Abstract
Background
Although type 2 diabetes (T2D) remission after gastric cancer surgery has been reported, little is known about the predictors of postoperative T2D remission.
Methods
This study used data from a nationwide cohort provided by the National Health Insurance Service in Korea. We developed a diabetes prediction (DP) score, which predicted postoperative T2D remissions using a logistic regression model based on preoperative variables. We applied machine-learning algorithms [random forest, XGboost, and least absolute shrinkage and selection operator (LASSO) regression] and compared their predictive performances with those of the DP score.
Results
The DP score comprised five parameters: baseline body mass index (< 25 or ≥ 25 kg/m2), surgical procedures (subtotal or total gastrectomy), age (< 65 or ≥ 65 years), fasting plasma glucose levels (≤ 130 or > 130 mg/dL), and antidiabetic medications (combination therapy including sulfonylureas, combination therapy not including sulfonylureas, single sulfonylurea, or single non-sulfonylurea]). The DP score showed a clinically useful predictive performance for T2D remission at 3 years after surgery [training cohort: area under the receiver operating characteristics (AUROC) 0.73, 95% confidence interval (CI), 0.71–0.75; validation cohort: AUROC 0.72, 95% CI 0.69–0.75], which was comparable to that of the machine-learning models (random forest: AUROC 0.71, 95% CI 0.68–0.74; XGboost: AUROC 0.70, 95% CI 0.67–0.73; LASSO regression: AUROC 0.75, 95% CI 0.73–0.78 in the validation cohort). It also predicted the T2D remission at 6 and 9 years after surgery.
Conclusions
The DP score is a useful scoring system for predicting T2D remission after gastric cancer surgery.
Similar content being viewed by others
Introduction
Approximately 10% of all patients with gastric cancer have a comorbid type 2 diabetes (T2D), which was diagnosed before the cancer [1,2,3]. The management of T2D in patients with cancer is critical because of the high risk of cancer- and non-cancer-related mortality in patients with pre-existing T2D [4, 5]. Recent studies have also shown that T2D is associated with a high mortality rate in gastric cancer survivors [6, 7]. However, T2D care in patients with gastric cancer is demanding because of the variable course of T2D after gastrectomy for cancer. Previous studies have reported the remission, improvement, or even aggravation of T2D in patients who underwent gastrectomy for cancer [8,9,10]. Considering that gastrectomy for cancer is a treatment modality that results in the postoperative alteration of glycemic control, the development of an accurate method to predict T2D prognosis is warranted for individualized glycemic control in patients who undergo gastric cancer surgery.
The foregut comprises the stomach, duodenum, and proximal jejunum and is responsible for the absorption of various nutrients and for gastrointestinal hormone regulation [11, 12]. Gastrectomy, the standard curative therapeutic option for gastric cancer [13, 14], modifies foregut physiology and subsequently alters the metabolic parameters related to glycemic control and the prognosis of T2D [8, 9, 15,16,17,18]. Therefore, patients with T2D who undergo gastrectomy for cancer experience a characteristic course referred to as T2D remission, which is defined as normoglycemia without the use of antidiabetic medication; this usually occurs within 1 year after surgery [10]. The reported T2D remission rate varies from 3 to 65% in patients who undergo gastrectomy for cancer [9, 16]. Previous studies have suggested that postoperative T2D remission is related to the preoperative body mass index (BMI), use of antidiabetic medications, and type of surgical procedure [8, 17, 18]. However, these studies included a small number of patients from a single center and provided limited information on the prediction of T2D remission after gastric cancer surgery.
Therefore, using a nationwide population-based cohort, we aimed to develop and to validate a novel easy-to-use scoring system to predict the probability of T2D remission after gastric cancer surgery, based on the preoperative clinical condition. In addition, we adopted machine-learning approaches to compare the predictive performances of the algorithms and our novel scoring system.
Methods
Data source and study population
The National Health Insurance Service (NHIS) exclusively manages a mandatory insurance system. It covers the entire Korean population and provides health examinations for all Korean people aged ≥ 40 years. To obtain the health examination data, we used a customized NHIS database for patients who underwent total or subtotal gastrectomy for cancer among Koreans between 2004 and 2014 and who underwent health examinations within 2 years before surgery. This database includes patient demographics and socioeconomic variables, medical treatments, procedures, and diagnoses, and a health examination dataset that includes the results of questionnaires on lifestyles as well as the results of biannual health examinations that are provided for all insured individuals aged ≥ 40 years. Detailed description of the NHIS database can be found in previous studies [19].
