Abstract
Background
Antiarrhythmic drugs are often used in the management of patients with atrial fibrillation (AF). Sotalol is conventionally initiated in the inpatient setting for monitoring efficacy and adverse effects, including QTc interval prolongation and torsades de pointes (TdP) proarrhythmia.
Objective
We aimed to evaluate the efficacy and safety of outpatient initiation of sotalol for the treatment of AF in a select group of patients with cardiac implantable electronic devices (CIEDs): permanent pacemakers (PPMs), implantable cardioverter defibrillators (ICDs), and implantable loop recorders (ILRs) capable of continuous rhythm monitoring remotely.
Methods
We conducted our clinical study in a real-world practice setting with longitudinal follow-up of the study cohort. We included adult patients with symptomatic paroxysmal and persistent AF eligible for sotalol for rhythm control strategy and who had CIEDs in our study. Patients with a known contraindication to sotalol were excluded. After making a shared management decision with patients, sotalol was initiated as an outpatient, with regular clinical encounters with patients to assess the efficacy and safety of treatment, and monitoring cardiac rhythm and QTc intervals with CIEDs utilizing their remote monitoring platforms.
Results
The study cohort comprised 105 patients; 38 (36%) females, mean age ± standard deviation (SD) 73.9 ± 10.36 years, and with a CHA2DS2-VASc score of 3.26 ± 1.37 and left ventricular ejection fraction of 60.16 ± 9.10%. Twenty-six (24.8%) patients were implanted with PPMs, 10 (9.5%) with dual-chamber ICDs, and 69 (65.7%) with ILRs. Over a follow-up period of 23 ± 15 months, sotalol was continued at a steady median dose of 80 mg twice daily, 105 ± 42 mg (mean ± SD) in 77 (73%) patients who maintained sinus rhythm, and discontinued in 28 (27%) patients because of inefficacy or development of adverse effects. No adverse effects relating to QTc prolongation and TdP or mortality were observed during the study period.
Conclusions
Effective and safe outpatient initiation and maintenance of sotalol therapy is possible in select patients who have CIEDs for continuous remote monitoring and surveillance capabilities.
Similar content being viewed by others
Sotalol is conventionally initiated in the inpatient setting for monitoring efficacy and adverse effects, including QTc interval prolongation and torsades de pointes (TdP) proarrhythmia. |
We aimed to evaluate the efficacy and safety of outpatient initiation of sotalol for the treatment of atrial fibrillation (AF) in a select group of patients with cardiac implantable electronic devices (CIEDs) capable of continuous rhythm monitoring remotely. |
Over a long follow-up period, sotalol was continued at a steady dose in the majority of patients who were able to maintain sinus rhythm. No adverse effects relating to QTc prolongation and TdP or mortality were observed in these patients. |
Effective and safe outpatient initiation and maintenance of sotalol therapy is possible in select patients who have CIEDs for continuous remote monitoring and surveillance capabilities. |
1 Introduction
With increasing numbers of patients with atrial fibrillation (AF) worldwide, the focus on early intervention for rhythm control has grown [1, 2]. Rhythm-control strategies are designed to maintain sinus rhythm (SR), reduce the frequency and duration of AF, and improve quality of life [1, 2]. Antiarrhythmic drugs (AADs) are often used in the management of patients with AF. Sotalol, commercially available in its racemic mixture of d and l isomers, has been extensively studied in both basic science experiments and clinical trials. While the d isomer as a class III effect prolongs repolarization by blocking the rapid component of the delayed rectifier potassium current (IKr) and prolongs action potential duration and refractory period throughout the heart and QT interval on the surface electrocardiogram (ECG), the l isomer, along with prolonging repolarization, bears nonselective β-blocking properties. Since the maximal potassium current blocking effect occurs when the heart rate is slow, sotalol is not effective in converting AF to SR, but rather