Abstract
Background
The time-to-isolation (TTI) may be a physiological predictor of durable isolations, and TTI-guided dosing strategies are widely performed in cryoballoon ablation. We sought to investigate the impact of the order of targeting the pulmonary veins (PVs) on the TTI values of left ipsilateral PVs.
Methods
This study included 144 atrial fibrillation patients who underwent PV isolations using 28-mm fourth-generation cryoballoons. In 101 patients, the left superior PV (LSPV) was targeted and followed by the left inferior PV (LIPV) (group 1), and the LIPV was targeted and followed by the LSPV in the remaining 43 (group 2).
Results
The total LSPV and LIPV freeze durations were 193 ± 60 and 171 ± 40 s, respectively. Real-time PV isolation monitoring was capable in 137 (95.1%) LSPVs and 119 (82.6%) LIPVs and in 112 (77.8%) patients (78 in group 1 and 34 in group 2) in both LSPVs and LIPVs. Among them, the LSPV TTI was significantly longer in group 1 than that in group 2 (54.8 ± 32.1 vs. 34.1 ± 17.3 s, p < 0.0001), while the LIPV TTI was significantly shorter in group 1 than that in group 2 (23.7 ± 11.8 vs. 39.2 ± 19.4 s, p < 0.0001). The ΔTTI ((TTI in LSPV)-(TTI in LIPV)) was significantly greater in group 1 than that in group 2 (31.1 ± 31.4 vs. − 5.0 ± 25.9 s, p < 0.0001). In 5 patients (3 in group 1 and 2 in group 2), initially targeted left PVs were not isolated despite complete vein occlusions, while they were by subsequent applications at the other ipsilateral PVs.
Conclusions
In CB ablation, the order of targeting PVs highly influenced the TTI of the left PVs owing to the presence of electrical connections between left ipsilateral PVs.
Similar content being viewed by others
1 Introduction
Cryoballoon (CB) pulmonary vein isolation (PVI) has already become established for catheter ablation of atrial fibrillation (AF). [1, 2] However, the optimal freeze dosing of cryoapplications is still under debate. Recent CB dosing protocols often incorporate the time-to-isolation (TTI), which denotes the elapsed time from the start of the cryoablation until an acute PVI. [3, 4] This is because an acute TTI seems to be a physiological predictor of a durable isolation and can be monitored in real time using the Achieve mapping catheter. On the contrary, it has been reported that the parameters predicting the PVI durability differ among the 4 pulmonary veins (PVs), and that the TTI is a strong predictor of the durability of the right superior PV (RSPV) but not the left PVs [5, 6]. The reasons have not been clarified.
Histological [7] and clinical studies [8,9,10] indicated the electrical connections between ipsilateral PVs, especially left ipsilateral PVs. In the segmental PVI, the electrical connections should have no impact on the procedure; however, in an ostial PVI, isolation of contiguous vessels is required to achieve a complete PVI because of the presence of inter-PV electrical connections. Actually, when the initial left superior PV (LSPV) application fails despite a complete occlusion using a 28-mm CB, both the LSPV and the left inferior PV (LIPV) are simultaneously isolated by a following LIPV application in approximately 40% of patients. [11] Based on these study results, we hypothesized that the TTI values depended on the order of targeting the PVs for left ipsilateral PVs. In this study, we investigated the impact of the order of targeting the PVs on the TTI values of left ipsilateral PVs.
2 Methods
2.1 Study population
This retrospective observational study consisted of 144 patients with paroxysmal and short-lasting persistent AF who underwent a PVI using a fourth-generation CB (Artic Front Advance PRO, Medtronic, Minneapolis, MN, USA) between August 2019 and December 2020. Among them, the LSPV was targeted and followed by the LIPV in 101 patients (group 1), and the LIPV was targeted and followed by the LSPV in 43 patients (group 2). In all patients, the PVI was performed exclusively with a 28-mm balloon and a single short freeze strategy without esophageal temperature monitoring. Patients with left common PVs were excluded from the study. AF was classified according to the latest guidelines. [1] All patients gave their written informed consent. The study protocol was approved by the hospital’s institutional review board. The study complied with the Declaration of Helsinki.