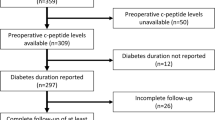
Using the International Classification of Diseases-10 Clinical Modification (ICD-10-CM) codes for total gastrectomy (Q2533–Q2537, QA533, QA535, and QA536), subtotal gastrectomy (Q0251–Q0259, Q2594, Q2595, Q2597, Q2598, QA595, QA597, and QA598), and gastric cancer (C16), we identified 61,179 patients who underwent gastric cancer surgery and who received health examinations within 2 years before surgery (Supplementary Fig. 1). The index date was defined as the date of the gastrectomy for cancer. We excluded participants without T2D (defined as at least one claim per year for the prescription of antidiabetic medication under ICD-10-CM codes E11–E14 within 2 years before the index date) (n = 41,791), those with a history of other cancers (ICD-10 CM codes, C00–C15 and C17–C97) or chemotherapy within 2 years before the index date (n = 13,006), patients with missing data (n = 240), and patients who died within 3 years after gastrectomy (n = 992). Finally, 5150 patients with T2D who underwent gastrectomy for cancer with ≥ 3 years of follow-up were enrolled. The participants were assigned randomly in a 7:3 ratio to a training cohort (for the development of a statistical model) (n = 3546) and a validation cohort (n = 1604). This study was approved by the Institutional Review Board of Korea University Anam Hospital (No. 2019AN0156), and the requirement for informed consent was waived because the customized database contained de-identified and anonymized data.
Outcome variables
We assessed T2D remission 3 years after gastric cancer surgery. Postoperative T2D remission was defined as the absence of antidiabetic medication prescription for at least 1 year [20]. Given (1) that there still exists extensive heterogeneity in the definition of T2D remission [21], and (2) the characteristics of patients with gastric cancer (e.g., old age and a longer duration of T2D) and variable glycemic goals in older adults (e.g., less stringent glycemic goals in patients with multiple coexisting chronic illnesses or functional dependence) [22], instead of applying uniform cut-off values to indicate glycemic control, we defined T2D remission after gastric cancer surgery based on the use of antidiabetic medication. Patients who died within 1 year after T2D remission were excluded from the analysis to avoid the influence of factors contributing to mortality on glycemic control. Patients were followed up until the date of death or until December 31, 2017, whichever came first.
Definitions of outcome variables obtained from the NHIS health examination database, including smoking status, alcohol consumption, regular exercise, income level, serum glucose levels, BMI, and baseline comorbidities, are described in Supplementary Table 1. Data on adjuvant chemotherapy medication within 1 year after gastric cancer surgery were collected, and antidiabetic medications at the index date were recorded and divided into seven classes (metformin, sulfonylurea, DDP-4 inhibitors, alpha-glucosidase inhibitors, thiazolidinediones, meglitinides, and insulins).
Development of the diabetes prediction (DP) score
The diabetes prediction (DP) score was developed using logistic regression, according to the following steps: first, we assessed the clinical variables, including the comorbidities, drugs used, laboratory measurements, and lifestyle factors, in univariate and multivariable logistic regression models to identify independent predictors of T2D remission. The nonlinearity of the continuous covariates was checked by categorizing the data into groups (e.g., using quartiles of the distribution or medically valid cut-off values). We performed sensitivity analyses to assess whether the statistical significance of the predictors included in the model remained for the different definitions of T2D remission and for the population that underwent gastric cancer surgery before 2008. Second, in the multivariable models, variables with P values < 0.05, were considered for inclusion in our scoring system. The odds ratios (ORs) were used to guide the development of a weighting system for DP scores. The interactions between the parameters included in the DP scores were assessed.
Validation of the DP score
To assess the validity of the scoring system, we retrospectively calculated the DP score for each patient in the validation cohort and performed Cochran–Armitage trend tests to investigate the association between the predicted and actual T2D remission rates. We also used receiver operating characteristic (ROC) curves and the estimated area under the ROC curve (AUROC) values with 95% confidence intervals (CIs). A value > 0.8 indicated excellent diagnostic accuracy, as a model with an AUROC > 0.7 indicates a clinically useful prognostic model [23, 24]. The sensitivities and specificities were obtained from the various cut-off values of the fitted probabilities in the models.
