Prevalence of somatic illnesses is higher in individuals with psychiatric disorders than in those without.Reference Momen, Plana-Ripoll, Agerbo, Benros, Børglum and Christensen1–Reference Tegethoff, Stalujanis, Belardi and Meinlschmidt4 The relationship appears to be bidirectional, with subsequent diagnoses of general medical conditions increased in those with psychiatric disorders and, among those identified with medical conditions, an increased risk of certain psychiatric disorders.Reference Scott, Kokaua and Baxter2,Reference Tegethoff, Stalujanis, Belardi and Meinlschmidt4 Eating disorders have both long-term somatic consequences as well as high somatic comorbidity and mortality;Reference Sartorius5,Reference Thornton, Watson, Jangmo, Welch, Wiklund and von Hausswolff-Juhlin6 however, the nature of the associations is unclear.
Two studies that explored a broad range of medical conditions following eating disorder diagnosis found increased risk for almost all studied medical conditions.Reference Momen, Plana-Ripoll, Agerbo, Benros, Børglum and Christensen1,Reference Scott, Lim, Al-Hamzawi, Alonso, Bruffaerts and Caldas-de-Almeida3 A third evaluated the association in both directions, finding a mix of increased and decreased risks for both subsequent medical conditions in those with eating disorders, and subsequent eating disorders in those with medical conditions.Reference Tegethoff, Stalujanis, Belardi and Meinlschmidt4 Eating disorders represent distinct psychiatric conditions with unique precipitating factors and physical sequelae. They include a heterogeneous group of conditions (i.e. anorexia nervosa, bulimia nervosa and eating disorder not otherwise specified (EDNOS)), which may carry differential risk for various medical conditions. Our group previously explored psychiatric and somatic comorbidity among individuals with psychiatric diagnoses in Denmark at a broad level, aiming to highlight associations of interest and encouraging further, more detailed work on comorbidity for specific disorders.Reference Momen, Plana-Ripoll, Agerbo, Benros, Børglum and Christensen1
The present study adapted the methods of these comprehensive studies of psychiatric disorder comorbidity in the Danish populationReference Momen, Plana-Ripoll, Agerbo, Benros, Børglum and Christensen1,Reference Plana-Ripoll, Pedersen, Holtz, Benros, Dalsgaard and de Jonge7 to parse comorbidity more extensively. We accessed Danish nationwide registers to provide gender-specific relative risks of diagnosis with a medical condition after eating disorder diagnosis and vice versa. Additionally, we calculated bidirectional gender-specific measures of absolute risk between different types of eating disorder and medical conditions, and estimates for matched reference groups. We expected an increased risk of subsequent medical condition diagnoses among those diagnosed with eating disorders; and increased risk of subsequent eating disorder diagnoses among those with prior medical conditions.
Method
To explore bidirectional associations between eating disorders and medical conditions, we determined: (a) risk of a medical condition diagnosis after diagnosis with an eating disorder (i.e. prior eating disorder–later medical condition); and (b) risk of an eating disorder diagnosis after diagnosis with a medical condition (i.e. prior medical condition–later eating disorder). Although the analyses for both directions were similar, there are notable differences. The methods are described below, and in greater detail in the supplementary material available at https://doi.org/10.1192/bjp.2021.104.
Study population and ascertainment of disorders of interest
This population-based cohort study included all individuals born in Denmark between 1977 and 2010 (n = 2 127 404) identified in the Danish Civil Registration System. To be included in the analyses, individuals had to be residing in the country at the start of follow-up (described below).
Eating disorders
Unlike other psychiatric diagnoses, eating disorder diagnoses are registered in both the Danish Psychiatric Central Research Register and the Danish National Patient Register; in 20−25% of anorexia nervosa cases, the first diagnosis is seen in the Patient Register. We used both registers, which is an addition from previous studies. For each individual, the initial diagnosis date was ascertained for anorexia nervosa (ICD-8 code 306.50; ICD-10 F50.0 and F50.1), bulimia nervosa (ICD-10 F50.2 and F50.3) and EDNOS (ICD-8 306.58 and 306.59; ICD-10 F50.8 and F50.9). As a specific code did not exist for bulimia nervosa in ICD-8, it was not possible to consider bulimia nervosa in all analyses. We therefore combined bulimia nervosa and EDNOS diagnoses to create an ‘other eating disorder’ (OED) category, consistent with previous investigations.Reference Zhang, Larsen, Kuja-Halkola, Thornton, Yao, Larsson and Lichtenstein8 Consequently, anorexia nervosa and OED were the primary eating disorder categories of interest; when possible, we examined bulimia nervosa and EDNOS separately.
