to no vaccination. Out of the three PCVs, PCV13-PFE was estimated to provide the greatest public health impact and overall cost savings for children under 5 years old. Thus, India should consider expanding access to PCV13-PFE in remaining states and union territories to prevent the maximum morbidity and mortality associated with pneumococcal diseases and save the most costs for their health system.
Change history
08 September 2021
A Correction to this paper has been published: https://doi.org/10.1007/s40121-021-00526-3
Notes
Data are not available for Ladakh.
States with existing immunization programs include 1. Himachal Pradesh, 2. Haryana, 3. Rajasthan, 4. Uttar Pradesh, 5. Bihar, 6. Madhya Pradesh.
Union territories that were assumed to have average national incidence include 1. Andaman & Nicobar Islands, 2. Dadra & Nagar Haveli, 3. Daman & Diu, 4. Lakshadweep, 5. Puducherry.
References
World Health Organization. Pneumococcal conjugate vaccines in infants and children under 5 years of age. Wkly Epidemiol Rec. 2019;94(8):85–104.
O’Brien KL, Wolfson LJ, Watt JP, et al. Burden of disease caused by Streptococcus pneumoniae in children younger than 5 years: global estimates. Lancet. 2009;374(9693):893–902.
Wahl B, O’Brien KL, Greenbaum A, et al. Burden of Streptococcus pneumoniae and Haemophilus influenzae type b disease in children in the era of conjugate vaccines: global, regional, and national estimates for 2000–15. Lancet Glob Health. 2018;6(7):e744–57.
Ministry of Health & Family Welfare, Government of India. National operational guidelines: introduction of pneumooccal conjugate vaccine (PCV). 2017. http://www.nhm.gov.in/New_Updates_2018/NHM_Components/Immunization/Guildelines_for_immunization/Operational_Guidelines_for_PCV_introduction.pdf. Accessed 30 Apr 2021.
Liu L, Chu Y, Oza S, et al. National, regional, and state-level all-cause and cause-specific under-5 mortality in India in 2000–15: a systematic analysis with implications for the Sustainable Development Goals. Lancet Glob Health. 2019;7(6):e721–34.
Wahl B, Sharan A, Deloria Knoll M, et al. National, regional, and state-level burden of Streptococcus pneumoniae and Haemophilus influenzae type b disease in children in India: modelled estimates for 2000–15. Lancet Glob Health. 2019;7(6):e735–47.
Rodgers GL, Klugman KP. Surveillance of the impact of pneumococcal conjugate vaccines in developing countries. Hum Vaccin Immunother. 2016;12(2):417–20.
Chapman R, Sutton K, Dillon-Murphy D, et al. Ten year public health impact of 13-valent pneumococcal conjugate vaccination in infants: a modelling analysis. Vaccine. 2020;38(45):7138–45.
Lecrenier N, Marijam A, Olbrecht J, et al. Ten years of experience with the pneumococcal non-typeable Haemophilus influenzae protein D-conjugate vaccine (Synflorix) in children. Expert Rev Vaccin. 2020;19(3):247–65.
World Health Organization. Public assessment summary report: pneumococcal conjugate vaccine, (adsorbed, 10-valent) Serum Institute of India Pvt. Ltd.: World Health Organization; 2019. https://extranet.who.int/gavi/PQ_Web/FormAttachment.aspx?ID=2877. Accessed 30 Apr 2021.
Alderson MR, Sethna V, Newhouse LC, Lamola S, Dhere R. Development strategy and lessons learned for a 10-valent pneumococcal conjugate vaccine (PNEUMOSIL®). Hum Vaccin Immunother. 2021:1–8.
Gavi The Vaccine Alliance, The Government of India. Proposal form for Gavi NVS support for India—pneumococcal and measles rubella vaccines: Gavi The Vaccine Alliance; 2016. https://www.gavi.org/sites/default/files/temp/gavi_1570473800/India-PCV-2017/Proposal%20for%20NVS%20support%202017%20-%20MR%20and%20PCV%20-%20India.pdf. Accessed 30 Apr 2021.
Gavi The Vaccine Alliance. India’s most vulnerable children to get access to new vaccine against pneumonia: Gavi The Vaccine Alliance; 2017. https://www.gavi.org/news/media-room/indias-most-vulnerable-children-get-access-new-vaccine-against-pneumonia. Accessed 30 April 2021.
Times News Network. Goa to procure new vaccine from Unicef at Rs 1.2crore: Times of India; 2020. https://timesofindia.indiatimes.com/city/goa/goa-to-procure-new-vaccine-from-unicef-at-rs-1-2crore/articleshow/73282105.cms. Accessed 30 Apr 2021.
Indian Academic of Pediatrics Advisory Committee on Vaccines & Immunization Practices. Pneumococcal conjugate vaccines (PCVs): Indian Academic of Pediatrics; 2021. http://acvip.org/professional/columns/pcvs-vaccines. Accessed 30 Apr 2021.
Kasi SG, Shivananda S, Marathe S, et al. Indian Academy of Pediatrics (IAP) Advisory Committee on Vaccines and Immunization Practices (ACVIP): recommended immunization schedule (2020–21) and update on immunization for children aged 0 through 18 years. Indian Pediatr. 2021;58(1):44–53.