Machine-learning approaches
We applied machine-learning algorithms to the same dataset that was used to develop the DP scores and compared their predictive performances. The machine-learning algorithm is an analytical method that is used in an automated model building process. We used the following three algorithms, which are widely known methods that are used in the clinical field: least-absolute shrinkage and selection operator (LASSO) logistic regression [25], extreme gradient boosting (XGBoost) [26], and random forest [27]. The LASSO logistic regression optimizes the bias-variance trade-off by performing the selection of variables with regularization to solve the overfitting problem. The XGBoost, an ensemble learning algorithm based on the gradient-boosted tree algorithm, solves the shortcomings of the gradient-boosted methods such as slow execution time and lack of regularization. The random forest is also an ensemble learning algorithm that works by constructing and merging multiple decision trees. We trained the models to learn the optimal hyperparameter via an adaptive search, using these three machine-learning algorithms, with a threefold cross-validation, in the training cohort. All the variables included in the logistic regression for the development of the DP score (Supplementary Table 2) were included in the models using the machine-learning approaches. The AUROCs were calculated to evaluate and to compare the performances of the models and overall discrimination of the models.
Performance of the DP score in long-term follow-up
The T2D remission rates according to the DP scores were evaluated at 6 and 9 years after gastric cancer surgery by estimating the number of patients maintaining T2D remission, excluding the deceased participants at each point. The Cochran–Armitage trend tests were performed to investigate the association between the predicted values and actual T2D remission rates. The a priori level of statistical significance was set at P < 0.05. These analyses were two-tailed and were performed using SAS software (version 9.3; SAS Institute Inc., Cary, NC, USA).
Results
Baseline characteristics
The mean age of the training cohort was 65.2 years [standard deviation (SD) 8.8 years], and 23.2% of the patients were women (Table 1). The mean BMI was 24.6 kg/m2 (SD 3.0 kg/m2). The mean fasting plasma glucose (FPG) level was 138.5 mg/dL (SD 48.9 mg/dL), and 27.0% of the patients used insulin for glycemic control. Within the training cohort, 19.0% and 81.0% of the patients underwent total and subtotal gastrectomies, respectively, while 19.5% received adjuvant chemotherapy after gastric cancer surgery. The validation cohort presented no significant difference from the training cohort in terms of baseline characteristics, including age (mean 65.0 years; SD 8.7 years), sex ratio (female 22.7%), BMI (mean 24.5 kg/m2; SD, 3.1 kg/m2), FPG (mean 136.7 mg/dL; SD 47.3 mg/dL), antidiabetic medications, surgical procedures (total gastrectomy, 17.8%), adjuvant chemotherapy (18.8%), and the presence of comorbidities except for liver disease (training cohort 11.7%; validation cohort 8.9%; P = 0.003).
Predictors of T2D remission after gastric cancer surgery
The T2D remission rate at 3 years after gastric cancer surgery was 25.2% in the training cohort. Our multivariable logistic regression model identified variables that were associated with T2D remission 3 years after surgery (Table 2). Regarding baseline BMI, we categorized five BMI intervals: < 18.5, 18.5–23, 23–25, 25–30, and ≥ 30 kg/m2, taking into account the World Health Organization recommendations for Asian populations [28]. In the multivariable model, two BMI intervals of obesity showed a stepwise increasing likelihood of T2D remission compared with the normal weight intervals: BMI 25–30 kg/m2 (OR 1.59; 95% CI 1.29–1.96) and ≥ 30 kg/m2 (OR 2.08; 95% CI 1.41–3.08). Total gastrectomy, as compared with subtotal gastrectomy (OR 1.46; 95% CI 1.20–1.79), age < 65 years, as compared with ≥ 65 years (OR 1.41; 95% CI 1.18–1.68), and FPG ≤ 130 mg/dL as compared with > 130 mg/dL (OR 1.97; 95% CI 1.65–2.34), were associated with T2D remission. Furthermore, the presence of hypertension (OR 0.78; 95% CI 0.65–0.95) and mild (OR 1.25; 95% CI 1.01–1.55) and heavy alcohol consumption (OR 1.33; 95% CI 1.04–1.72) were also significantly associated with T2D remission (Supplementary Table 2). The use of an adjuvant chemotherapy regimen did not significantly influence the final logistic model, and the use of adjuvant chemotherapy (yes or no) was adjusted in the multivariable model.