General medical conditions
We selected 12 medical conditions, consistent with previous work on somatic comorbidity and eating disorders (Table 1 and supplementary Table 1).Reference Thornton, Watson, Jangmo, Welch, Wiklund and von Hausswolff-Juhlin6 The following labels were derived to group medical conditions: neurological, infectious, immune, respiratory, gastrointestinal, skin, musculoskeletal, genitourinary, circulatory, endocrine, congenital and injuries. Individuals with medical conditions were identified by combining information from the Danish National Patient Register and Cause of Death Register. Medical condition diagnosis date was the date of the first relevant hospital diagnosis or, if the individual died from a medical condition without having received a previous diagnosis, date of death.
Table 1 Eating disorders and general medical conditions: ICD codes used for definition and the frequency of cases among all individuals born in Denmark between 1977 and 2010 (n = 2 127 404)

OED, other eating disorder; EDNOS, eating disorder not otherwise specified.
Study design
The main analyses examined the bidirectional associations between two eating disorders (anorexia nervosa and OED) and the 12 medical conditions. We estimated associations between 46 temporally ordered eating disorder–medical condition pairs (i.e. all possible pairs, except those for which congenital malformations would be the later disorder).
To provide estimates of relative risk for most pairs, follow-up started on 1 January 1983 or the individual's sixth birthday, whichever occurred later (supplementary Fig. 1).
For prior eating disorder–later medical condition, depending on whether individuals had a diagnosis of a particular eating disorder between 1983 (6 years after the National Patient Register became available) and 2016, we estimated risk of receiving a diagnosis of each medical condition during follow-up. When considering chronic medical conditions (i.e. all except infections and injuries), individuals with a diagnosis prior to follow-up were excluded.
For prior medical condition–later eating disorder, depending on whether individuals had a diagnosis of a particular medical condition between 1977 (when the National Patient Register started) and 2016, we estimated the risk of receiving a diagnosis of each eating disorder during follow-up. Individuals with an eating disorder diagnosis prior to follow-up were excluded. In addition to considering anorexia nervosa and OED when eating disorders were the later disorder, we explored bulimia nervosa and EDNOS separately.
The exceptions were when immune disorders (‘immune medical conditions’) were one of the disorders of interest (follow-up from 1 January 2000), as it was not possible to ascertain immune disorders prior to the use of ICD-10 in the registers. Further details are provided in the supplementary material.
Statistical analysis
We compared the rate of diagnosis with a specific later disorder between those exposed and unexposed to each prior disorder using hazard ratios (HRs) and 95% confidence intervals (CIs), obtained via Cox proportional hazards models with age as the underlying timescale, using two models. Model A examined the association between a prior disorder and a later disorder, adjusted for gender and date of birth, which, in combination with underlying age in the models, also adjusted for calendar time. Model B included additional adjustment for other psychiatric disordersReference Plana-Ripoll, Pedersen, Holtz, Benros, Dalsgaard and de Jonge7 (detailed in the supplementary material) diagnosed before the prior disorder of interest. Prior OED was also included in Model B when anorexia nervosa was the eating disorder of interest; when bulimia nervosa was the eating disorder of interest, EDNOS was included. Individuals were followed up until the first of the following: diagnosis with the later disorder, death, emigration or end of follow-up (31 December 2016). A hierarchy was applied to eating disorder diagnoses: when considering OED or bulimia nervosa, anorexia nervosa also acted as a censoring event, like death or emigration. For EDNOS, both anorexia nervosa and bulimia nervosa acted as censoring events. Following the hierarchy ‘anorexia nervosa, bulimia nervosa, EDNOS’ ascribes association to one specific disorder not several.Reference Larsen, Munk-Olsen, Bulik, Thornton, Koch and Mortensen9
The prior disorders were treated as time-varying exposures for relative risks. Individuals were ‘unexposed’ to the prior disorder, becoming ‘exposed’ when diagnosed for the first time with this disorder.