2.2 Mapping and ablation protocol
The surface electrocardiogram and bipolar intracardiac electrograms were continuously monitored and stored on a computer-based digital recording system (EP-WorkMate, St. Jude Medical, Minneapolis, MN, USA). The bipolar electrograms were filtered from 30 to 500 Hz. The procedure was performed under moderate sedation obtained with dexmedetomidine. A 100 IU/kg body weight of heparin was administered immediately following the venous access, and heparinized saline was additionally infused to maintain the activated clotting time at 300–350 s. A single transseptal puncture was performed using a radiofrequency needle (Baylis Medical, Inc., Montreal, QC, Canada) and 8-Fr long sheath (SL0, AF Division, St. Jude Medical). The transseptal sheath was exchanged over a guidewire for a 15-Fr steerable sheath (Flexcath Advance, Medtronic). Following the isolation of the right PVs (starting with right superior PV (RSPV) followed by right inferior PV (RIPV)), a single application was applied for the LSPV. Then, regardless of the TTI value of the LSPV (even if no LSPV isolation), a single application was applied for the LIPV in 101 patients (group 1). In the remaining 43 patients, a single application for the LIPV preceded the LSPV application (group 2). The order of targeting the left PVs was decided by the operators. A spiral mapping catheter (Achieve, Medtronic) was used to advance the 28-mm CB into the PV for support and to map the PV potentials. A 23-mm CB was not used in any cases. Following the verification of complete sealing with a contrast medium injection, a freeze cycle of maximal 180 s was applied. The basic freeze dose was 180 s for the upper PVs and 150–180 s for the lower PVs based on the nadir balloon temperature, TTI value, and patient’s body size. The quality of the initial freeze was evaluated within 60 s, and the second application was applied following the interruption of the initial application and balloon re-positioning if the initial freeze was considered an ineffective freeze. During the CB applications for the right PVs, the electromyography was monitored to anticipate phrenic nerve injury. If the balloon temperature reached − 60 °C or the amplitude of the electromyography significantly decreased, the freezing was terminated. The procedural endpoint was defined as an electrical PVI, and no bonus applications were performed after the isolation. Esophageal temperature monitoring was not performed in any cases.
2.3 Statistical analysis
Continuous data are expressed as the mean ± standard deviation for normally distributed variables or as the median (25th and 75th percentiles) for non-normally distributed variables, and were compared using a Student’s t-test or Mann–Whitney U-test, respectively. Categorical variables were compared using the chi-square test. A linear regression analysis was calculated to determine the relationship between 2 continuous variables. A probability value of p < 0.05 indicated statistical significance.
3 Results
3.1 Clinical characteristics and procedure results
The baseline patient characteristics are summarized in Table 1. The patient characteristics were similar between the 2 groups except for a higher proportion of persistent AF patients and larger LA size in group 1 than that in group 2. No patients had any PV anomalies.
In the 144 patients, a total of 576 PVs were identified. Overall, 570 of 576 (99.0%) PVs were isolated successfully using exclusively 28-mm CBs, while the remaining 6 (1.0%) PVs (1 LSPVs, 1 RSPVs, and 4 RIPVs) required touch-up ablation (Table 2). The gaps were located at the roof of the LSPV in 1 patient, postero-inferior RSPV in 1, posterior RIPV in 1, postero-superior RIPV in 1, and antero-superior RIPV in 2. The total number of CB applications was 1.2 ± 0.6, 1.2 ± 0.4, 1.2 ± 0.5, and 1.2 ± 0.6, and the total freeze duration (the sum of the freeze duration for each vein) was 193 ± 60, 171 ± 40, 189 ± 45, and 187 ± 68 s for the LSPV, LIPV, RSPV, and RIPV, respectively. The nadir balloon temperature was − 50.8 ± 5.1, − 45.5 ± 4.9, − 54.8 ± 4.9, and − 51.9 ± 6.4 °C for the LSPV, LIPV, RSPV, and RIPV, respectively. In 136 (94.4%) patients (94 in group 1 and 42 in group 2), the voltage map was created with a 3-D mapping system after the PVI, and the isolation of the left carina area was confirmed in all.