Multivariable logistic regression analysis (Supplementary Table 2) showed that the use of a single antidiabetic medication was associated with a higher T2D remission rate than the use of two or more antidiabetic medications (OR 3.00; 95% CI 2.54–3.54). Among various antidiabetic medications, sulfonylureas were the most strongly associated with postoperative T2D remission; the non-use of sulfonylureas significantly increased the likelihood of T2D remission compared with the use of sulfonylureas (OR 4.16; 95% CI 3.45–5.03). Therefore, we classified the antidiabetic medication regimen into four categories according to the number of antidiabetic medications and use of sulfonylureas, that is, single non-sulfonylurea, single sulfonylurea, combination therapy including a sulfonylurea, and combination therapy not including a sulfonylurea. The use of a single non-sulfonylurea agent as compared with the use of combination therapy with a sulfonylurea (OR 7.57; 95% CI 6.03–9.49) increased the likelihood of T2D remission after surgery (Table 2).
Sensitivity analyses showed that the statistical significance of the predictors remained significant when different definitions were applied for T2D remission (discontinuation of antidiabetic medication with FPG level < 126 mg/dL or FPG level < 100 mg/dL) and when only patients undergoing gastric cancer surgery before 2008 were included in the analysis, as shown in Supplementary Table 3 and 4, respectively.
Development and validation of the DP score
The ORs of the five variables in the multivariable model were used to develop a scoring system that assigned scores for high BMI, total gastrectomy, young age, low FPG, and small number of antidiabetic medications or non-use of sulfonylureas (Table 3). Although the presence of hypertension and alcohol consumption was significantly related to the T2D remission rate, the inclusion of these predictors did not improve the predictive performance of the score; consequently, these factors were excluded from the final scoring system. The DP scores ranged from 0 to 14. We stratified patients into five groups according to their DP scores: 0–2, 3–5, 6–8, 9–11, and 12–14 (Supplementary Table 5). High scores predicted a high probability of postoperative T2D remission (P for trend < 0.001; Supplementary Fig. 2). No interactions were identified between the variables in the DP scores. At 3 years after surgery, 57.0% of the patients who scored 12–14, 43.4% of those who scored 9–11, 35.4% of those who scored 6–8, 15.8% of those who scored 3–5, and 11.5% of those who scored 0–2 achieved T2D remission. In the validation cohort, a high DP score also predicted a high probability of T2D remission at 3 years after gastric cancer surgery (P for trend < 0.001).
Comparison of the performance of the DP score and the machine-learning models
The DP score showed a clinically useful discrimination for T2D remission within both the training (AUROC 0.73; 95% CI 0.71–0.75) and validation cohorts (AUROC 0.72, 95% CI 0.69–0.75), with the performance approaching that of the random forest, XGboost, and LASSO regression algorithms (ranging from 0.70 to 0.75) (Table 4). The sensitivities and specificities of the different rules in predicting T2D remission at 3 years after surgery were assessed (Supplementary Table 6).
Effectiveness of the DP score in predicting T2D remission in long-term follow-up
Patients who underwent T2D remissions at 3 years after surgery were followed up for a median of 4.4 years (interquartile range 2.8–6.7 years; maximum, 14.7 years). High DP scores consistently predicted a high probability of T2D remission at 6 and 9 years after surgery (P for trend < 0.0001 for trend) (Fig. 1).
Type 2 diabetes remission at postoperative 3, 6, and 9 years according to five DP score intervals in the training and validation cohorts. A significant association was observed between T2D remission rates assessed at each follow-up point and the DP score, and this association was sustained for 9 years after surgery, with statistical significance (Cochran–Armitage test, P value < 0.001 at all follow-up points in both cohorts). T2D type 2 diabetes, DP diabetes prediction
Discussion
T2D remission after gastrectomy for cancer has been reported, mostly in single-center studies [8,9,10, 16,17,18, 29, 30]; however, there is still a paucity of large-scale studies investigating which patients will achieve postoperative T2D remission. A Taiwanese nationwide study showed that T2D remission after total gastrectomy for cancer was significantly associated with age, insulin use, and the presence of liver cirrhosis [31]; however, the statistical model was not adjusted for sufficient preoperative variables and could not suggest the personalized likelihood of T2D remission after gastrectomy for cancer. This study is the first to predict individualized T2D remission after gastric cancer surgery. We established a comprehensive prediction model and demonstrated a significant association between preoperative variables such as antidiabetic medications, baseline BMI, and the extent of gastrectomy and T2D remission after gastric cancer surgery; we used these associations to formulate the DP scores, which we believe will enable the personalized prediction for postoperative T2D remission. We adopted the best-in-class machine-learning approaches and found that the DP scores showed comparable predictive performances in the training and validation cohorts.