We also estimated the cumulative incidence proportion (CIP) of diagnosis with a later disorder after diagnosis of a prior disorder, using competing risks survival analyses to account for individuals’ simultaneous risk of the later disorder, dying or emigrating. To compare CIPs among people with a prior disorder diagnosis with those among people without a diagnosis, a matched reference group was generated for each prior disorder. For every index person with the prior disorder, up to three age- and gender-matched individuals (who had not received a diagnosis of the relevant prior disorder at or before the age the index person was diagnosed) were randomly selected. More detailed information can be found in the supplementary material.
The Danish Data Protection Agency and the Danish Health Data Authority approved this study. By Danish law, no informed consent is required for a register-based study using anonymised data.
Results
In total, 2 127 404 million individuals were born in Denmark between 1977 and 2010. The number of cases of each medical condition and eating disorder in this population is presented in Table 1, and their baseline characteristics are presented in supplementary Table 2. The study population used to provide estimates of relative risk for all pairs (except those including immune disorders) consisted of 2 063 912 Danish residents (1 005 347 females and 1 058 565 males), followed up for 33.6 million person-years. During this time, 9433 individuals died and 43 264 emigrated. In the study population used for relative risks for pairs including immune disorders and for absolute risks, there were 2 058 865 million individuals (1 002 412 females and 1 056 453 males); however, total follow-up was 25.6 million person-years.
Bidirectional pairwise associations and absolute risks for all eating disorder–medical condition pairs are shown in Figs 1–3 and supplementary Figs 2–10. General findings are described below.
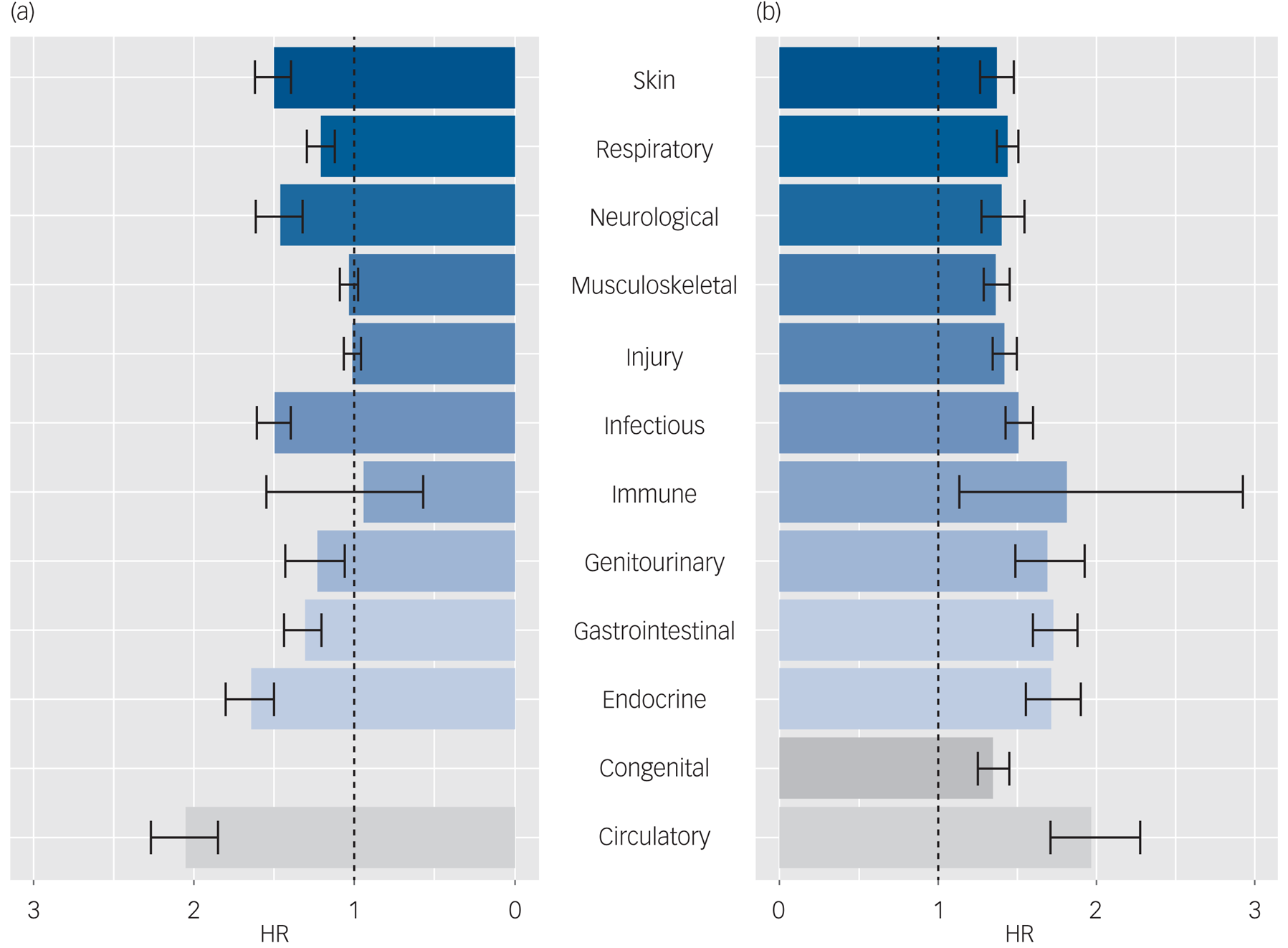
Fig. 1 The bidirectional associations between anorexia nervosa and general medical conditions for all persons (men and women).
Estimates were obtained via Cox proportional hazards models with age as the underlying timescale, adjusting for gender, calendar time and other mental disorders with onset before the prior disorder under study. (a) Hazard ratios (HRs) and 95% CIs for the risk of being diagnosed with a medical condition following a diagnosis of anorexia nervosa (i.e. anorexia nervosa is the prior disorder), compared with people without a diagnosis of anorexia nervosa. (b) HRs and 95% CIs for the risk of being diagnosed with anorexia nervosa following a medical condition diagnosis (i.e. the medical condition of interest is the prior disorder), compared with people without the medical condition. The line of unity is shown as a black dashed line in each plot.

Fig. 2 The bidirectional associations between ‘other eating disorder’ (OED) and general medical conditions for all persons (men and women).
