Abstract
Purpose
To evaluate the brain volumetric changes caused by BRAF gene mutation in non-epileptic CFC patients and the influence of the age of epilepsy onset on brain development in 2 cohorts of epileptic CFC patients.
Methods
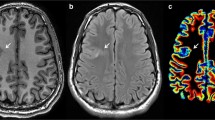
We enrolled CFC patients carrying BRAF gene mutations without epilepsy (4 patients) and with epilepsy (16 patients). CFC epileptic patients were divided into two cohorts based on the age of seizure onset: early-age onset (7 children) and late-age onset (9 adolescents). All three cohorts of patients underwent 3D FSPGR T1-weighted imaging to assess supratentorial and infratentorial brain volumes. Moreover, for each compartment, gray matter (GM), white matter (WM), and cerebrospinal fluid (CSF) volumes were measured. All measurements were compared with those of age-matched controls without neuroimaging abnormalities.
Results
All CFC patients showed supratentorial and infratentorial WM reduction and supratentorial ventricular enlargement (p < 0.01).
However, patients with early age of epilepsy onset, compared with the other two cohorts of CFC patients, showed both GM and a more pronounced WM volume reduction (p < 0.01).
Conclusion
In non-epileptic CFC children, we demonstrated WM volumetric reduction suggesting a direct effect of BRAF gene mutation on brain development. Nevertheless, in CFC epileptic patients, the age of epilepsy onset may contribute to brain atrophy.
Brain atrophy in CFC patients, in part due to the natural history of the disease, may be worsened by epilepsy when it begins in the early ages because of interference with brain growth at that critical age of development.



Similar content being viewed by others
References
Pierpont ME, Magoulas PL, Adi S et al (2014) Cardio-facio-cutaneous syndrome: clinical features, diagnosis, and management guidelines. Pediatrics 134:e1149–e1162. https://doi.org/10.1542/peds.2013-3189
Niihori T, Aoki Y, Narumi Y et al (2006) Germline KRAS and BRAF mutations in cardio-facio-cutaneous syndrome. Nat Genet 38:294–296. https://doi.org/10.1038/ng1749
Cao H, Alrejaye N, Klein OD et al (2017) A review of craniofacial and dental findings of the RASopathies. Orthod Craniofac Res 20(Suppl 1):32–38. https://doi.org/10.1111/ocr.12144
Myers A, Bernstein JA, Brennan ML et al (2014) Perinatal features of the RASopathies: Noonan syndrome, cardiofaciocutaneous syndrome and Costello syndrome. Am J Med Genet A 164A:2814–2821. https://doi.org/10.1002/ajmg.a.36737
Grebe TA, Clericuzio C (2000) Neurologic and gastrointestinal dysfunction in cardio-facio-cutaneous syndrome: identification of a severe phenotype. Am J Med Genet 95:135–143
Adachi M, Abe Y, Aoki Y, Matsubara Y (2012) Epilepsy in RAS/MAPK syndrome: two cases of cardio-facio-cutaneous syndrome with epileptic encephalopathy and a literature review. Seizure 21:55–60. https://doi.org/10.1016/j.seizure.2011.07.013
Yoon G, Rosenberg J, Blaser S, Rauen KA (2007) Neurological complications of cardio-facio-cutaneous syndrome. Dev Med Child Neurol 49:894–899. https://doi.org/10.1111/j.1469-8749.2007.00894.x
Rauen KA (1993) Cardiofaciocutaneous syndrome. In: Adam MP, Ardinger HH, Pagon RA, et al (eds) GeneReviews((R)). Seattle (WA)
Wakusawa K, Kobayashi S, Abe Y et al (2014) A girl with cardio-facio-cutaneous syndrome complicated with status epilepticus and acute encephalopathy. Brain Dev 36:61–63. https://doi.org/10.1016/j.braindev.2012.12.007
Cabrera S, Morel C, Tartaglia MC (2016) Clinical report: cognitive decline in a patient with cardiofaciocutaneous syndrome. Am J Med Genet A 170A:1251–1256. https://doi.org/10.1002/ajmg.a.37552
Rodriguez-Viciana P, Tetsu O, Tidyman WE et al (2006) Germline mutations in genes within the MAPK pathway cause cardio-facio-cutaneous syndrome. Science 311:1287–1290. https://doi.org/10.1126/science.1124642
Tidyman WE, Rauen KA (2009) The RASopathies: developmental syndromes of Ras/MAPK pathway dysregulation. Curr Opin Genet Dev 19:230–236. https://doi.org/10.1016/j.gde.2009.04.001