The study population included patients who survived > 3 years after gastric cancer surgery, and > 80% of the included patients did not receive adjuvant chemotherapy (Table 1). Considering that chemotherapy is administered to 94.4% of patients with stage II or III gastric cancer in Korea [32], approximately 80% of the investigated study population was thought to be patients with stage I gastric cancer, which shows a 5-year survival rate of > 90% in Korea. The number of long-term gastric cancer survivors has increased, and the management of chronic disease in these patients in the field of oncology, has been highlighted. The DP score is a simple scoring system that identifies the patients who are expected to experience diabetes remission. It is recommended that physicians should educate patients with regard to the self-monitoring of blood glucose and their responses to hypoglycemic events, concepts of diabetes remission after gastrectomy, and the necessity of extra hospital visits rather than regular follow-ups for antidiabetic medication control.
Defects in the beta-cell function are key prognostic factors for the progression of T2D [33] and important predictors of T2D remission after other gastrointestinal surgeries, such as bariatric surgery [34]. Among the five predictors included in the DP score, four (BMI, age, FPG, and number of antidiabetic medications) were directly or indirectly associated with the severity of T2D and residual function of the pancreatic beta-cells [35,36,37]. In addition, we investigated various kinds of antidiabetic medications and found that the non-use of sulfonylureas exhibited the strongest association with a high likelihood of T2D remission (OR 4.16; 95% CI 3.45–5.03; Supplementary Table 2), in contrast to a previous study that reported that the non-use of insulin was a strong predictor of T2D remission [31]. Although the exact mechanisms remain unclear, the distinctive association between the use of sulfonylurea and T2D remission after gastric cancer may be explained by the detrimental effects of the prolonged stimulation of insulin secretion from the beta-cells [38, 39], which may have resulted in the apoptoses of the beta-cells [40, 41], thereby limiting T2D remission after surgery. In the same context, use of insulin allowed the beta-cells to rest, which would explain the more advantageous effects of the use of insulin on T2D remission after gastric cancer surgery, compared with the use of sulfonylureas [38].
The DP scores predicted a higher T2D remission rate after total gastrectomy than after subtotal gastrectomy. The extent of gastrectomy may have contributed to the differences in postoperative weight loss [42] and decrease in ghrelin levels. Ghrelin is secreted by enteroendocrine cells located in the fundus of the stomach and is associated with insulin sensitivity [43, 44]. In addition, Roux-en-Y reconstructions are performed after total gastrectomy, while Billroth I or Billroth II reconstruction is usually performed after subtotal gastrectomy. Since the Roux-en-Y reconstruction is known to be superior to Billroth I or II reconstruction in terms of T2D remission [45], the difference in the reconstruction methods might also contribute to the higher T2D remission rate after total gastrectomy than after subtotal gastrectomy.
Machine-learning approaches have shown better performances than conventional modeling when applied to various medical conditions, including the prediction of T2D [46, 47]. Although the DP score comprises only five variables that can be obtained easily, it showed a predictive performance equivalent to models using machine-learning methods that were trained with many features. Given that machine-learning approaches have limitations with respect to practicality and cost-effectiveness in various clinical settings, the DP score can be a useful predictive tool for T2D remission with a high predictive performance and feasibility.