Estimates were obtained via Cox proportional hazards models with age as the underlying timescale, adjusting for gender, calendar time and other mental disorders with onset before the prior disorder under study. (a) Hazard ratios (HRs) and 95% CIs for the risk of being diagnosed with a medical condition following a diagnosis of OED (i.e. OED is the prior disorder), compared with people without a diagnosis of OED. (b) HRs and 95% CIs for the risk of being diagnosed with OED following a medical condition diagnosis (i.e. the medical condition of interest is the prior disorder), compared with people without the medical condition. The line of unity is shown as a black dashed line in each plot.

Fig. 3 Absolute risks for general medical conditions and anorexia nervosa for all persons (men and women).
(a) Estimates of absolute risks for a later diagnosis within a medical condition, following a diagnosis of anorexia nervosa. (b) Absolute risks for a later diagnosis of anorexia nervosa, following a diagnosis of a medical condition. The cumulative incidence per 100 persons (solid lines for those with the prior disorder of interest, dashed lines for the matched reference groups) of receiving a diagnosis of each later disorder of interest, after a diagnosis of the prior disorder of interest. Shaded pale blue areas around the lines for those with the prior disorder of interest represent 95% CIs (in some panels these are obscured by the estimates line).
Relative risks
Results adjusted for gender, date of birth and other prior psychiatric disorders (i.e. Model B results) for all persons (both males and females) are shown for each direction for anorexia nervosa and OED in Figs 1 and 2. Results adjusted for gender and date of birth (Model A) can be found in the supplementary material.
Prior eating disorders–later medical conditions
Elevated risks for each later medical condition of interest were observed among all persons (i.e. both males and females combined) with the prior eating disorder of interest (anorexia nervosa or OED), for 21 of 22 pairs; however, the 95% CI included 1 for four of these. The point estimate for anorexia nervosa and subsequent immune disorders was slightly below 1 (0.94) but confidence intervals were imprecise and included 1. The highest Model B HR was seen for prior anorexia nervosa and later circulatory disorders (HR = 2.05, 95% CI 1.86−2.27). The lowest HR was 0.94 (95% CI 0.57−1.55), observed for anorexia nervosa and immune disorders. Model B estimates were slightly attenuated compared with Model A estimates (supplementary Table 3). Gender-specific HRs can be seen in supplementary Figs 2 and 3. The highest HR for males was for prior anorexia nervosa and later endocrine disorders (HR = 4.02, 95% CI 2.75−5.86); for females it was for prior anorexia nervosa and subsequent circulatory disorders (HR = 1.99, 95% CI 1.79−2.21).