Farooqui H, Jit M, Heymann DL, Zodpey S. Burden of severe pneumonia, pneumococcal pneumonia and pneumonia deaths in Indian states: modelling based estimates. PLoS ONE. 2015;10(6):e0129191.
Ghia C, Wasserman M, Fletcher M, Farkouh R, Rambhad G. Modeling possible inclusion of pneumococcal conjugate vaccine into the National Immunization Program for infants in India. Value Health Reg Issues. 2018;15:99–105.
Constenla D, Liu T. Estimating the economic impact of pneumococcal conjugate, Haemophilus influenzae type b and rotavirus vaccines in India: national and state-level analyses. Vaccine. 2019;37(52):7547–59.
Krishnamoorthy Y, Eliyas SK, Nair NP, et al. Impact and cost effectiveness of pneumococcal conjugate vaccine in India. Vaccine. 2019;37(4):623–30.
Strutton DR, Farkouh RA, Earnshaw SR, et al. Cost-effectiveness of 13-valent pneumococcal conjugate vaccine: Germany, Greece, and the Netherlands. J Infect. 2012;64(1):54–67.
Klok RM, Lindkvist RM, Ekelund M, Farkouh RA, Strutton DR. Cost-effectiveness of a 10- versus 13-valent pneumococcal conjugate vaccine in Denmark and Sweden. Clin Ther. 2013;35(2):119–34.
Ministry of Home Affairs, Government of India. C-13 single year age returns by residence and sex: Office of the Registrar General & Census Commissioner, India; 2011 [updated January 21, 2020]. http://censusindia.gov.in/2011census/C-series/C-13.html. Accessed 30 Apr 2021.
United Nations Children’s Fun (UNICEF) India. National factsheet, coverage evaluation survey, 2009: India Water Portal; 2010. https://www.indiawaterportal.org/sites/default/files/iwp2/National_Factsheet_Coverage_Evaluation_Survey_UNICEF_2009.pdf. Accessed 30 Apr 2021.
Rudan I, O'Brien KL, Nair H, et al. Epidemiology and etiology of childhood pneumonia in 2010: estimates of incidence, severe morbidity, mortality, underlying risk factors and causative pathogens for 192 countries. J Glob Health. 2013;3(1):010401.
Wahl B, Knoll MD, Shet A, et al. National, regional, and state-level pneumonia and severe pneumonia morbidity in children in India: modelled estimates for 2000 and 2015. Lancet Child Adolesc Health. 2020;4(9):678–87.
Rupa V, Isaac R, Rebekah G, Manoharan A. Association of Streptococcus pneumoniae nasopharyngeal colonization and other risk factors with acute otitis media in an unvaccinated Indian birth cohort. Epidemiol Infect. 2016;144(10):2191–9.
Thomas K, Invasive Bacterial Infection Surveillance Group, International Clinical Epidemiology Network. Prospective multicentre hospital surveillance of Streptococcus pneumoniae disease in India. Lancet. 1999;353(9160):1216–21.
Nisarga R, Premalatha R, Ravikumar K, et al. Hospital-based surveillance of invasive pneumococcal disease and pneumonia in South Bangalore. India Indian Pediatr. 2015;52(3):205–11.
Black SB, Shinefield HR, Ling S, et al. Effectiveness of heptavalent pneumococcal conjugate vaccine in children younger than five years of age for prevention of pneumonia. Pediatr Infect Dis J. 2002;21(9):810–5.
Lucero MG, Dulalia VE, Nillos LT, et al. Pneumococcal conjugate vaccines for preventing vaccine‐type invasive pneumococcal disease and X‐ray defined pneumonia in children less than two years of age. Cochrane Database Syst Rev. 2009(4):CD004977.
Hansen J, Black S, Shinefield H, et al. Effectiveness of heptavalent pneumococcal conjugate vaccine in children younger than 5 years of age for prevention of pneumonia: updated analysis using World Health Organization standardized interpretation of chest radiographs. Pediatr Infect Dis J. 2006;25(9):779–81.
Ray GT, Whitney CG, Fireman BH, Ciuryla V, Black SB. Cost-effectiveness of pneumococcal conjugate vaccine: evidence from the first 5 years of use in the United States incorporating herd effects. Pediatr Infect Dis J. 2006;25(6):494–501.
Fireman B, Black SB, Shinefield HR, et al. Impact of the pneumococcal conjugate vaccine on otitis media. Pediatr Infect Dis J. 2003;22(1):10–6.
Gavi Secretariat and partners. Gavi-supported pneumococcal conjugate vaccines profiles to support country decision making: Gavi The Vaccine Alliance; 2019. https://www.gavi.org/sites/default/files/document/pcv-profilespdf.pdf. Accessed 30 Apr 2021.
Kim SY, Sweet S, Slichter D, Goldie SJ. Health and economic impact of rotavirus vaccination in GAVI-eligible countries. BMC Public Health. 2010;10(1):1–24.