Our study has some limitations. First, the limited availability of laboratory measurements (e.g., oral glucose tolerance test and glycated hemoglobin) in the NHIS claims database did not allow for statistical adjustments according to the T2D severity. Nonetheless, indirect variables, including antidiabetic medications and FPG, which are easily accessible in primary care settings, were included to reflect the T2D severity and to efficiently predict the T2D remission rate. Second, misclassification of T2D remission cannot be ruled out. While we defined T2D remission according to the use of medication, some antidiabetic medications (e.g., metformin) may be recommended and prescribed in the remitted T2D state. In addition, there are concerns arising from the absence of information on biochemical assessments when defining T2D remission. Sensitivity analyses assessing the significance of the multivariate analyses according to the different T2D remission definitions showed that the predictors’ effect on T2D remission remained significant regardless of the definition of T2D that was used (Supplementary Table 3). Third, the NHIS database update in 2008 regarding the definition of some variables may have contributed to the heterogeneity of the cohort of patients undergoing gastrectomy before and after 2008. We performed a sensitivity analysis for patients undergoing gastric cancer surgery before 2008 and observed that the predictors for T2D remission remained significant (Supplementary Table 4). Fourth, to assess the status of T2D medications during the follow-up period, we used the claims for the prescription of medications, which do not necessarily equate to actual use of medication. Fifth, owing to the paucity of information in the NHIS claims data, we did not compare the different surgical reconstruction methods (e.g., Billroth I or II, Roux-en-Y) after gastrectomy for cancer. Given the consistently higher T2D remission rate after total gastrectomy compared with subtotal gastrectomy, regardless of the reconstruction methods used, the reconstruction methods may have had minimal effects on our model. Sixth, because the study population was limited to Korean individuals, further validation studies involving patients of other ethnicities or nationalities should be considered.
Conclusions
We developed and validated a DP score that is easy to use and enables the stratification of patients with gastric cancer based on the probability of T2D remission after gastrectomy. The DP score yielded a comparable performance to the machine-learning models, and its predictive performance persisted in the prediction of T2D remission until 9 years after surgery. We expect our results to help healthcare professionals to preoperatively predict the probability of T2D remission and to provide personalized T2D management for patients who undergo gastric cancer surgery.
References
van Gestel YR, Lemmens VE, de Hingh IH, Steevens J, Rutten HJ, Nieuwenhuijzen GA, et al. Influence of comorbidity and age on 1-, 2-, and 3 month postoperative mortality rates in gastrointestinal cancer patients. Ann Surg Oncol. 2013;20:371–80.
Koppert LB, Janssen-Heijnen ML, Louwman MW, Lemmens VE, Wijnhoven BP, Tilanus HW, et al. Comparison of comorbidity prevalence in oesophageal and gastric carcinoma patients: a population-based study. Eur J Gastroenterol Hepatol. 2004;16:681–8.
Wang JB, Zheng CH, Li P, Xie JW, Lin JX, Lu J, et al. Effect of comorbidities on postoperative complications in patients with gastric cancer after laparoscopy-assisted total gastrectomy: results from an 8 year experience at a large-scale single center. Surg Endosc. 2017;31:2651–60.
Currie CJ, Poole CD, Jenkins-Jones S, Gale EA, Johnson JA, Morgan CL. Mortality after incident cancer in people with and without type 2 diabetes: impact of metformin on survival. Diabetes Care. 2012;35:299–304.
Barone BB, Yeh HC, Snyder CF, Peairs KS, Stein KB, Derr RL, et al. Long-term all-cause mortality in cancer patients with preexisting diabetes mellitus: a systematic review and meta-analysis. JAMA. 2008;300:2754–64.
Tseng CH. Diabetes conveys a higher risk of gastric cancer mortality despite an age-standardised decreasing trend in the general population in Taiwan. Gut. 2011;60:774–9.
Lee CK, Jung M, Jung I, Heo SJ, Jeong YH, An JY, et al. Cumulative metformin use and its impact on survival in gastric cancer patients after gastrectomy. Ann Surg. 2016;263:96–102.
Lee TH, Lee CM, Park S, Jung DH, Jang YJ, Kim JH, et al. Long-term follow-up for type 2 diabetes mellitus after gastrectomy in non-morbidly obese patients with gastric cancer: the legitimacy of onco-metabolic surgery. J Gastric Cancer. 2017;17:283–94.
Lanzarini E, Csendes A, Lembach H, Molina J, Gutiérrez L, Silva J. Evolution of type 2 diabetes mellitus in non morbid obese gastrectomized patients with Roux en-Y reconstruction: retrospective study. World J Surg. 2010;34:2098–102.
Zervos EE, Agle SC, Warren AJ, Lang CG, Fitzgerald TL, Dar M, et al. Amelioration of insulin requirement in patients undergoing duodenal bypass for reasons other than obesity implicates foregut factors in the pathophysiology of type II diabetes. J Am Coll Surg. 2010;210:564–72.