Prior medical conditions–later eating disorders
For all persons, elevated risks for anorexia nervosa and OED were observed after diagnosis of all medical conditions of interest, and confidence intervals did not include 1 for any pair, except immune disorders–OED. The highest HR was seen for prior circulatory disorders and later anorexia nervosa (HR = 1.98, 95% CI 1.71−2.28). The lowest HR was for prior congenital disorders and subsequent anorexia nervosa (HR = 1.35 (95% CI 1.26−1.45). All Model B estimates were slightly higher than their corresponding Model A estimate (supplementary Table 4). Gender-specific HRs can be seen in supplementary Figs 2 and 3. The highest HR for males was for prior immune disorders and later anorexia nervosa (HR = 4.96, 95% CI 1.59–15.41); for females it was for prior circulatory disorders and later anorexia nervosa (HR = 1.99, 95% CI 1.72−2.31).
The HRs for bulimia nervosa and EDNOS excluding bulimia nervosa can be seen in supplementary Figs 4 and 5. The risk was increased for those with each medical condition, with the 95% CIs of 22 of 24 HRs not including 1.
Absolute risks
Figure 3(a) shows the all-person absolute risk of receiving each medical condition diagnosis after a previous diagnosis of anorexia nervosa. Conversely, Fig. 3(b) shows the risk of receiving an anorexia nervosa diagnosis after a prior diagnosis of each medical condition. Gender-specific absolute risks, as well as graphs for OED, bulimia nervosa and EDNOS as the later disorders of interest, are in the supplementary material.
Prior eating disorders–later medical conditions
For all pairs, cumulative incidence for all medical conditions was higher among those with prior eating disorders than without (with the exception of injuries). However, the proportions were similar. The highest cumulative incidence proportion (CIP) 15 years after an eating disorder diagnosis was seen for anorexia nervosa–injuries (among those with anorexia nervosa, CIP = 67.5%, 95% CI 65.0−70.0%). However, the CIP was even higher among their matched reference group (CIP = 80.6%, 95% CI 79.6−81.7%); similarly, high CIPs were observed for OED–injuries.
Prior medical conditions–later eating disorders
For all pairs, cumulative incidence for eating disorders was higher among those with prior medical conditions than without. However, the proportions were similar. The highest CIP within 15 years after medical condition diagnosis for all persons was seen for endocrine disorders–anorexia nervosa, at 0.89% (95% CI 0.80–1.01%). For the matched reference group, the CIP reached 0.61% (95% CI 0.56–0.66%).
Discussion
This population-based study, comprising 2.1 million individuals, shows patterns of comorbidity between eating disorders and medical conditions in both directions. In general, relative risks of being diagnosed with a range of medical conditions were higher among those with any type of eating disorder and, in a reciprocal fashion, risks of being diagnosed with any type of eating disorder were higher among those with a range of medical conditions. Absolute risks for both later eating disorders and medical conditions among those with the prior disorders of interest were similar to risks in the reference groups, but at a slightly higher level.
