Abstract
Background
Bacillus Calmette-Guérin (BCG)-unresponsive non-muscle invasive bladder cancer (NMIBC) is a newly defined subtype that is unlikely to benefit from BCG rechallenge. Radical cystectomy is currently recommended for BCG-unresponsive NMIBC; however, a certain proportion of these patients can be managed with treatments other than that. Herein, we conducted a multicenter retrospective study to analyze the clinical outcomes of BCG-unresponsive NMIBC patients who did not receive radical cystectomy.
Methods
Of the 141 BCG-unresponsive NMIBC patients, 94 (66.7%) received treatment except radical cystectomy. Survival outcomes were calculated from the date of diagnosis using the Kaplan–Meier method and compared using the log-rank test. Prognostic factors were identified using the multivariate Cox regression model. This group was further classified into three groups according to the number of risk factors, and survival outcomes were compared.
Results
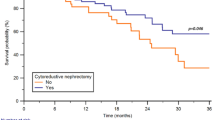
Multivariate analyses identified low estimated glomerular filtration rate (< 45 ml/min/1.73 m2) and large tumor size (≥ 30 mm) before BCG induction as independent poor prognostic factors for progression-free survival and overall survival, while the latter was also an independent factor for cancer-specific survival. The presence of variant histology was an independent poor prognostic factor for overall survival. The high-risk non-cystectomy group showed a significantly poor prognosis for progression-free survival (hazard ratio: 7.61, 95% confidence interval: 2.11–27.5), cancer-specific survival (10.4, 0.54–70.02), and overall survival (8.28, 1.82–37.7).
Conclusions
Our findings suggest that patients with renal impairment and large tumors should undergo radical cystectomy if the complications and intentions of the patients allow so.



Similar content being viewed by others
Abbreviations
- BCG:
-
Bacillus Calmette-Guérin
- BP:
-
Bladder prevention
- CIS:
-
Cancer in situ
- CKD-EPI:
-
Chronic Kidney Disease Epidemiology Collaboration
- CSS:
-
Cancer-specific survival
- ECOG-PS:
-
Eastern Cooperative Oncology Group-performance status
- eGFR:
-
Estimated glomerular filtration rate
- iBCG:
-
Bacillus Calmette-Guérin induction
- JUA:
-
Japanese Urological Association
- LVI:
-
Lymphovascular invasion
- NIMBC:
-
Non-muscle invasive bladder cancer
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- RC:
-
Radical cystectomy
- TURBT:
-
Transurethral resection of bladder tumor
References
Miyake M, Gotoh D, Shimada K et al (2015) Exploration of risk factors predicting outcomes for primary T1 high-grade bladder cancer and validation of the Spanish Urological Club for Oncological Treatment scoring model: long-term follow-up experience at a single institute. Int J Urol 22:541–547
Matsumoto H, Shiraishi K, Azuma H et al (2020) Clinical practice guidelines for bladder cancer 2019 update by the Japanese Urological Association: summary of the revision. Int J Urol 27:702–709
Babjuk M, Burger M, Compérat EM et al (2019) European Association of Urology guidelines on non-muscle-invasive bladder cancer (TaT1 and carcinoma in situ)—2019 update. Eur Urol 76:639–657
Chang SS, Bochner BH, Chou R (2017) Treatment of non-metastatic muscle-invasive bladder cancer: AUA/ASCO/ASTRO/SUO guideline. J Urol 198:552–559
Shirakawa H, Kikuchi E, Tanaka N et al (2012) Prognostic significance of Bacillus Calmette-Guerin failure classification in non-muscle-invasive bladder cancer. BJU Int 110:E216–E221
Lerner SP, Dinney C, Kamat A et al (2015) Clarification of bladder cancer disease states following treatment of patients with intravesical BCG. Bladder Cancer 1:29–30
Steinberg RL, Thomas LJ, Mott SL et al (2016) Bacillus Calmette-Guérin (BCG) treatment failures with non-muscle invasive bladder cancer: a data-driven definition for BCG unresponsive disease. Bladder Cancer 2:215–224
Klaassen Z, Kamat AM, Kassouf W et al (2018) Treatment strategy for newly diagnosed T1 high-grade bladder urothelial carcinoma: new insights and updated recommendations. Eur Urol 74:597–608
Kikuchi E, Hayakawa N, Fukumoto K et al (2020) Bacillus Calmette-Guerin-unresponsive non-muscle-invasive bladder cancer: its definition and future therapeutic strategies. Int J Urol 27:108–116
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Lamm DL, Blumenstein BA, Crissman JD et al (2000) Maintenance Bacillus Calmette-Guerin immunotherapy for recurrent Ta, T1 and carcinoma in situ transitional cell carcinoma of the bladder: a randomized Southwest Oncology Group Study. J Urol 163:1124–1129
Matsumoto H, Shiraishi K, Azuma H et al (2020) Clinical practice guidelines for bladder cancer 2019 edition by the Japanese Urological Association: revision working position paper. Int J Urol 27:362–368
Kamat AM, Gontero P, Palou J (2019) How should I manage a patient with tumor recurrence despite adequate Bacille Calmette-Guerin? Eur Urol 3:252–257
