Abstract
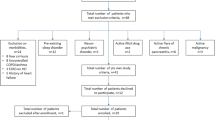
The incidence of sleep problems is increasing in children, and they are thought to contribute to pain in functional abdominal pain disorder (FAPD). In this study, we aimed to evaluate the pattern of sleep disturbance in children with FAPD and identify the associated factors. We retrospectively analyzed patients aged 12–18 years who were diagnosed with FAPD based on the Rome IV criteria. To assess sleep problems, we used the Korean version of the Pittsburgh Sleep Quality Index (PSQI-K). To evaluate factors associated with sleep disturbances, we used the odds ratios (OR) estimated in logistic regression models. Among the 66 patients evaluated, 57.6% (38/66) had a total PSQI-K score > 5, indicating a significant disturbance in sleep, 52.6% (20/38) had irritable bowel syndrome (IBS), and 47.4% (18/38) had functional abdominal pain-not otherwise specified. The mean PSQI-K score was 7.2 ± 6.0, and longer sleep onset latency was noted (26.33 ± 19.44 min) in all patients than healthy controls. Almost all PSQI-K subscales scores were elevated in patients with IBS. In univariate analysis, abdominal pain score > 7 and IBS were associated with poor sleep quality. In multivariate analysis, only IBS was associated with sleep disturbance. A relatively large proportion of patients with FAPD had sleep problems and these were more common in patients with IBS. Thus, interventions for improving sleep quality should also be considered in patients with FAPD with severe abdominal pain and IBS.
Similar content being viewed by others
References
Korterink J, Devanarayana NM, Rajindrajith S, Vlieger A, Benninga MA. Childhood functional abdominal pain: mechanisms and management. Nat Rev Gastroenterol Hepatol. 2015;12:159–71.
Drossman DA. Functional gastrointestinal disorders: history, pathophysiology, clinical features, and Rome IV. Gastroenterology. 2016;150:1262–79.
Farmer AD, Aziz Q. Gut pain and visceral hypersensitivity. Br J Pain. 2013;7:39–47.
Faure C, Thapar N, Di Lorenzo C. Pediatric neurogastroenterology: gastrointestinal motility and functional disorders in children. New York: Springer; 2016.
Devanarayana NM, Mettananda S, Liyanarachchi C, et al. Abdominal pain–predominant functional gastrointestinal diseases in children and adolescents: prevalence, symptomatology, and association with emotional stress. J Pediatr Gastroenterol Nutri. 2011;53:659–65.
Newton E, Schosheim A, Patel S, Chitkara DK, van Tilburg MA. The role of psychological factors in pediatric functional abdominal pain disorders. Neurogastroenterol Motil. 2019;31:e13538.
Kim SY, Choung RS, Lee SK, et al. Self-reported sleep impairment in functional dyspepsia and irritable bowel syndrome. J Neurogastroenterol Motil. 2018;24:280–8.
Huntley ED, Campo JV, Dahl RE, Lewin DS. Sleep characteristics of youth with functional abdominal pain and a healthy comparison group. J Pediatr Psychol. 2007;32:938–49.
Long AC, Krishnamurthy V, Palermo TM. Sleep disturbances in school-age children with chronic pain. J Pediatr Psychol. 2008;33:258–68.
Schurman JV, Friesen CA, Dai H, Danda CE, Hyman PE, Cocjin JT. Sleep problems and functional disability in children with functional gastrointestinal disorders: an examination of the potential mediating effects of physical and emotional symptoms. BMC Gastroenterol. 2012;12:142.
Al-Khani AM, Sarhandi MI, Zaghloul MS, Ewid M, Saquib N. A cross-sectional survey on sleep quality, mental health, and academic performance among medical students in Saudi Arabia. BMC Res Notes. 2019;12:665.
Patel A, Hasak S, Cassell B, et al. Effects of disturbed sleep on gastrointestinal and somatic pain symptoms in irritable bowel syndrome. Aliment Pharmacol Ther. 2016;44:246–58.
Hyams JS, Di Lorenzo C, Saps M, Shulman RJ, Staiano A, van Tilburg M. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology. 2016;150:1456–68.
Laird KT, Sherman AL, Smith CA, Walker LS. Validation of the abdominal pain index using a revised scoring method. J Pediatr Psychol. 2015;40:517–25.
Karcioglu O, Topacoglu H, Dikme O, Dikme O. A systematic review of the pain scales in adults: which to use? Am J Emerg Med. 2018;36:707–14.
Sohn SI, Kim DH, Lee MY, Cho YW. The reliability and validity of the Korean version of the Pittsburgh Sleep Quality Index. Sleep Breath. 2012;16:803–12.
Luca G, Peris L. Sleep quality and sleep disturbance perception in dual disorder patients. J Clin Med. 2020;9:2015.
Carter KA, Hathaway NE, Lettieri CF. Common sleep disorders in children. Am Fam Physician. 2014;89:368–77.
Abdulahad S, Huls H, Balikji S, van de Loo AJ, Roth T, Verster JC. Irritable bowel syndrome, immune fitness, and insomnia: results from an online survey among people reporting sleep complaints. Sleep Vigilance. 2019;3:121–9.
Owens J. Classification and epidemiology of childhood sleep disorders. Prim Care. 2008;35:533–46.
Wang B, Duan R, Duan L. Prevalence of sleep disorder in irritable bowel syndrome: a systematic review with meta-analysis. Saudi J gastroenterol. 2018;24:141–50.
Wu S, Chen S, Zhao Y, Ma X, Wang R, He J. Association between excessive daytime sleepiness and functional gastrointestinal disorders: a population-based study in China. J Neurogastroenterol Motil. 2017;23:298–305.
Tu Q, Heitkemper M, Jarrett M, Buchanan D. Sleep disturbances in irritable bowel syndrome: a systematic review. Neurogastroenterol Motil. 2017;29:e12946.
Kennedy P, Cryan J, Quigley E, Dinan T, Clarke G. A sustained hypothalamic–pituitary–adrenal axis response to acute psychosocial stress in irritable bowel syndrome. Psychol Med. 2014;44:3123–34.
Fass R, Fullerton S, Tung S, Mayer EA. Sleep disturbances in clinic patients with functional bowel disorders. Am J Gastroenterol. 2000;95:1195–200.
Rhie S, Chae KY. Effects of school time on sleep duration and sleepiness in adolescents. PLoS ONE. 2018;13:e0203318.
Pan F, Tian J, Cicuttini F, Jones G. Sleep disturbance and its association with pain severity and multisite pain: a prospective 10.7-Year study. Pain Ther. 2020;9:751–63.
Nojkov B, Rubenstein JH, Chey WD, Hoogerwerf WA. The impact of rotating shift work on the prevalence of irritable bowel syndrome in nurses. Am J Gastroenterol. 2010;105:842–7.
Vandekerckhove M, Wang Y-L. Emotion, emotion regulation and sleep: an intimate relationship. AIMS Neurosci. 2018;5:1–17.
Acknowledgements
There are no additional acknowledgments associated with this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The funding organization(s) played no role in the study design, collection, analysis, and interpretation of data, writing of the report, or decision to submit the report for publication.
Ethical committee permission
This retrospective analysis was approved by the Institutional Review Board of Chungnam National University Hospital and conducted in accordance with principles of the Declaration of Helsinki.
Research involving human participants and/or animals
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, H.J. Importance of sleep quality in functional abdominal pain disorder in pediatric patients. Sleep Biol. Rhythms 20, 81–85 (2022). https://doi.org/10.1007/s41105-021-00342-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-021-00342-9