Although our findings are in line with those in the broad studies of Momen et al and Scott et alReference Momen, Plana-Ripoll, Agerbo, Benros, Børglum and Christensen1,Reference Scott, Lim, Al-Hamzawi, Alonso, Bruffaerts and Caldas-de-Almeida3 – which included prior eating disorders and later medical conditions – Tegethoff et alReference Tegethoff, Stalujanis, Belardi and Meinlschmidt4 found reduced risks for several medical conditions following eating disorders, including skin diseases, arthritis, heart disease and ‘any physical disease’. Furthermore, they found reduced risks for eating disorders following several medical conditions, including skin diseases, diabetes and gastrointestinal diseases. However, Tegethoff et al used survey data on 13- to 18-year-olds, so some differences could be due to the age of their study population. A Swedish study looking at somatic comorbidity among those with binge-eating disorder (included in our EDNOS category) did not consider temporality of the diagnoses but found estimates of similar magnitude as in our study.Reference Thornton, Watson, Jangmo, Welch, Wiklund and von Hausswolff-Juhlin6
Several studies focused on single eating disorder–medical condition pairs have also highlighted eating disorder comorbidity. For example, a study comparing patients admitted to hospital with bulimia nervosa with those admitted because of pregnancy complicationsReference Tith, Paradis, Potter, Low, Healy-Profitós and He10 found an increased risk of cardiovascular disease among those with bulimia nervosa; the observed HR was 4.25, which is higher than we found in our study. Another study reported that eating disorder diagnoses were higher among Danish female adolescents admitted for infections, compared with those not admitted for infections (HR = 1.22, similar in magnitude to our estimates of 1.58 for anorexia nervosa and 1.61 for OED in females).Reference Breithaupt, Kohler-Forsberg, Larsen, Benros, Thornton and Bulik11 A recent review concluded that it is plausible that comorbidity between eating disorders and gastrointestinal diseases is common and this could occur in either direction, supporting our findings.Reference Santonicola, Gagliardi, Guarino, Siniscalchi, Ciacci and Iovino12 Earlier studies have indicated associations between autoimmune diseases and eating disorders;Reference Zerwas, Larsen, Petersen, Thornton, Quaranta and Koch13,Reference Raevuori, Haukka, Vaarala, Suvisaari, Gissler and Grainger14 because of this link with some immune-mediated disorders, it could be expected that our study would have found risk of eating disorders to be higher in those with immune medical conditions, and vice versa. Although we found increased risks for most pairs of eating disorders and immune medical conditions, in both directions, the findings observed for prior anorexia nervosa–later immune medical conditions was suggestive of a slightly reduced risk, although 95% CIs included 1. It is important to note that immune disorders and autoimmune disorders comprise different disease entities. Additionally, for our immune medical condition category, 95% CIs are relatively wide; this is because disorders in this category are not as common as some of the other medical conditions and they are the only medical condition that could not be identified using ICD-8 codes.
Estimates of relative risk were attenuated when adjusting for additional prior psychiatric and eating disorders for the direction of prior eating disorders–later medical conditions, which is in keeping with evidence linking psychiatric disorders with an increased risk of subsequent medical conditions. However, for the direction of prior medical conditions–later eating disorders, adjustment for prior psychiatric disorders increased the resulting HRs slightly. It may be that prior medical conditions have stronger associations with eating disorders when no other psychiatric disorders are present, but this is speculative.
We had expected that HRs for medical conditions among people with anorexia nervosa would be slightly higher than HRs for medical conditions among people with OED (compared with their respective reference groups), as physical complications from anorexia nervosa are typically more severe.Reference Monteleone, Brambilla, N, RIG and M15 Although higher HRs were seen for anorexia nervosa for several medical conditions, this was not true for all medical conditions, and generally magnitudes did not differ greatly. A previous study in Danish adolescents found that risks for autoimmune and autoinflammatory diseases were elevated in those with eating disorders compared with those without;Reference Zerwas, Larsen, Petersen, Thornton, Quaranta and Koch13 the risk was elevated to a greater extent among those with bulimia nervosa than those with anorexia nervosa. Additionally, the patterns observed may reflect the higher mortality rates seen in those with anorexia nervosa; a higher proportion of those with anorexia nervosa may die before the ages at which medical conditions are typically diagnosed.Reference Arcelus, Mitchell, Wales and Nielsen16,Reference Weye, Momen, Christensen, Iburg, Dalsgaard and Laursen17