prevents occurrence of AF usually initiated by premature atrial depolarization complexes. The ‘reverse use-dependence’ effect of sotalol could thus promote early-after depolarization-related triggered polymorphic ventricular tachyarrhythmias (VT), i.e. torsades de pointes (TdP), a proarrhythmia that is observed along with QT prolongation. The superior efficacy of sotalol for the prevention of recurrent VT, and the fact that it did not cause increased mortality in patients with ischemic cardiomyopathy, unlike class I AADs, was the basis for the approval of sotalol for clinical use, as well as marketing for the treatment of VT, with further approval for the treatment of AF in the early 90s and an injectable form in 2009 [3,4,5,6]. The package inserts for the commercial products of sotalol contain black-box warnings regarding the potential for QT prolongation and VT, such that initiating and re-initiating sotalol in an inpatient monitoring setting is conventionally recommended. However, since proarrhythmia related to sotalol is dose-dependent rather than idiosyncratic, and can be prevented by monitoring the QT interval, many practicing clinicians often question the strategy of hospitalization. Some experts would initiate sotalol in hospital in the absence of implantable cardioverter defibrillators (ICDs) [1]. Such practice may be further supported by observations made in the study by Chung et al. that the only significant predictor of arrhythmia complications in patients admitted for sotalol initiation was the absence of a permanent pacemaker (PPM) in these patients [7]. As the field of AF management has evolved over years, it is not uncommon for many patients with AF to have cardiac implantable electronic devices (CIEDs), i.e. PPMs, ICDs, and implantable loop recorders (ILRs). Those patients with PPMs and ICDs who are vulnerable to developing significant bradycardia would be expected to better tolerate sotalol by virtue of cardiac pacing. The modern contemporary CIEDs are capable of recording intracardiac electrograms and single to multichannel ECG tracings that may be downloaded and printed offline for accurate measurements of cardiac event intervals, including the QT intervals. With their easy-to-operate technology for continuous rhythm monitoring remotely and with a high degree of sensitivity and specificity for accurate rhythm diagnosis, such devices would further allow early intervention, including prompt discontinuation or dose adjustment in sotalol in case of development of QT prolongation.
With the aforementioned premise, the purpose of this study was to assess the efficacy and safety of outpatient sotalol initiation in a select group of patients with AF who are implanted with CIEDs.
2 Methods
This was a longitudinal follow-up study conducted in a real-world practice setting. We performed a retrospective analysis of clinical data from patients with AF who were being treated with AADs for the maintenance of SR from January 2016 to September 2020. For inclusion in this study, patients needed to meet the following criteria: (1) age > 18 years; (2) documented paroxysmal or persistent AF; (3) left ventricular ejection function (LVEF) > 55%; (4) implanted with dual-chamber PPMs and ICDs or ILRs, or able to undergo implantation of these devices capable of continuous rhythm monitoring; (5) able to understand and perform CIED’s remote transmission; and (6) able to communicate, comprehend, take necessary instructions, and follow-up as needed.
Patients were excluded from the study for the following reasons: (1) known contraindication to sotalol; significant renal dysfunction, creatinine clearance < 40 mL/min, significant prolonged (> 450 ms) corrected QT (QTc) interval, and history of long QT syndromes; (2) taking any AADs; (3) bradycardia, heart rate < 60 beats per min (bpm) that was not able to be corrected; (4) single chamber ventricular PPMs and ICDs; (5) cognitive dysfunction; and (6) unable to provide informed consent. Furthermore, those patients with chronic permanent AF in whom, by definition, both the physicians and patients accept AF and only rate control strategy rather than persevere with the rhythm control measures were not included.