Hansen EN, Tamboli RA, Isbell JM, Saliba J, Dunn JP, Marks-Shulman PA, et al. Role of the foregut in the early improvement in glucose tolerance and insulin sensitivity following Roux-en-Y gastric bypass surgery. Am J Physiol Gastrointest Liver Physiol. 2011;300:G795–802.
Bae JM, Park JW, Yang HK, Kim JP. Nutritional status of gastric cancer patients after total gastrectomy. World J Surg. 1998;22:254–61.
Allum WH, Blazeby JM, Griffin SM, Cunningham D, Jankowski JA, Wong R. Guidelines for the management of oesophageal and gastric cancer. Gut. 2011;60:1449–72.
Songun I, Putter H, Kranenbarg EM, Sasako M, van de Velde CJ. Surgical treatment of gastric cancer: 15 year follow-up results of the randomised nationwide Dutch D1D2 trial. Lancet Oncol. 2010;11:439–49.
Kim JW, Cheong JH, Hyung WJ, Choi SH, Noh SH. Outcome after gastrectomy in gastric cancer patients with type 2 diabetes. World J Gastroenterol. 2012;18:49–54.
An JY, Kim YM, Yun MA, Jeon BH, Noh SH. Improvement of type 2 diabetes mellitus after gastric cancer surgery: short-term outcome analysis after gastrectomy. World J Gastroenterol. 2013;19:9410–7.
Kwon Y, Abdemur A, Lo Menzo E, Park S, Szomstein S, Rosenthal RJ. The foregut theory as a possible mechanism of action for the remission of type 2 diabetes in low body mass index patients undergoing subtotal gastrectomy for gastric cancer. Surg Obes Relat Dis. 2014;10:235–42.
Lee W, Ahn SH, Lee JH, Park DJ, Lee HJ, Kim HH, et al. Comparative study of diabetes mellitus resolution according to reconstruction type after gastrectomy in gastric cancer patients with diabetes mellitus. Obes Surg. 2012;22:1238–43.
Cheol Seong S, Kim YY, Khang YH, Heon Park J, Kang HJ, Lee H, et al. Data resource profile: the national health information database of the national health insurance service in South Korea. Int J Epidemiol. 2017;46:799–800.
Buse JB, Caprio S, Cefalu WT, Ceriello A, Del Prato S, Inzucchi SE, et al. How do we define cure of diabetes? Diabetes Care. 2009;32:2133–5.
Captieux M, Prigge R, Wild S, Guthrie B. Defining remission of type 2 diabetes in research studies: a systematic scoping review. PLoS Med. 2020;17:e1003396.
American Diabetes Association. 6. Glycemic targets: standards of medical care in diabetes–2021. Diabetes Care. 2021;44:S73–84.
Mandrekar JN. Receiver operating characteristic curve in diagnostic test assessment. J Thorac Oncol. 2010;5:1315–6.
Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143:29–36.
Tibshirani R. The lasso method for variable selection in the Cox model. Stat Med. 1997;16:385–95.
Chen T, Guestrin C. XGBoost: a scalable tree boosting system. In: Proceeding 22nd ACM SIGKDD international conference on knowledge discovery and data mining. 2016. p. 785–94.
Breiman L. Random forests. Mach Learn. 2001;45:5–32.
World Health Organisation, International Association for the Study of Obesity, International Obesity TaskForce. The Asia-Pacific perspective: redefining obesity and its treatment. Melbourne: Health Communications, Australia Pty Ltd; 2000.
Yang J, Li C, Liu H, Gu H, Chen P, Liu B. Effects of subtotal gastrectomy and Roux-en-Y gastrojejunostomy on the clinical outcome of type 2 diabetes mellitus. J Surg Res. 2010;164:e67–71.
Wang KC, Huang KH, Lan YT, Fang WL, Lo SS, Li AF, et al. Outcome after curative surgery for gastric cancer patients with type 2 diabetes. World J Surg. 2014;38:431–8.
Ho TW, Wu JM, Yang CY, Lai HS, Lai F, Tien YW. Total gastrectomy improves glucose metabolism on gastric cancer patients: a nationwide population-based study. Surg Obes Relat Dis. 2016;12:635–41.