Ghia CJ, Marfatia SA, Maniar TH, et al. Economic burden for management of community acquired pneumonia in children below 5 years in India. J Indian Med Assoc. 2018;116(10):23–26.
Organisation for Economic Co-operation and Development (OECD). OECD Health Statistics 2014 - How does India compare? OECD; 2014. http://www.oecd.org/els/health-systems/Briefing-Note-INDIA-2014.pdf. Accessed 30 Apr 2021.
Ministry of Health & Family Welfare. National Health Policy 2015 Draft: National Health Portal of India; 2014. https://www.nhp.gov.in/sites/default/files/pdf/draft_national_health_policy_2015.pdf. Accessed 30 Apr 2021.
Megiddo I, Klein E, Laxminarayan R. Potential impact of introducing the pneumococcal conjugate vaccine into national immunisation programmes: an economic-epidemiological analysis using data from India. BMJ Glob Health. 2018;3(3):e000636.
Subcommittee on Introduction of Hib Vaccine in Universal Immunization Program, National Technical Advisory Group on Immunization. NTAGI subcommittee recommendations on Haemophilus influenzae type B (Hib) vaccine introduction in India. Indian Pediatr. 2009;46(11):945–54.
Onishchenko K, Hill S, Wasserman M, et al. Trends in vaccine investment in middle income countries. Hum Vaccin Immunother. 2019;15(10):2378–85.
Clarke E, Bashorun A, Adigweme I, et al. Immunogenicity and safety of a novel ten-valent pneumococcal conjugate vaccine in healthy infants in the Gambia: a phase 3, randomised, double-blind, non-inferiority trial. Lancet Infect Dis. 2021. https://doi.org/10.1016/S1473-3099(20)30735-0.
Gladstone RA, Jefferies JM, Tocheva AS, et al. Five winters of pneumococcal serotype replacement in UK carriage following PCV introduction. Vaccine. 2015;33(17):2015–21.
Ladhani SN, Collins S, Djennad A, et al. Rapid increase in non-vaccine serotypes causing invasive pneumococcal disease in England and Wales, 2000–17: a prospective national observational cohort study. Lancet Infect Dis. 2018;18(4):441–51.
Desmet S, Lagrou K, Wyndham-Thomas C, et al. Dynamic changes in paediatric invasive pneumococcal disease after sequential switches of conjugate vaccine in Belgium: a national retrospective observational study. Lancet Infect Dis. 2021;21(1):127–36.
Farooqui HH, Zodpey S, Chokshi M, Thacker N. Estimates on state-specific pneumococcal conjugate vaccines (PCV) coverage in the private sector in the year 2012: evidence from PCV utilization data. Indian J Public Health. 2016;60(2):145–9.
Griffin MR, Zhu Y, Moore MR, Whitney CG, Grijalva CG. US pneumonia hospitalizations, a decade of pneumococcal conjugate vaccine use. N Engl J Med. 2013;369(2):155–63.
Waight PA, Andrews NJ, Ladhani SN, et al. Effect of the 13-valent pneumococcal conjugate vaccine on invasive pneumococcal disease in England and Wales 4 years after its introduction: an observational cohort study. Lancet Infect Dis. 2015;15(5):535–43.
Shiri T, Datta S, Madan J, et al. Indirect effects of childhood pneumococcal conjugate vaccination on invasive pneumococcal disease: a systematic review and meta-analysis. Lancet Glob Health. 2017;5(1):e51–9.
Bloom DE, Kirby PN, Pugh S, Stawasz A. Commentary: why has uptake of pneumococcal vaccines for children been so slow? The perils of undervaluation. Pediatr Infect Dis J. 2020;39(2):145–56.
Acknowledgements
Funding
This work, including the Journal’s Rapid Service Fee, was funded by Pfizer Inc.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
Gautam Rambhad, Canna J. Ghia, Johnna Perdrizet, Emily K Horn, and Matt D Wasserman contributed to the conception, design and implementation of research for this study. Ramaa Chitale, Johnna Perdrizet, Emily K Horn, and Matt D Wasserman contributed to the analysis of results. All authors contributed to the revision of the results and writing of the manuscript. We would like to acknowledge Consulting at McCann Health, a division of McCann Health Medical Communications Ltd., and Calum Jones for their role in the model development.
Disclosures
Johnna Perdrizet, Matt D Wasserman, and Emily K Horn are employees of Pfizer Inc and may own stock or stock options. Canna J. Ghia and Gautam Rambhad are employees of Pfizer India and may own stock or stock options. Ramaa Chitale was an employee of Pfizer Inc at the time of this study and is now affiliated with The George Washington University, Milken Institute School of Public Health.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
All data generated or analyzed during this study are included in this published article/as supplementary information files.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ghia, C.J., Horn, E.K., Rambhad, G. et al. Estimating the Public Health and Economic Impact of Introducing the 13-Valent Pneumococcal Conjugate Vaccine or 10-Valent Pneumococcal Conjugate Vaccines into State Immunization Programs in India. Infect Dis Ther 10, 2271–2288 (2021). https://doi.org/10.1007/s40121-021-00498-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-021-00498-4