Risk factors for anorexia nervosa do differ considerably from risk factors for other psychiatric disorders; for example, some early adversities are associated with a decreased risk of anorexia nervosa, whereas there were increased risks for bulimia nervosa and EDNOS, and further increased risks for other psychiatric disorders.Reference Larsen, Munk-Olsen, Bulik, Thornton, Koch and Mortensen9 Additionally, associations for parental ages and multiple births have been shown to vary for different types of eating disorder.Reference Larsen, Bulik, Thornton, Koch and Petersen18 Further, in comparison to other psychiatric disorders, anorexia nervosa has more a pronounced metabolic component at a genetic level.Reference Watson, Yilmaz, Thornton, Hübel, Coleman and Gaspar19 However, when it comes to somatic comorbidities, eating disorders are similar and do not differ appreciably from other psychiatric disorders.Reference Momen, Plana-Ripoll, Agerbo, Benros, Børglum and Christensen1
When considering absolute risks, we found that higher proportions of those with eating disorders were subsequently diagnosed with medical conditions, and higher proportions of those with medical conditions were subsequently diagnosed with eating disorders. However, despite cumulative incidence being slightly higher following diagnosis with each disorder of interest, levels generally reflected those in the respective reference groups. The exception to this was later injuries, which were higher in the reference groups for both prior anorexia nervosa and OED. Although the risk of certain injuries could be expected to be higher among individuals who have previously had anorexia nervosa (e.g. fractures due to the effects of anorexia nervosa on bone mineral density, which can be evident after just 1 year of the eating disorder),Reference Herzog, Minne, Deter, Leidig, Schellberg and Wüster20,Reference Solmi, Veronese, Correll, Favaro, Santonastaso and Caregaro21 the observed lower risk could be due to behavioural differences, particularly in the earlier years post-diagnosis. Alternatively, it could be related to personality differences; a previous study suggested that people with eating disorders show higher levels of harm avoidance and lower levels of novelty-seeking (although the study was limited to women),Reference Klump, Strober, Bulik, Thornton, Johnson and Devlin22 which may result in them engaging in fewer behaviours that could lead to injury. By the end of the first year after start of follow-up, 12 out of 100 individuals with anorexia nervosa and 20 out of 100 in the reference group had attended hospital with an injury. Relatively speaking, cumulative incidence of injuries was almost 60% higher among those in the reference group than those in the anorexia nervosa group after the first year of follow-up. However, at 15 years after the start of follow-up, 73 out of 100 individuals with anorexia nervosa and 78 out of 100 in the reference group had attended hospital with an injury; so after 15 years, cumulative incidence of injuries was only 6% higher in the reference group.
The associations found were not markedly different depending on direction. There may be a number of reasons for the associations observed. Although in some cases associations may be causal, in others there may be shared mechanisms, or environmental or genetic risk factors. Alternatively, once receiving treatment for one disorder, other symptoms may be identified, leading to subsequent referrals and diagnoses.Reference Berkson23
Strengths and limitations
Our register-based study has several strengths. It uses the nationwide registers of Denmark, which provide data on the whole population, yielding a large sample size and minimising selection bias. Danish citizens have free and equal access to healthcare, thus any effect related to the ability to afford private insurance/access to healthcare is reduced. It is mandatory in Denmark for all hospitals to report discharge diagnoses to central registries. The study is not susceptible to recall bias and self-reporting bias (limitations of cross-sectional surveys which rely on retrospective recall in those individuals alive at the time of the survey and willing to participate). We considered all types of eating disorder, included a comprehensive range of medical conditions, and provided estimates of relative and absolute risks.
There are important limitations that should also be considered. First, in our study we included only 12 types of medical condition. However, the medical conditions selected were considered to be particularly relevant comorbidities for people with eating disorders. Furthermore, our analyses comprised individual pairs of eating disorders and medical conditions, which does not reflect the full complexity of comorbidity, as patients may experience multiple medical conditions, as well as multiple eating disorders, over time. Second, there may be misclassification with regard to ascertainment of conditions. Validity may vary across diagnoses. We do not have data on those who do not seek treatment for their disorders or those treated entirely in primary care settings. The UK's National Institute for Health and Care Excellence highlights that eating disorders are often untreated, especially in men.24 Furthermore, prescription medications were not used to ascertain medical conditions. Although this will affect ascertainment of some medical conditions more than others, cases will be biased to the more severe end of the clinical spectrum. As an example, people who present with hypertension or dyslipidaemia, which are often managed in primary care with medication, may be misclassified as not having a circulatory medical condition. Although it is difficult to speculate regarding the effect on HRs, underestimation of CIPs is likely among both those with prior disorders and their reference groups. Misclassification can also occur for onset: the date