Health Insurance Review and Assessment Service. National healthcare quality report for the gastric cancer in 2014 (in Korean). https://www.hira.or.kr/cms/open/04/04/12/2015_09.pdf. Accessed June 2021.
Kahn SE. Clinical review 135: The importance of beta-cell failure in the development and progression of type 2 diabetes. J Clin Endocrinol Metab. 2001;86:4047–58.
Souteiro P, Belo S, Neves JS, Magalhães D, Silva RB, Oliveira SC, et al. Preoperative beta cell function is predictive of diabetes remission after bariatric surgery. Obes Surg. 2017;27:288–94.
Chiu KC, Lee NP, Cohan P, Chuang LM. Beta cell function declines with age in glucose tolerant Caucasians. Clin Endocrinol (Oxf). 2000;53:569–75.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Yoon KH, Ko SH, Cho JH, Lee JM, Ahn YB, Song KH, et al. Selective beta-cell loss and alpha-cell expansion in patients with type 2 diabetes mellitus in Korea. J Clin Endocrinol Metab. 2003;88:2300–8.
van Raalte DH, Verchere CB. Improving glycaemic control in type 2 diabetes: stimulate insulin secretion or provide beta-cell rest? Diabetes Obes Metab. 2017;19:1205–13.
Kahn SE, Haffner SM, Heise MA, Herman WH, Holman RR, Jones NP, et al. Glycemic durability of rosiglitazone, metformin, or glyburide monotherapy. N Engl J Med. 2006;355:2427–43.
Maedler K, Carr RD, Bosco D, Zuellig RA, Berney T, Donath MY. Sulfonylurea induced beta-cell apoptosis in cultured human islets. J Clin Endocrinol Metab. 2005;90:501–6.
Takahashi A, Nagashima K, Hamasaki A, Kuwamura N, Kawasaki Y, Ikeda H, et al. Sulfonylurea and glinide reduce insulin content, functional expression of K(ATP) channels, and accelerate apoptotic beta-cell death in the chronic phase. Diabetes Res Clin Pract. 2007;77:343–50.
Davis JL, Selby LV, Chou JF, Schattner M, Ilson DH, Capanu M, et al. Patterns and predictors of weight loss after gastrectomy for cancer. Ann Surg Oncol. 2016;23:1639–45.
Jeon TY, Lee S, Kim HH, Kim YJ, Son HC, Kim DH, et al. Changes in plasma ghrelin concentration immediately after gastrectomy in patients with early gastric cancer. J Clin Endocrinol Metab. 2004;89:5392–6.
Soleyman-Jahi S, Abdirad A, Fallah AA, Ghasemi S, Sadeghi F, Heidari R, et al. Prognostic significance of preoperative and postoperative plasma levels of ghrelin in gastric cancer: 3-year survival study. Clin Transl Gastroenterol. 2017;8:e209.
Choi YY, Noh SH, An JY. A randomized controlled trial of Roux-en-Y gastrojejunostomy vs. gastroduodenostomy with respect to the improvement of type 2 diabetes mellitus after distal gastrectomy in gastric cancer patients. PLoS One. 2017;12:e0188904.
Anderson AE, Kerr WT, Thames A, Li T, Xiao J, Cohen MS. Electronic health record phenotyping improves detection and screening of type 2 diabetes in the general United States population: a cross-sectional, unselected, retrospective study. J Biomed Inform. 2016;60:162–8.
Taylor RA, Pare JR, Venkatesh AK, Mowafi H, Melnick ER, Fleischman W, et al. Prediction of in-hospital mortality in emergency department patients with sepsis: a local big data-driven, machine learning approach. Acad Emerg Med. 2016;23:269–78.
Acknowledgements
None.
Funding
This work was supported by the Korea Medical Device Development Fund grant funded by the Korean government (the Ministry of Science and ICT, Ministry of Trade, Industry and Energy, Ministry of Health & Welfare, and Ministry of Food and Drug Safety) (Project Number: 9991007295, KMDF_PR_202012D13-02) (for S.P.), and Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Education (2020R1I1A1A01070106) (for Y.K.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kwon, Y., Kwon, JW., Ha, J. et al. Remission of type 2 diabetes after gastrectomy for gastric cancer: diabetes prediction score. Gastric Cancer 25, 265–274 (2022). https://doi.org/10.1007/s10120-021-01216-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-021-01216-2