3.2 Electrical connections between the left ipsilateral PVs
Real-time PVI monitoring was capable in 137 (95.1%) LSPVs and 119 (82.6%) LIPVs (Table 2). The mean TTI was 49.0 ± 29.3 s and 28.8 ± 16.8 s in the LSPVs and LIPVs. In 5 patients (3 patients in group 1 and 2 patients in group 2), the initially targeted left PV was not isolated by a single cryoapplication despite a complete vein occlusion, while they were isolated by a subsequent application at the other ipsilateral PV. In the total population, the TTI at the LSPVs was significantly longer in group 1 than that in group 2 (55.7 ± 30.9 vs. 33.3 ± 16.7 s, p < 0.0001), while the TTI at the LIPVs was significantly shorter in group 1 than that in group 2 (24.0 ± 12.4 vs. 39.9 ± 20.2 s, p < 0.0001).
Real-time PVI monitoring of both the LSPV and the LIPV was capable in 112 (77.8%) patients. In the 112 patients (78 patients in group 1 and 34 patients in group 2), the TTI at the LSPVs was significantly longer in group 1 than that in group 2 (54.8 ± 32.1 vs. 34.1 ± 17.3 s, p < 0.0001) (Fig. 1A), while the TTI at the LIPVs was significantly shorter in group 1 than that in group 2 (23.7 ± 11.8 vs. 39.2 ± 19.4 s, p < 0.0001) (Fig. 1B). The ΔTTI ((TTI in LSPV)-(TTI in LIPV)) was significantly greater in group 1 than that in group 2 (31.1 ± 31.4 vs. − 5.0 ± 25.9 s, p < 0.0001) (Fig. 1C). Even if the patients with persistent AF were excluded from the analysis, the ΔTTI was significantly greater in group 1 than that in group 2 (29.3 ± 28.1 vs. − 5.0 ± 26.7 s, p < 0.0001).
A comparison of the TTI values in the left PVs between group 1 and group 2 in 112 patients in whom TTI monitoring was capable for both the LSPV and the LIPV. A TTI at the LSPVs. B TTI at the LIPVs. C ΔTTI ((TTI in LSPVs) – (TTI in LIPVs)). LI(S)PV left inferior (superior) PV, PV pulmonary vein, TTI time-to-isolation
The ΔTTI value had a weak positive correlation with the total freeze dose of the LSPV (R = 0.3, p < 0.01) but not with the total freeze dose of the LIPV (p = 0.99). There was no significant difference in the total freeze dose of the LSPV (194 ± 61 vs. 192 ± 60 s, p = 0.81), total freeze dose of the LIPV (174 ± 47 vs. 166 ± 17 s, p = 0.27), total number of freezes for the LSPV (1.2 ± 0.6 vs. 1.1 ± 0.6, p = 0.60), and total number of freezes for the LIPV (1.2 ± 0.5 vs. 1.1 ± 0.3, p = 0.24) between group 1 and group 2.
3.3 Repeat procedures
During a median of 8.0 (4–12) months of follow-up, 10 (6.9%) patients (8 in group 1 and 2 in group 2, p = 0.72) had recurrent AF and underwent a second procedure at a median of 4.5 (1.7–11.2) months after the initial procedure. A total of 12 reconnected PVs (4 LSPVs, 2 LIPVs, 2 RSPVs, and 4 RIPVs) were identified in 8 patients, while no PVs reconnected in the remaining 2 patients (1 in each group). A reconnection was observed in the initially targeted vein in 5 patients (4 LSPVs in group 1 and 1 LIPV in group 2) and in the secondary targeted vein in 1 patient (1 LIPV in group 1).
4 Discussion
The present study demonstrated that the order of targeting the PVs highly influenced the TTI values of the left PVs owing to the presence of electrical connections between the left ipsilateral PVs in CB ablation. Although the TTI is one of the important parameters for deciding the optimal freeze dose, this should be taken into account in the CB ablation of the left PVs.