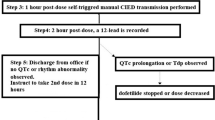
All patients had their renal function assessed prior to the initiation of sotalol. After discussing the benefits and risks of the drug, a shared decision treatment plan was developed. Upon approval of the plan by the patients, sotalol was initiated as an outpatient. A 12-lead ECG was obtained to establish a baseline. We programmed all PPMs and ICDs to provide a lower rate of atrial pacing at 70 bpm, with adequately long AV delays to also allow native ventricular conduction of the atrial beats. We programmed ILRs to detect a heart rate > 150 bpm for tachycardia, < 40 bpm for bradycardia, and pause for > 3 s, along with the manufacturers’ specific algorithms for the management of AF. A mandatory manual transmission was obtained from the patient’s CIED at 2 h post-sotalol dosing, and the QT interval was assessed from intracardiac electrograms and ECG tracings that were downloaded and printed offline. Patients were seen daily for the first 3 days, and thereafter at a minimum of once, or more frequently, at 1 week, 2 weeks, and 1 month after sotalol initiation in the office during which 12-lead ECGs were recorded. Patients were asked to bring their CIED monitors with them during their office visit, for interrogation of the CIEDs. On an individual case-by-case basis, patients were also instructed not to travel outside their residential area for at least 1–3 weeks during the monitoring period after starting sotalol. Patients were also advised to be prepared to seek emergency medical help, including 911 calls, and visit their local health care facility and physician’s office if necessary. Oral potassium and magnesium supplements were administered, both routinely and as needed, to patients who were receiving diuretics, as well as to other patients not receiving diuretics if the biochemistry tests showed low levels. Subsequent follow-ups were performed every 3–4 months. Baseline characteristics, laboratory data, and medical history, including ECG and CIED data specifically related to abnormal rhythm and QTc duration, were obtained from the electronic medical records. Medication history, including dose strengths and total number and adjustment of doses, discontinuations, and occurrence of arrhythmias and adverse effects were recorded.
Clinical endpoints of efficacy, adverse effects (including QTc prolongation, TdP, severe bradycardia and conduction block), and mortality, were assessed.
We observed the ethical standards of the study as per the 1975 Declaration of Helsinki. Each patient provided informed consent for the implantation of US FDA-approved CIEDs and their programming to implement guideline-based clinical practice. Institutional Review Board (IRB) approval was waived for retrospective analyses of the data.
Statistical analyses were performed on the data sets collected during follow-up. Categorical data are expressed as count (percentage), while continuous variables are expressed as median and mean ± standard deviation (SD) where appropriate. A one-way analysis of variance (ANOVA) test was used for comparison of intergroup differences of dosages between the three types of CIEDs. A p value < 0.05 was considered significant. Statistical analysis and data graphing were performed using OriginPro 2019b (OriginLab Corp., Northhampton, MA, USA).
3 Results
Of 196 patients presenting with AF and screened for inclusion in this study, 91 (46%) were excluded for various reasons: 57 patients with known contraindications to sotalol, 7 patients with a heart rate < 60 bpm that was not able to be corrected, 23 patients who had single-chamber ventricular PPMs and ICDs, and 4 patients with cognitive dysfunction or an inability to provide consent. In the remainder 105 (54%) patients deemed appropriate candidates for pharmacotherapy with sotalol, the drug was initiated as an outpatient and formed the study cohort (Fig. 1).
The age of the study cohort was 73.9 ± 10.36 years (mean ± SD) and included 38 (36%) females. The CHA2DS2-VASc score and LVEF were 3.26 ± 1.37 and 60.16 ± 9.10%, respectively. Ninety-four (89.5%) patients had hypertension, 31 (29.5%) patients had diabetes mellitus, 9 (8.6%) patients had heart failure, and 23 (21.9%) patients had vascular disease. The clinical characteristics of patients are provided in Table 1, and details of the concomitant use of potential QTc-prolonging drugs is given in Table 2. Twenty-six (24.8%) patients were implanted with PPMs, 10 (9.5%) patients were implanted with ICDs, and 69 (65.7%) patients were implanted with ILRs. Further details regarding the types of CIEDs in use among the cohort are provided in Table 3.
Patients were followed for 23 ± 15 months. The baseline QTc of 415 ± 32.56 ms and post-treatment QTc interval of 434.71 ± 40.31 ms at follow-up did not show a significant statistical difference (Fig. 2). Furthermore, no significant QTc prolongation occurred that mandated discontinuation of the drug.