Papadopoulou E, Sifakis S, Sol-Church K et al (2011) CNS imaging is a key diagnostic tool in the evaluation of patients with CFC syndrome: two cases and literature review. Am J Med Genet A 155A:605–611. https://doi.org/10.1002/ajmg.a.33787
Manci EA, Martinez JE, Horenstein MG et al (2005) Cardiofaciocutaneous syndrome (CFC) with congenital peripheral neuropathy and nonorganic malnutrition: an autopsy study. Am J Med Genet A 137:1–8. https://doi.org/10.1002/ajmg.a.30834
Cizmeci MN, Lequin M, Lichtenbelt KD et al (2018) Characteristic MR imaging findings of the neonatal brain in RASopathies. AJNR Am J Neuroradiol 39:1146–1152. https://doi.org/10.3174/ajnr.A5611
Sabatino G, Verrotti A, Domizio S et al (1997) The cardio-facio-cutaneous syndrome: a long-term follow-up of two patients, with special reference to the neurological features. Childs Nerv Syst 13:238–241. https://doi.org/10.1007/s003810050075
Gross-Tsur V, Gross-Kieselstein E, Amir N (1990) Cardio-facio cutaneous syndrome: neurological manifestations. Clin Genet 38:382–386. https://doi.org/10.1111/j.1399-0004.1990.tb03600.x
Kahle KT, Kulkarni AV, Limbrick DD, Warf BC (2016) Hydrocephalus in children Lancet Lond Engl 387:788–799. https://doi.org/10.1016/S0140-6736(15)60694-8
Reinker KA, Stevenson DA, Tsung A (2011) Orthopaedic conditions in Ras/MAPK related disorders. J Pediatr Orthop 31:599–605. https://doi.org/10.1097/BPO.0b013e318220396e
Kousi M, Katsanis N (2016) The genetic basis of hydrocephalus. Annu Rev Neurosci 39:409–435. https://doi.org/10.1146/annurev-neuro-070815-014023
Calandrelli R, Pilato F, Massimi L et al (2020) Posterior cranial fossa maldevelopment in infants with repaired open myelomeningoceles: double trouble or a dynamic process of posterior cranial fossa abnormalities? World Neurosurg 141:e989–e997. https://doi.org/10.1016/j.wneu.2020.06.106
Caciagli L, Bernasconi A, Wiebe S et al (2017) A meta-analysis on progressive atrophy in intractable temporal lobe epilepsy: time is brain? Neurology 89:506–516. https://doi.org/10.1212/WNL.0000000000004176
Hocker S, Nagarajan E, Rabinstein AA et al (2016) Progressive brain atrophy in super-refractory status epilepticus. JAMA Neurol 73:1201–1207. https://doi.org/10.1001/jamaneurol.2016.1572
Kim YE, Baek ST (2019) Neurodevelopmental aspects of RASopathies. Mol Cells 42:441–447. https://doi.org/10.14348/molcells.2019.0037
Nickels KC, Zaccariello MJ, Hamiwka LD, Wirrell EC (2016) Cognitive and neurodevelopmental comorbidities in paediatric epilepsy. Nat Rev Neurol 12:465–476. https://doi.org/10.1038/nrneurol.2016.98
Vatansever D, Kyriakopoulou V, Allsop JM et al (2013) Multidimensional analysis of fetal posterior fossa in health and disease. Cerebellum 12:632–644. https://doi.org/10.1007/s12311-013-0470-2
Yushkevich PA, Piven J, Hazlett HC et al (2006) User-guided 3D active contour segmentation of anatomical structures: significantly improved efficiency and reliability. Neuroimage 31:1116–1128. https://doi.org/10.1016/j.neuroimage.2006.01.015
Chepkoech J-L, Walhovd KB, Grydeland H et al (2016) Effects of change in FreeSurfer version on classification accuracy of patients with Alzheimer’s disease and mild cognitive impairment. Hum Brain Mapp 37:1831–1841. https://doi.org/10.1002/hbm.23139
Dale AM, Fischl B, Sereno MI (1999) Cortical surface-based analysis. I Segmentation and surface reconstruction Neuroimage 9:179–194. https://doi.org/10.1006/nimg.1998.0395
Segonne F, Dale AM, Busa E et al (2004) A hybrid approach to the skull stripping problem in MRI. Neuroimage 22:1060–1075. https://doi.org/10.1016/j.neuroimage.2004.03.032
Fischl B, Salat DH, Busa E et al (2002) Whole brain segmentation: automated labeling of neuroanatomical structures in the human brain. Neuron 33:341–355. https://doi.org/10.1016/s0896-6273(02)00569-x
Desikan RS, Ségonne F, Fischl B et al (2006) An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. Neuroimage 31:968–980. https://doi.org/10.1016/j.neuroimage.2006.01.021