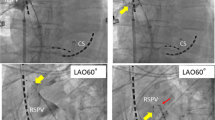
The presence of crossing myocardial strands on the epicardial and/or subendocardial aspects of the PV wall between adjacent PVs has been reported in histological studies,7 and the presence has been confirmed in electrophysiological studies. [8,9,10] The recognition is important during a PV ostial isolation using a CB because a CB-PVI is an ostial PVI when using a 28-mm CB. Actually, a previous study clarified that, even if the LSPV was not isolated by a single 180 s cryoapplication with a complete vein occlusion, approximately 40% of the LSPVs are isolated by a subsequent LIPV application. [11] The relatively thick myocardial tissue in the left ridge area and close proximity of the adjacent PVs explains the higher incidence of the crosstalk phenomenon in the left ipsilateral PVs. The present study results were in line with those study results. When the LSPV was initially targeted and followed by the LIPV, the TTI of the LSPV was relatively long and the TTI of the LIPV was short. On the contrary, when the LIPV was initially targeted and followed by the LSPV, the TTI of the LIPV was relatively long and the TTI of the LSPV was short. This could be well-explained by the presence of electrical connections between the ipsilateral left PVs (Fig. 2). The inter-PV connections could be eliminated by both LSPV and LIPV applications, and the disconnection is necessary for the electrical isolation of both the LSPV and the LIPV. We speculated that when the inter-PV connections were rich and the CB positions were ostial, the role of inter-PV connections was relatively more important. With CB ablation, the carina area, which included myocardial crossing fibers and thick myocardial sleeves, was ablated by both sequential LSPV and LIPV applications, which resulted in creating a robust lesion in this challenging area. This could explain the high PVI durability after the CB ablation rather than with the radiofrequency point-by-point ablation.
Illustration of the mechanisms. The green and blue circles indicate the PV musculature and CB contact area. The red lines indicate the inter-PV connections and thick myocardium in the ridge area. When the LSPV was initially targeted and followed by the LIPV, the TTI of the LSPV was relatively long, and the TTI of the LIPV was short (left panel). On the contrary, when the LIPV was initially targeted and followed by the LSPV, the TTI of the LIPV was relatively long, and the TTI of the LSPV was short (right panel). This was because the inter-PV connections and thick myocardium in the ridge area had already been ablated by the initial cryoapplication, and the contribution of this area to the LA-PV connections became relatively small during the second application. LI(S)PV left inferior (superior) PV, PV pulmonary vein, TTI time-to-isolation
The recognition of inter-PV connections is clinically important. Currently, the most important physiologic endpoint to predict a successful PVI appears to be the TTI as identified by the Achieve catheter, as this is the only true tissue physiology that can be monitored. Some prior studies proposed the TTI-guided dosing strategy, such as the TTI plus 120 s if the TTI was < 60 s.3,4 However, the data during the second procedure showed that the TTI plus 120 s (if the TTI was < 60 s) did not always predict a durable PVI in each individual PV. [6] The other study showed that the parameters predicting the PVI durability differed among the 4 PVs, and that the TTI was a strong predictor of the durability of the RSPV but was not the LSPV and LIPV.5 The relatively lower reliability of the TTI of left PVs than that for the right PVs could be reasonably explained by the presence of electrical connections between the ipsilateral left PVs. The present study together with the other previous studies showed that the optimal freeze dose of left PVs needs to be decided based on several clinical and procedural parameters, but not solely on the TTI.
4.1 Study limitations
This study was a single-center observational study. Therefore, there were differences in some patient characteristics between the 2 groups. Nevertheless, the study results were similar even if the persistent AF patients were excluded. The study population of group 2 was relatively small; nevertheless, the difference in the TTI value was significant. We did not change the order of targeting the PVs for the right ipsilateral PVs because a crosstalk phenomenon is less likely to occur compared to the left PVs, which has been shown in histological [7] and clinical studies. [11]
5 Conclusions
In CB ablation, the order of targeting the PVs highly influenced the TTI of the left PVs owing to the presence of electrical connections between the left ipsilateral PVs. Although the TTI is one of the important parameters for deciding the optimal freeze dose, this should be taken into account in the CB ablation of the left PVs.
References
Calkins H, Hindricks G, Cappato R, Kim YH, Saad EB, Aguinaga L, Akar JG, Badhwar V, Brugada J, Camm J, Chen PS, Chen SA, Chung MK, Nielsen JC, Curtis AB, Davies DW, Day JD, d’Avila A, de Groot NMSN, Di Biase L, Duytschaever M, Edgerton JR, Ellenbogen KA, Ellinor PT, Ernst S, Fenelon G, Gerstenfeld EP, Haines DE, Haissaguerre M, Helm RH, Hylek E, Jackman WM, Jalife J, Kalman JM, Kautzner J, Kottkamp H, Kuck KH, Kumagai K, Lee R, Lewalter T, Lindsay BD, Macle L, Mansour M, Marchlinski FE, Michaud GF, Nakagawa H, Natale A, Nattel S, Okumura K, Packer D, Pokushalov E, Reynolds MR, Sanders P, Scanavacca M, Schilling R, Tondo C, Tsao HM, Verma A, Wilber DJ, Yamane T. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Heart Rhythm. 2017;14:e275–444.
Kuck KH, Brugada J, Fürnkranz A, Metzner A, Ouyang F, Chun KR, Elvan A, Arentz T, Bestehorn K, Pocock SJ, Albenque JP, Tondo C, FIRE AND ICE Investigators. Cryoballoon or radiofrequency ablation for paroxysmal atrial fibrillation. N Engl J Med. 2016;374:2235–45.
Chun KR, Stich M, Fürnkranz A, Bordignon S, Perrotta L, Dugo D, Bologna F, Schmidt B. Individualized cryoballoon energy pulmonary vein isolation guided by real-time pulmonary vein recordings, the randomized ICE-T trial. Heart Rhythm. 2017;14:495–500.
Aryana A, Kenigsberg DN, Kowalski M, Koo CH, Lim HW, O’Neill PG, Bowers MR, Hokanson RB, Ellenbogen KA, Cryo-DOSING Investigators. Verification of a novel atrial fibrillation cryoablation dosing algorithm guided by time-to-pulmonary vein isolation: results from the Cryo-DOSING Study (Cryoballoon-ablation DOSING based on the assessment of time-to-effect and pulmonary vein isolation guidance). Heart Rhythm. 2017;14:1319–25.
Miyazaki S, Kajiyama T, Watanabe T, Nakamura H, Hachiya H, Tada H, Iesaka Y. Predictors of durable pulmonary vein isolation after second-generation cryoballoon ablation with a single short freeze strategy - different criteria for the best freeze of the 4 individual PVs. Int J Cardiol. 2020;301:96–102.
Miyazaki S, Kajiyama T, Watanabe T, Nakamura H, Hachiya H, Tada H, Iesaka Y. Can the durability of pulmonary vein isolation be predicted by the time-to-isolation in second-generation cryoballoon ablation?: Insight From the Results of Repeat Procedures. Circ Arrhythm Electrophysiol. 2020;13:e008076.
Cabrera JA, Ho SY, Climent V, Fuertes B, Murillo M, Sánchez-Quintana D. Morphological evidence of muscular connections between contiguous pulmonary venous orifices: relevance of the interpulmonary isthmus for catheter ablation in atrial fibrillation. Heart Rhythm. 2009;6:1192–8.
Tritto M, De Ponti R, Zardini M, Spadacini G, Oliveira M, Salerno-Uriarte JA. Electrical connection between pulmonary veins in humans. Evidence after radiofrequency ablation of the venoatrial junction. Circulation. 2001;104:e30–1.
Takahashi A, Iesaka Y, Takahashi Y, Takahashi R, Kobayashi K, Takagi K, Kuboyama O, Nishimori T, Takei H, Amemiya H, Fujiwara H, Hiraoka M. Electrical connections between pulmonary veins: implication for ostial ablation of pulmonary veins in patients with paroxysmal atrial fibrillation. Circulation. 2002;105:2998–3003.
Squara F, Liuba I, Chik W, Santangeli P, Maeda S, Zado ES, Callans D, Marchlinski FE. Electrical connection between ipsilateral pulmonary veins: prevalence and implications for ablation and adenosine testing. Heart Rhythm. 2015;12:275–82.
Miyazaki S, Kajiyama T, Watanabe T, Hada M, Nakamura H, Hachiya H, Tada H, Hirao K, Iesaka Y. Impact of electrical connections between ipsilateral pulmonary veins on the second-generation cryoballoon ablation procedure. J Cardiovasc Electrophysiol. 2019;30:27–31.
Acknowledgements
We thank Mr John Martin for his help in the preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The study protocol was approved by the hospital’s institutional review board. The study complied with the Declaration of Helsinki.
Informed consent
All patients gave their written informed consent.
Conflict of interest
Dr Miyazaki has received consulting fees and speaker honoraria from Medtronic and belongs to the endowed departments of Medtronic, Boston, Abbott, and Japan Lifeline. The other authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Miyazaki, S., Hasegawa, K., Nodera, M. et al. The impact of electrical connections between left ipsilateral pulmonary veins on the time-to-isolation values in cryoballoon ablation. J Interv Card Electrophysiol 64, 581–586 (2022). https://doi.org/10.1007/s10840-021-01034-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-021-01034-7