Abstract
Background
Venous thromboembolism (VTE), including deep venous thrombosis (DVT) and pulmonary embolism (PE), represents a common cause of morbidity and mortality following complex gastrointestinal surgery. Whether perioperative VTE also exposes patients to a higher long-term risk of VTE events remains poorly defined.
Methods
The Medicare 100% Standard Analytic Files were used to identify patients undergoing esophageal, hepatic, pancreatic, and colorectal resection between 2013 and 2017. The impact of perioperative VTE, defined as a VTE episode occurring during the index hospitalization or within 30 days of discharge, on the risk of developing subsequent long-term VTE episodes (i.e., more than 30 days following discharge) was examined.
Results
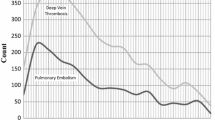
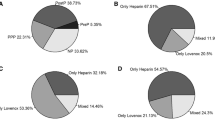
Among 253,212 patients who underwent complex gastrointestinal surgery, 1.9% (n=4763) developed a VTE episode perioperatively. With a median follow-up period of 553 days (IQR 194–1052), a total of 11,052 patients (4.4%) developed a long-term VTE episode. Of note, patients who developed a DVT perioperatively had a higher risk of experiencing a long-term VTE episode than patients who had no perioperative thromboembolic complications (HR 6.50, 95%CI 6.04–6.98). The increase in risk was more pronounced among patients who had a PE (HR 27.97, 95%CI 25.39–30.80) at the time of surgery. Risk factors for long-term thromboembolic events following complex GI surgery included Black patients (HR 1.20, 95%CI 1.11–1.30), receipt of surgery at a teaching hospital (HR 1.09, 95%CI 1.04–1.13), nonelective surgery (HR 1.19, 95%CI 1.14–1.24), as well as a diagnosis of cancer (HR 1.10, 95%CI 1.05–1.16). The development of a perioperative DVT was associated with an increased long-term risk of VTE in both cancer (HR 5.59, 95%CI 5.29–6.61) and non-cancer patients (HR 6.98, 95%CI 6.37–7.64). Similarly, experiencing a PE at the time of surgery led to a higher long-term risk of VTE in cancer (HR 24.30, 95%CI 21.08–28.02), as well as non-cancer (HR 30.81, 95%CI 27.01–35.15) patients.
Conclusions
Patients with a history of perioperative VTE had a higher risk of developing subsequent VTE events within 1–2 years following complex GI surgery. The risk was more pronounced among patients who had perioperative PE rather than DVT. These findings were consistent among both cancer and non-cancer patients.

Similar content being viewed by others
References
Beckman MG, Hooper WC, Critchley SE, et al. Venous thromboembolism: a public health concern. Am J Prev Med 2010; 38(4 Suppl):S495-501.
Kim NH, Delcroix M, Jenkins DP, et al. Chronic thromboembolic pulmonary hypertension. J Am Coll Cardiol 2013; 62(25 Suppl):D92-9.
Makedonov I, Kahn SR, Galanaud JP. Prevention and Management of the Post-Thrombotic Syndrome. J Clin Med 2020; 9(4).
Kearon C, Akl EA, Ornelas J, et al. Antithrombotic Therapy for VTE Disease: CHEST Guideline and Expert Panel Report. Chest 2016; 149(2):315-352.
Kahn SR, Lim W, Dunn AS, et al. Prevention of VTE in nonsurgical patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012; 141(2 Suppl):e195S-e226S.
Grosse SD, Nelson RE, Nyarko KA, et al. The economic burden of incident venous thromboembolism in the United States: A review of estimated attributable healthcare costs. Thromb Res 2016; 137:3-10.
Heit JA, O'Fallon WM, Petterson TM, et al. Relative impact of risk factors for deep vein thrombosis and pulmonary embolism: a population-based study. Arch Intern Med 2002; 162(11):1245-8.
Iorio A, Kearon C, Filippucci E, et al. Risk of recurrence after a first episode of symptomatic venous thromboembolism provoked by a transient risk factor: a systematic review. Arch Intern Med 2010; 170(19):1710-6.
Kearon C, Ageno W, Cannegieter SC, et al. Categorization of patients as having provoked or unprovoked venous thromboembolism: guidance from the SSC of ISTH. J Thromb Haemost 2016; 14(7):1480-3.
Braekkan SK, Hansen JB. Substantial recurrence risk after venous thromboembolism provoked by minor risk factors. J Thromb Haemost 2018; 16(9):1671-1673.
Sweetland S, Green J, Liu B, et al. Duration and magnitude of the postoperative risk of venous thromboembolism in middle aged women: prospective cohort study. BMJ 2009; 339:b4583.
Anderson DR, Morgano GP, Bennett C, et al. American Society of Hematology 2019 guidelines for management of venous thromboembolism: prevention of venous thromboembolism in surgical hospitalized patients. Blood Adv 2019; 3(23):3898-3944.
Baglin T, Luddington R, Brown K, et al. Incidence of recurrent venous thromboembolism in relation to clinical and thrombophilic risk factors: prospective cohort study. Lancet 2003; 362(9383):523-6.
Hansson PO, Sorbo J, Eriksson H. Recurrent venous thromboembolism after deep vein thrombosis: incidence and risk factors. Arch Intern Med 2000; 160(6):769-74.