Sylvester RJ, Meijden APM, Oosterlinck W et al (2006) Predicting recurrence and progression in individual patients with stage Ta T1 bladder cancer using EORTC risk tables: a combined analysis of 2596 patients from seven EORTC trials. Eur Urol 49:466–477
Seisen T, Comperat E, Leon P (2014) Impact of histological variants on the outcomes of nonmuscle invasive bladder cancer after transurethral resection. Curr Opin Urol 24:524–531
Soave A, Schmidt S, Dahlem R et al (2015) Does the extent of variant histology affect oncological outcomes in patients with urothelial carcinoma of the bladder treated with radical cystectomy? Urol Oncol 33:21.e1-21.e9
Tae BS, Kim JK, Kang M et al (2017) Prognostic value of impaired estimated glomerular filtration rate in intravesical BCG-treated non-muscle-invasive bladder cancer patients. Sci Rep 7:1380
Blute ML, Kucherov V, Rushmer TJ et al (2017) Reduced estimated glomerular filtration rate (eGFR<60 mL/min/1.73 m2) at first transurethral resection of bladder tumour is a significant predictor of subsequent recurrence and progression. BJU Int 120:387–393
Ucpinar B, Erbin A, Ayranci A et al (2019) Prediction of recurrence in non-muscle invasive bladder cancer patients. Do patient characteristics matter? J BUON 24:1659–1665
Rausch S, Hennenlotter J, Todenhofer T et al (2014) Impaired estimated glomerular filtration rate is a significant predictor for non-muscle-invasive bladder cancer recurrence and progression-introducing a novel prognostic model for bladder cancer recurrence. Urol Oncol 32:1178–1183
Roth GA, Eichinger DL, Ankersmit HJ et al (2011) Increased total cytokerain-18 serum and urine levels in chronic kidney disease. Clin Chim Acta 11:713–717
Packiam VT, Werntz RP, Steinberg GD (2019) Current clinical trials in non-muscle-invasive bladder cancer: heightened need in an era of chronic BCG shortage. Curr Urol Rep 20:84
Mukherjee N, Svatek RS, Mansour AM (2018) Role of immunotherapy in Bacillus Calmette-Guerin-unresponsive non-muscle invasive bladder cancer. Urol Oncol 36:103–108
Kamat AM, Shore N, Hahn N et al (2020) KEYNOTE-676: phase III study of BCG and pembrolizmab for persistent/recurrent high-risk NMIBC. Future Oncol 16:507–516
Acknowledgements
The clinicopathological statistics are based on the results of contributions from a number of institutions in Japan. We thank the contributions of many urologists.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors disclose no potential conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
10147_2021_1988_MOESM1_ESM.tif
Supplementary file1 Supplementary Table 1. Comparison of background in patients with BCG-unresponsive NMIBC between the RC group and the non-RC group. Among the 141 patients with BCG-unresponsive NMIBC, 22 of the 73 in patients with high grade T1 at 3 months after initial BCG (30.1%), 17 of the 48 in patients with persistent high-grade NMIBC at 6 months despite adequate BCG (35.4%), and 8 of the 20 in patients with early relapsing (40.0%) underwent RC. Abbreviations: BCG, Bacillus Calmette-Guérin; NMIBC, non-muscle invasive bladder cancer; RC, radical cystectomy (TIF 572 KB)
10147_2021_1988_MOESM2_ESM.tif
Supplementary file2 Supplementary Table 2. Outcome of the non-radical cystectomy group. Of the patients undergoing TURBT alone, TURBT and BCG rechallenge and TURBT and maintenance intravesical chemotherapy, 13 (31.0%), 23 (51.1%), 5 (71.4%) did not experience progression. Abbreviations: TURBT, Transurethral resection of bladder tumor; BCG, Bacillus Calmette-Guérin (TIF 655 KB)
10147_2021_1988_MOESM3_ESM.tif
Supplementary file3 Supplementary Table 3. Univariate analyses for PFS, CSS and OS of the non-radical cystectomy group. The log-rank test showed that large tumor size and the presence of LVI before induction BCG were poor prognostic factors for PFS. Moreover, large tumor size (≥ 3 cm) before induction BCG was a poor prognostic factor for CSS, and low eGFR, large tumor size, and presence of variant histology before induction BCG were associated with OS. Abbreviations: PFS, Progression-free survival; CSS, cancer-specific survival; OS, Overall survival; LVI, Lymphovascular invasion; BCG, Bacillus Calmette-Guérin; eGFR, estimated glomerular filtration rate (TIF 1134 KB)
10147_2021_1988_MOESM4_ESM.tif
Supplementary file4 Supplementary Figure 1. Survival curves for outcomes of the non-radical cystectomy group according to prognostic factors. Survival curves for progression-free survival in the non-radical cystectomy group according to eGFR (a) and tumor size (b). Survival curves for cancer-specific survival according to tumor size (c). Survival curves for overall survival according to eGFR (d), tumor size (e), and variant histology (f). Abbreviations: eGFR, estimated glomerular filtration rate (TIF 786 KB)
About this article
Cite this article
Iida, K., Miyake, M., Murakami, K. et al. Bacillus Calmette-Guérin-unresponsive non-muscle invasive bladder cancer outcomes in patients without radical cystectomy. Int J Clin Oncol 26, 2104–2112 (2021). https://doi.org/10.1007/s10147-021-01988-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-021-01988-8