Sotalol was initiated at doses of 40 mg twice daily in 11, 2, and 18 patients in the PPM, ICD, and ILR subgroups, respectively, and 80 mg twice daily in 15, 8, and 51 patients in the PPM, ICD, and ILR subgroups, respectively (Fig. 3). Sotalol was continued in 77 (73%) patients of the total cohort at a steady dose of 80 mg twice daily (median), 105 ± 42 mg (mean ± SD) who maintained SR, and discontinued in 28 (27%) patients because of inefficacy or the development of adverse effects. In the subgroups, the steady dose of sotalol was 91.32 ± 36.93 mg twice daily among patients with PPM, 108.66 ± 35.81 mg twice daily in patients with ICDs, and 87.78 ± 35.38 mg twice daily in patients with ILRs, with a median dose of 80 mg twice daily (Fig. 4). In the PPM subgroup, 8 patients were maintained on sotalol at a steady dose of 40 mg twice daily, 16 patients were receiving a steady dose of 80 mg twice daily, and two patients were receiving a steady dose of 160 mg twice daily. In the ICD subgroup, 8 patients were maintained at a steady dose of 80 mg twice daily and 2 patients were titrated to a steady dose of 160 mg twice daily. Finally, in the ILR subgroup, 28 patients were maintained on sotalol at a steady dose of 40 mg twice daily, 36 patients were receiving a steady dose of 80 mg twice daily, and 5 patients were titrated to a steady dose of 160 mg twice daily (Table 4). A one-way ANOVA test performed to compare intergroup variance of steady-state dosages between the three CIED subgroups showed no statistical significance (p = 0.24). In the subgroup of patients with dual-chamber PPMs and ICDs, we did not observe ventricular pacing, even during atrial paced rhythm at a steady dose of sotalol.
The dosage of sotalol was adjusted for uptitration when AF was not controlled, and, likewise, adjusted for downtitration when doing well, but on a relatively high dose or when the patient experienced bradycardia. Patients were receiving a steady dose of sotalol for 223.07 ± 293.78 days before a dose adjustment was made. In 28 (27%) patients, after 537.5 ± 442.06 days, sotalol was discontinued and patients switched to another AAD because they did not response to treatment and experienced breakthrough AF, or because they developed untenable adverse effects.
After initiating sotalol, 7 patients (7%) failed to convert to SR and therapy was discontinued. Sotalol was also discontinued in 2 patients (2%) who developed renal failure, 4 patients (4%) in the ILR subgroup who developed bradycardia that warranted drug discontinuation, 2 patients (2%) who experienced an unremittent adverse effect of persistent nausea, and, finally, 20 patients (19%) who experienced continued breakthrough AF. The latter group of patients who experienced breakthrough arrhythmias were receiving sotalol for 730.5 ± 437.27 days before its discontinuation; the reasons for discontinuation are shown in Table 5.
Throughout the study period, there were no incidents of exacerbation of heart failure, hospitalization, or mortality related to sotalol use or from AF.
No CIED malfunction or premature battery depletion due to continuous monitoring and mandatory manual transmissions was seen during the study duration.
4 Discussion
In our longitudinal clinical follow-up study performed in a real-world practice setting, we found that in the majority of patients (66%) we were able to safely initiate sotalol in an outpatient setting to maintain normal SR and monitor therapy long-term utilizing different CIEDs with equal variance of dosages. Furthermore, dose adjustment and discontinuation of sotalol after breakthrough of AF on steady state was needed in a minority of patients after a very long treatment period.
The practice of needing to initiate sotalol on an inpatient telemetry monitoring setting over a period of time has allowed outcome data regarding efficacy and safety to be gathered. In a study by Biswas et al., the data of 213 patients who were admitted to five hospitals in the US showed that over 90% were successfully discharged on sotalol without occurrence of any adverse event [8]. Absence of a dose adjustment was a strong predictor of successful initiation, with an odds ratio (OR) of 6.6 (95% confidence interval [CI] 1.3–32.7; p = 0.02). Hypertension, use of a calcium channel blocker, use of a separate β-blocker, and presence of a pacemaker were predictors of dose adjustments [8]; hence, in those patients in whom these factors are absent, sotalol may be initiated as an outpatient. The types of proarrhythmia related to sotalol, along with their risks and management, have been well-described [9]. Female sex, presenting with ventricular tachycardia or ventricular fibrillation, sotalol dosage > 320 mg/day, history of congestive heart failure, high serum creatinine, baseline prolonged QTc, and hypokalemia or hypomagnesemia correlate with predisposition to the development of TdP. These factors, along with the finding of a lower incidence of 1.8% of TdP at lower dosages, and a much higher incidence of up to 6.8% of TdP with dosages exceeding 640 mg/day, should help in appropriate patient selection [9]. Being a unique set-up of initiating sotalol in an outpatient setting, we intentionally used a protocol to start sotalol at the lowest possible dosage and achieved a steady maintenance dose of 80 mg twice daily. In a study conducted at a well-reputable tertiary academic medical center in the US, higher incidence of QTc prolongation and the need for more frequent therapy modifications were associated with inpatient sotalol initiation at higher and non-conventional dosages [10]. The key component of our protocol was remote surveillance of implanted CIEDs supplemented by regular office visits. Modern CIEDs have a greatly increased capacity to determine arrhythmic changes and report such changes quickly [11]. Remote monitoring technology also provides other necessary non-arrhythmia alerts, such as heart failure status, patients’ activity levels, battery status of the device, pacing, and integrity of the defibrillator leads, etc. [12]. Remote monitoring of CIEDs has become a normal and essential component of standard of care in patients with cardiac arrhythmias [13,14,15,16].
With CIED remote monitoring technology we were able to initiate dofetilide effectively and safely in an outpatient setting, in a small select group of patients, for the management of AF during strict and extenuating circumstances of the coronavirus disease 2019 (COVID-19) pandemic lockdown [17]. We have also previously reported the utility of the technology in optimizing AADs and anticoagulation therapy, including the safe withdrawal of long-term oral anticoagulation in some AF patients with a high risk of bleeding [18, 19].
It is also noteworthy that we were able to detect QTc prolongation using CIEDs at similar and comparable rates that have been observed in the real-world studies where conventional methods of QTc monitoring were used [20, 21]. Interestingly, we did not observe any TdP or other ventricular arrhythmias in our study population. In our study cohort, 34% of patients had dual-chamber PPM and ICD devices, which allowed us to maintain a higher heart rate with atrial pacing if necessary, to avoid bradycardia-related TdP.
The main limitation of our study was its retrospective design, small cohort size, and non-randomized design. Our study is essentially a longitudinal clinical observational study conducted in a real-world practice setting. Selection bias could not be ruled out as patients with single-chamber ventricular pacing were excluded on the premise of difficult and accurate assessment of QTc intervals in ventricular paced rhythm, and, furthermore, the possibility of the development of pacing-induced cardiomyopathy and deterioration of cardiac function. Although shared decision-making of initiating sotalol in an outpatient setting was taken with the patient, the discussion was initiated only after the patient’s refusal for hospitalization. The latter is not too uncommonly encountered in a real-world clinical practice setting. Furthermore, our study does not include the experience of using intravenous sotalol, which has gained approval for the treatment of various cardiac arrhythmias.
5 Conclusion
The results of our study show that in carefully selected patients with AF and implanted with CIEDs, outpatient sotalol may be safely initiated for rhythm control, and monitored and regulated long-term.
References
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, Conti JB, Ellinor PT, Ezekowitz MD, Field ME, Murray KT, Sacco RL, Stevenson WG, Tchou PJ, Tracy CM, Yancy CW, American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society [published erratum appears in J Am Coll Cardiol. 2014 Dec 2;64(21):2305-7]. J Am Coll Cardiol. 2014;64(21):e1-76. https://doi.org/10.1016/j.jacc.2014.03.022 (PMID: 24685669).
Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, Boriani G, Castella M, Dan GA, Dilaveris PE, Fauchier L, Filippatos G, Kalman JM, La Meir M, Lane DA, Lebeau JP, Lettino M, Lip GYH, Pinto FJ, Thomas GN, Valgimigli M, Van Gelder IC, Van Putte BP, Watkins CL, ESC Scientific Document Group. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2021;42(5):373–498. https://doi.org/10.1093/eurheartj/ehaa612.
Anderson JL, Prystowsky EN. Sotalol: an important new antiarrhythmic. Am Heart J. 1999;137(3):388–409. https://doi.org/10.1016/s0002-8703(99)70484-9.
BETAPACE/BETAPACE AF [prescribing info]. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/019865s021lbl.pdf
Batul SA, Gopinathannair R. Intravenous sotalol—reintroducing a forgotten agent to the electrophysiology therapeutic arsenal. J Atr Fibrillation. 2017;9(5):1499. https://doi.org/10.4022/jafib.1499.
Samanta R, Thiagalingam A, Turner C, Lakkireddy DJ, Kovoor P. The use of intravenous sotalol in cardiac arrhythmias. Heart Lung Circ. 2018;27(11):1318–26. https://doi.org/10.1016/j.hlc.2018.03.017.
Chung MK, Schweikert RA, Wilkoff BL, Niebauer MJ, Pinski SL, Trohman RG, Kidwell GA, Jaeger FJ, Morant VA, Miller DP, Tchou PJ. Is hospital admission for initiation of antiarrhythmic therapy with sotalol for atrial arrhythmias required? Yield of in-hospital monitoring and prediction of risk for significant arrhythmia complications. J Am Coll Cardiol. 1998;32(1):169–76. https://doi.org/10.1016/s0735-1097(98)00189-2.
Biswas M, Levy A, Weber R, Tarakji K, Chung M, Noseworthy PA, Newton-Cheh C, Rosenberg MA. Multicenter analysis of dosing protocols for sotalol initiation. J Cardiovasc Pharmacol Ther. 2020;25(3):212–8. https://doi.org/10.1177/1074248419887710.
Hohnloser SH. Proarrhythmia with class III antiarrhythmic drugs: types, risks, and management. Am J Cardiol. 1997;80(8A):82G-89G. https://doi.org/10.1016/s0002-9149(97)00717-0.
Ting C, Malloy R, Knowles D. Assessment of sotalol and dofetilide dosing at a large academic medical center. J Cardiovasc Pharmacol Ther. 2020;25(5):438–43. https://doi.org/10.1177/1074248420921740.
Zeitler EP, Piccini JP. Remote monitoring of cardiac implantable electronic devices (CIED). Trends Cardiovasc Med. 2016;26(6):568–77. https://doi.org/10.1016/j.tcm.2016.03.012.
Ploux S, Varma N, Strik M, Lazarus A, Bordachar P. Optimizing implantable cardioverter-defibrillator remote monitoring: a practical guide. JACC Clin Electrophysiol. 2017;3(4):315–28. https://doi.org/10.1016/j.jacep.2017.02.007.
Daoud EG, Glotzer TV, Wyse DG, Ezekowitz MD, Hilker C, Koehler J, Ziegler PD, TRENDS Investigators. Temporal relationship of atrial tachyarrhythmias, cerebrovascular events, and systemic emboli based on stored device data: a subgroup analysis of TRENDS. Heart Rhythm. 2011;8(9):1416–23. https://doi.org/10.1016/j.hrthm.2011.04.022.
Turakhia MP, Ziegler PD, Schmitt SK, Chang Y, Fan J, Than CT, Keung EK, Singer DE. Atrial fibrillation burden and short-term risk of stroke: case-crossover analysis of continuously recorded heart rhythm from cardiac electronic implanted devices. Circ Arrhythm Electrophysiol. 2015;8(5):1040–7. https://doi.org/10.1161/CIRCEP.114.003057.
Glotzer TV, Daoud EG, Wyse DG, Singer DE, Ezekowitz MD, Hilker C, Miller C, Qi D, Ziegler PD. The relationship between daily atrial tachyarrhythmia burden from implantable device diagnostics and stroke risk: the TRENDS study. Circ Arrhythm Electrophysiol. 2009;2(5):474–80. https://doi.org/10.1161/CIRCEP.109.849638.
Mascarenhas DA, Sharma M. Revisiting the role of antiarrhythmic drugs in prevention of atrial fibrillation recurrence: a single center retrospective review. Cardiol Res. 2018;9(3):165–70. https://doi.org/10.14740/cr724w.
Mascarenhas DAN, Mudumbi PC, Kantharia BK. Outpatient initiation of dofetilide: insights from the complexities of atrial fibrillation management during the COVID-19 lockdown. J Interv Card Electrophysiol. 2021. https://doi.org/10.1007/s10840-021-00942-y.
Mascarenhas DA, Farooq MU, Ziegler PD, Kantharia BK. Role of insertable cardiac monitors in anticoagulation therapy in patients with atrial fibrillation at high risk of bleeding. Europace. 2016;18(6):799–806. https://doi.org/10.1093/europace/euv350.
Mascarenhas DAN, Sharma M, Ziegler PD, Kantharia BK. Role of cardiovascular implantable electronic devices in delivering individualized disease-guided management of patients with non-valvular atrial fibrillation and high bleeding risk. Acta Cardiol. 2019;74(2):131–9. https://doi.org/10.1080/00015385.2018.1475029.
Anand V, Vakil K, Tholakanahalli V, Li JM, McFalls E, Adabag S. Discontinuation of dofetilide from QT prolongation and ventricular tachycardia in the real world. JACC Clin Electrophysiol. 2016;2(7):777–81. https://doi.org/10.1016/j.jacep.2016.05.007.
Yarlagadda B, Vuddanda V, Dar T, Jazayeri MA, Parikh V, Turagam MK, Lavu M, Avula SR, Atkins D, Bommana S, Gopinathannair R, Yeruva MR, Lakkireddy D. Safety and efficacy of inpatient initiation of dofetilide versus sotalol for atrial fibrillation. J Atr Fibrillation. 2017;10(4):1805. https://doi.org/10.4022/jafib.1805.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Daniel A. N. Mascarenhas, Praveen C. Mudumbi, and Bharat K. Kantharia declare they have no potential conflicts of interest that might be relevant to the contents of this manuscript.
Funding
No external funding was used for this study.
Ethics
The authors observed the ethical standards of the study as per the 1975 Declaration of Helsinki. Each patient gave informed consent for the implantation of FDA-approved CIEDs and their programming to implement guideline-based clinical practice. IRB approval was waived for retrospective analyses of the data.
Consent to participate and for publication
Not applicable.
Contributions
All authors have met the following authorship criteria: (1) substantial contributions to the conception and design, acquisition of data, or analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content; and (3) final approval of the version to be published. All authors take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation. Daniel A. N. Mascarenhas and Bharat K. Kantharia conceived and designed the research. All authors conducted the research, collected and analyzed the data, contributed to the writing of the manuscript, and read and approved the final version of the manuscript.
Data availability statement
This manuscript has no associated data that need deposition in a data repository. Furthermore, data sharing is not applicable to this article.
Rights and permissions
About this article
Cite this article
Mascarenhas, D.A.N., Mudumbi, P.C. & Kantharia, B.K. Outpatient Initiation of Sotalol in Patients with Atrial Fibrillation: Utility of Cardiac Implantable Electronic Devices for Therapy Monitoring. Am J Cardiovasc Drugs 21, 693–700 (2021). https://doi.org/10.1007/s40256-021-00493-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-021-00493-7