Prins MH, Lensing AWA, Prandoni P, et al. Risk of recurrent venous thromboembolism according to baseline risk factor profiles. Blood Adv 2018; 2(7):788-796.
Blom JW, Doggen CJ, Osanto S, et al. Malignancies, prothrombotic mutations, and the risk of venous thrombosis. JAMA 2005; 293(6):715-22.
Centers for Medicare and Medicaid services Limited Data Set (LDS) Files 06/30/2020 11:06 AM. Available at: https://www.cms.gov/Research-Statistics-Data-and-Systems/Files-for-Order/Data-Disclosures-Data-Agreements/DUA_-_NewLDS. Accessed February 23rd, 2021.
Spyropoulos AC, Ashton V, Chen YW, et al. Rivaroxaban versus warfarin treatment among morbidly obese patients with venous thromboembolism: Comparative effectiveness, safety, and costs. Thromb Res 2019; 182:159-166.
White RH, Garcia M, Sadeghi B, et al. Evaluation of the predictive value of ICD-9-CM coded administrative data for venous thromboembolism in the United States. Thromb Res 2010; 126(1):61-7.
Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40(5):373-83.
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005; 43(11):1130-9.
Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 2011; 173(6):676-82.
Abbas A, Madison Hyer J, Pawlik TM. Race/Ethnicity and County-Level Social Vulnerability Impact Hospice Utilization Among Patients Undergoing Cancer Surgery. Ann Surg Oncol 2021; 28(4):1918-1926.
Merath K, Chen Q, Bagante F, et al. Textbook Outcomes Among Medicare Patients Undergoing Hepatopancreatic Surgery. Ann Surg 2020; 271(6):1116-1123.
Fine JG, RJ. A Proportional Hazards Model for the Subdistribution of a Competing Risk. Journal of the American Statistical Association 1999; 94(446):496-509.
Nelson RE, Grosse SD, Waitzman NJ, et al. Using multiple sources of data for surveillance of postoperative venous thromboembolism among surgical patients treated in Department of Veterans Affairs hospitals, 2005-2010. Thromb Res 2015; 135(4):636-42.
Hachey KJ, Sterbling H, Choi DS, et al. Prevention of Postoperative Venous Thromboembolism in Thoracic Surgical Patients: Implementation and Evaluation of a Caprini Risk Assessment Protocol. J Am Coll Surg 2016; 222(6):1019-27.
Ortel TL, Neumann I, Ageno W, et al. American Society of Hematology 2020 guidelines for management of venous thromboembolism: treatment of deep vein thrombosis and pulmonary embolism. Blood Adv 2020; 4(19):4693-4738.
Galster H, Kolb G, Kohsytorz A, et al. The pre-, peri-, and postsurgical activation of coagulation and the thromboembolic risk for different risk groups. Thromb Res 2000; 100(5):381-8.
Gangireddy C, Rectenwald JR, Upchurch GR, et al. Risk factors and clinical impact of postoperative symptomatic venous thromboembolism. J Vasc Surg 2007; 45(2):335-341; discussion 341-2.
Trinh VQ, Karakiewicz PI, Sammon J, et al. Venous thromboembolism after major cancer surgery: temporal trends and patterns of care. JAMA Surg 2014; 149(1):43-9.
Davenport DL, Vargas HD, Kasten MW, et al. Timing and perioperative risk factors for in-hospital and post-discharge venous thromboembolism after colorectal cancer resection. Clin Appl Thromb Hemost 2012; 18(6):569-75.
Hanna-Sawires RG, Groen JV, Klok FA, et al. Outcomes following pancreatic surgery using three different thromboprophylaxis regimens. Br J Surg 2019; 106(6):765-773.
Mantziari S, Gronnier C, Pasquer A, et al. Incidence and Risk Factors Related to Symptomatic Venous Thromboembolic Events After Esophagectomy for Cancer. Ann Thorac Surg 2016; 102(3):979-984.
Sahara K, Paredes AZ, Merath K, et al. Evaluation of the ACS NSQIP Surgical Risk Calculator in Elderly Patients Undergoing Hepatectomy for Hepatocellular Carcinoma. J Gastrointest Surg 2020; 24(3):551-559.
Colorectal Writing Group for Surgical C, Outcomes Assessment Program-Comparative Effectiveness Research Translation Network C, Nelson DW, et al. Thromboembolic Complications and Prophylaxis Patterns in Colorectal Surgery. JAMA Surg 2015; 150(8):712-20.
Beal EW, Tumin D, Chakedis J, et al. Which Patients Require Extended Thromboprophylaxis After Colectomy? Modeling Risk and Assessing Indications for Post-discharge Pharmacoprophylaxis. World J Surg 2018; 42(7):2242-2251.
Austin H, De Staercke C, Lally C, et al. New gene variants associated with venous thrombosis: a replication study in White and Black Americans. J Thromb Haemost 2011; 9(3):489-95.
Ross SW, Kuhlenschmidt KM, Kubasiak JC, et al. Association of the Risk of a Venous Thromboembolic Event in Emergency vs Elective General Surgery. JAMA Surg 2020; 155(6):503-511.
Symer MM, Abelson JS, Yeo HL. Barriers to Regionalized Surgical Care: Public Perspective Survey and Geospatial Analysis. Ann Surg 2019; 269(1):73-78.
Hull RD, Schellong SM, Tapson VF, et al. