Abstract
Desmoplastic melanoma commonly occurs on the head and neck in a pure form, but occasionally, it occurs in a mixed tumor with another type, usually superficial spreading melanoma (SSM), and rarely as a metastasis from a primary SSM. We report here a primary SSM on the leg of a 32-year-old male which metastasised to lymph nodes, and 10 years later recurred at the primary site initially with mixed features but evolving to resemble a uniformly desmoplastic, deeply invasive melanoma. This unusual case has implications for clinical management and is additionally notable for its reversal in behavior, from metastatic to local infiltrative type, correlating with the change in morphology.
Similar content being viewed by others
Desmoplastic melanoma most commonly occurs on the head and neck as a poorly circumscribed dermal mass and tends to recur locally rather than metastasise [1]. It usually occurs in pure form but occasionally is seen as a desmoplastic component of a mixed tumor with the other element being a lentigo malignant melanoma (LMM) or superficial spreading melanoma (SSM) type and behavior then relates to the more aggressive component [2]. Very rarely a metastasis from SSM occurs as a desmoplastic lesion [3, 4]. We describe here a primary melanoma of clear SSM phenotype which metastasised to lymph nodes and showed in-transit metastases, but 10 years later recurred near the scar at the primary site with mixed conventional and desmoplastic features and then progressed to resemble a completely desmoplastic, deeply invasive melanoma at the original site. We believe it important to record this unusual case as it has implications for clinical management. In addition, we note that the reversal in aggressive behavior from metastatic to local infiltrative type was correlated with the change in morphology.
Case report
In 2005, a male aged 32 years was referred by his general practitioner to a plastic surgeon with a newly acquired pigmented lesion on the left calf suspected to be melanoma. This was excised and histologically diagnosed as SSM, 1.5-mm thick, with mitotic count 6/mm2. It was widely excised and sentinel node biopsy was performed. Two sentinel nodes from the left groin both contained a parenchymal metastasis 0.2 mm in maximum dimension. The melanoma was shown to have a BRAFV600E mutation.
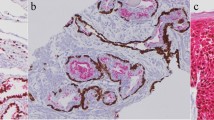
In the same year, 2005, the patient had six clinically benign moles on the mid- and upper back excised, one of which was histologically melanoma in situ. In 2008, three further pigmented lesions were removed from the left anterior calf, left lateral thigh, and left anterior shin. All were confirmed as benign junctional naevi, completely excised. However, in 2009, 4 years after diagnosis of the primary SSM, the patient found a nodule in the upper left popliteal fossa. Histology showed completely excised metastatic melanoma. In 2011, 6 years after diagnosis of the primary SSM, new pigmentation was noted adjacent to the original scar, and on excision was histologically diagnosed as a junctional naevus with dysplasia without a dermal component (Figs. 1, 2, 3).
The skin seen in Fig. 2 shows elongated spindle cells positive with S100
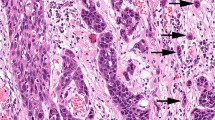
In 2015, 10 years after excision of the primary SSM on the calf, three subcutaneous nodules were identified near the original scar. On excision, these were shown to be recurrent melanoma with an epithelioid component similar to the original, but merging with a spindle cell desmoplastic component. The deeper spindle desmoplastic component was S100-positive but HMB45-negative, in contrast to the original melanoma which was HMB45-positive.
In August 2016, a further subcutaneous lesion was identified on the left calf underlying the previous scar. This was excised and described histologically as spindle cell recurrent melanoma. Ten months later in June 2017, and 12 years after diagnosis of the original primary SSM, another excision of a further subcutaneous lesion near the original scar showed merging of atypical spindle cells with scarring suggesting progression to desmoplastic melanoma. In April 2018, another nodule excised near the scar showed features of desmoplastic melanoma extending to the margins of the specimen. A further excision in May 2018 contained more desmoplastic melanoma still showing a BRAFV600E mutation, and this time appearing completely excised. In September 2020, the patient was referred to another hospital with intrathoracic lesions radiologically suspected as metastases. A biopsy was not proposed as the features were so highly consistent with metastatic melanoma.
Discussion
The histological interest of this case rests on the evolution over a 10-year period from primary SSM with nodal metastases to a spindle cell tumor with desmoplasia and without further metastasis but recurring locally with features of desmoplastic melanoma. The earlier metastases of epithelioid-type melanoma were to a groin node and an in-transit metastasis in the popliteal fossa. These were completely excised.
Ten years after the original excision, the tumor recurred in the original scar with mixed epithelioid and spindle cell features and this then recurred again with spindle/desmoplastic features 13 years after the original presentation. It had the infiltrative pattern of a desmoplastic melanoma and a further complete excision was achieved. No perineural invasion or neutropism was identified. Not only did the histological features change with time but also the pattern of growth also changed from metastatic to locally infiltrative, although it still retained a BRAF mutation which is unusual in desmoplastic melanoma. Their molecular features typically include NF1 mutations as well as in CBL, ERBB2, MAP2K1, and MAP3K1 [5,6,7]. It appears that this melanoma underwent metaplastic change to resemble desmoplastic melanoma and acquired the associated biological characteristics, but it retained the BRAF mutation and eventually has reverted to biological behavior more typical of SSM.
The rate of mutations is higher than in most other melanomas, and the majority are said to be related to ultraviolet radiation mutagenesis [5]. Whether this applies to the large minority of desmoplastic melanomas that arise on infrequently exposed anatomical sites remains to be established, as does the genetic signature in mixed desmoplastic and other melanoma types.
Data availability
Not applicable.
Code availability
Not applicable.
References
de Almeida LS et al (2008) Desmoplastic malignant melanoma: a clinicopathologic analysis of 113 cases. Am J Dermatopathol 30(3):207–215
George E et al (2009) Subclassification of desmoplastic melanoma: pure and mixed variants have significantly different capacities for lymph node metastasis. J Cutan Pathol 36(4):425–432
Busam KJ et al (2004) Cutaneous desmoplastic melanoma: reappraisal of morphologic heterogeneity and prognostic factors. Am J Surg Pathol 28(11):1518–1525
Scolyer RA, Thompson JF (2005) Desmoplastic melanoma: a heterogeneous entity in which subclassification as “pure” or “mixed” may have important prognostic significance. Ann Surg Oncol 12(3):197–199
Rabbie R et al (2019) Melanoma subtypes: genomic profiles, prognostic molecular markers and therapeutic possibilities. J Pathol 247(5):539–551
Kim J et al (2012) BRAF, NRAS and KIT sequencing analysis of spindle cell melanoma. J Cutan Pathol 39(9):821–825
Davison JM et al (2005) Absence of V599E BRAF mutations in desmoplastic melanomas. Cancer 103(4):788–792
Acknowledgements
The authors would like to thank Professor Richard Marais who helped to secure project funding and provided useful discussion throughout.
Funding
The work was supported by Cancer Research UK (Ref. C5759/A20971).
Author information
Authors and Affiliations
Contributions
All authors contributed to the data acquisition, conception, and writing, and gave final approval.
Corresponding author
Ethics declarations
Ethics approval
Approval was given by the Royal Surrey County Hospital Ethics Committee (07/Q190913).
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Martin G Cook and Barry W. E. M Powell are members of the EORTC Melanoma Group.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cook, M.G., Powell, B.W.E.M., Grant, M.E. et al. Evolution of superficial spreading melanoma to resemble desmoplastic melanoma: case report. Virchows Arch 480, 945–947 (2022). https://doi.org/10.1007/s00428-021-03127-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-021-03127-0