of administrative onset, as recorded in the registers, will be later than the actual onset of eating disorders and many medical conditions. A German study reported that the mean duration of untreated anorexia nervosa was over 2 years, in which time physiological effects could have already occurred.Reference Neubauer, Weigel, Daubmann, Wendt, Rossi and Löwe25 This may lead to incorrect temporal ordering of eating disorders and medical conditions. Third, the length of follow-up is limited by the period of time the relevant registers have been available, as well as the ICD codes in use at different times. When looking at absolute risks for prior eating disorders–later medical conditions, medical conditions had to be diagnosed within 15 years of the eating disorder diagnosis (owing to data availability); this duration of follow-up may have been insufficient for the population to experience late-onset medical condition diagnosis (and thus to capture all potential comorbidity). Studies on psychiatric disorders have suggested that risk of comorbid diagnoses is greatest in the years closely succeeding the index diagnosis,Reference Momen, Plana-Ripoll, Agerbo, Benros, Børglum and Christensen1,Reference Plana-Ripoll, Pedersen, Holtz, Benros, Dalsgaard and de Jonge7,Reference Tith, Paradis, Potter, Low, Healy-Profitós and He10 but longer follow-up, which can be incorporated into future studies as more register data become available, will be informative. Fourth, there are likely to be several factors associated with both eating disorders and medical conditions that we were unable to consider in our study, such as socioeconomic status, genetic factors and childhood adversity. Finally, the generalisability of our findings outside of Denmark may be limited. Observed patterns of comorbidity may vary in other countries, especially those with different healthcare structures.
Future research and clinical implications
There are several ways that research can add to our understanding of comorbidity in those with different types of eating disorder. Future studies can further investigate associations at the broad level, for example, by considering patterns of comorbidity or causes of mortality. In addition, studies can evaluate associations in finer detail, by considering individual pairs of eating disorders and medical conditions, and the specific diagnoses within each category.
This study provides a broad examination of the comorbidity between different types of eating disorder and medical conditions. Our findings highlight that those with eating disorders have increased risks of most types of medical condition, and those with medical conditions have increased risks of eating disorders – risks are elevated bidirectionally. This information may be useful in clinical settings, particularly for clinicians working with patients with eating disorder diagnoses, to help early identification of medical conditions, as most medical conditions appear to be more common for individuals with eating disorders.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjp.2021.104.
Data availability
No additional data are available. Access to individual-level Denmark data is governed by Danish authorities. These include the Danish Data Protection Agency, the Danish Health Data Authority, the Ethical Committee and Statistics Denmark. Each scientific project must be approved before initiation, and approval is granted to a specific Danish research institution. Researchers at Danish research institutions may obtain the relevant approval and data. International researchers may gain data access if governed by a Danish research institution that has the needed approval and data access.
Author contributions
L.V.P. came up with the study idea. All authors contributed to the design of the study. N.C.M., O.P.-R. and L.V.P. planned the analysis. N.C.M. carried out the analysis. All authors contributed to the interpretation of the findings. N.C.M. and L.V.P. prepared the first draft of the manuscript, and all authors provided critical revisions. All authors approved the version to be published and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding
Z.Y. acknowledges grant support from the National Institute of Mental Health (NIMH) (R01MH105500; R01MH120170) and Brain and Behavior Research Foundation (NARSAD Young Investigator Award, grant no. 28799). C.M.B. is supported by NIMH (R01MH120170; R01MH119084; R01MH118278; U01 MH109528); Brain and Behavior Research Foundation Distinguished Investigator Grant; Swedish Research Council (Vetenskapsrådet, award: 538-2013-8864); Lundbeck Foundation (grant no. R276-2018-4581). J.M. is supported by the Danish National Research Foundation (Niels Bohr Professorship). J.M. is employed by the Queensland Centre for Mental Health Research, which receives core funding from the Department of Health, Queensland Government. O.P.-R. has received funding from the European Union's Horizon 2020 research and innovation programme under the Marie Sklodowska-Curie grant agreement no. 837180. L.V.P. received funding from Lundbeck Foundation (grant no. R276-2018-4581) and the Novo Nordisk Foundation (grant no. NNF20OC0064993). The investigators conducted the research independently. The funders had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; or the decision to submit the manuscript for publication.
Declaration of interest
C.M.B. reports: Shire (grant recipient, Scientific Advisory Board member); Idorsia (consultant).










eLetters
No eLetters have been published for this article.