Iglesias JE, Van Leemput K, Bhatt P et al (2015) Bayesian segmentation of brainstem structures in MRI. Neuroimage 113:184–195. https://doi.org/10.1016/j.neuroimage.2015.02.065
Kang M, Lee Y-S (2019) The impact of RASopathy-associated mutations on CNS development in mice and humans. Mol Brain 12:96. https://doi.org/10.1186/s13041-019-0517-5
Aizaki K, Sugai K, Saito Y et al (2011) Cardio-facio-cutaneous syndrome with infantile spasms and delayed myelination. Brain Dev 33:166–169. https://doi.org/10.1016/j.braindev.2010.03.008
Suzuki-Muromoto S, Miyabayashi T, Nagai K et al (2019) Leucine-485 deletion variant of BRAF may exhibit the severe end of the clinical spectrum of CFC syndrome. J Hum Genet 64:499–504. https://doi.org/10.1038/s10038-019-0579-3
Bonilha L, Rorden C, Appenzeller S et al (2006) Gray matter atrophy associated with duration of temporal lobe epilepsy. Neuroimage 32:1070–1079. https://doi.org/10.1016/j.neuroimage.2006.05.038
Doucet GE, Sharan A, Pustina D et al (2015) Early and late age of seizure onset have a differential impact on brain resting-state organization in temporal lobe epilepsy. Brain Topogr 28:113–126. https://doi.org/10.1007/s10548-014-0366-6
Klingberg T, Hedehus M, Temple E et al (2000) Microstructure of temporo-parietal white matter as a basis for reading ability: evidence from diffusion tensor magnetic resonance imaging. Neuron 25:493–500. https://doi.org/10.1016/s0896-6273(00)80911-3
Munakata S, Okada T, Okahashi A et al (2013) Gray matter volumetric MRI differences late-preterm and term infants. Brain Dev 35:10–16. https://doi.org/10.1016/j.braindev.2011.12.011
Tierney AL, Nelson CA (2009) Brain development and the role of experience in the early years. Zero Three 30:9–13
Cendes F (2005) Progressive hippocampal and extrahippocampal atrophy in drug resistant epilepsy: review. Curr Opin Neurol 18:173–177. https://doi.org/10.1097/01.wco.0000162860.49842.90
Stefanatou M, Gatzonis S, Peskostas A et al (2019) Drug-responsive versus drug-refractory mesial temporal lobe epilepsy: a single-center prospective outcome study. Postgrad Med 131:479–485. https://doi.org/10.1080/00325481.2019.1663126
Kamali A, Kramer LA, Frye RE et al (2010) Diffusion tensor tractography of the human brain cortico-ponto-cerebellar pathways: a quantitative preliminary study. J Magn Reson Imaging 32:809–817. https://doi.org/10.1002/jmri.22330
Brodal P, Bjaalie JG (1997) Salient anatomic features of the cortico-ponto-cerebellar pathway. Prog Brain Res 114:227–249. https://doi.org/10.1016/s0079-6123(08)63367-1
Author information
Authors and Affiliations
Contributions
Rosalinda Calandrelli: project development, data collection, manuscript writing.
Fabio Pilato: data collection, statistical analysis, manuscript writing.
Marco Panfili: data collection.
Domenica Battaglia: data collection.
Maria Luigia Gambardella: patient recruitment, drafting paper.
Cesare Colosimo: project development, manuscript writing.
All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Rosalinda Calandrelli declares that she has no conflict of interest.
Fabio Pilato declares that he has no conflict of interest.
Marco Panfili declares that he has no conflict of interest.
Domenica Battaglia declares that she has no conflict of interest.
Maria Luigia Gambardella declares that she has no conflict of interest.
Cesare Colosimo declares that he is a scientific consultant for Bracco Diagnostics Inc. and Bayer HealthCare.
Ethical approval
We declare that all procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Calandrelli, R., Pilato, F., Panfili, M. et al. Brain structural changes in patients with cardio-facio-cutaneous syndrome: effects of BRAF gene mutation and epilepsy on brain development. A case–control study by quantitative magnetic resonance imaging. Neuroradiology 64, 185–195 (2022). https://doi.org/10.1007/s00234-021-02769-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-021-02769-w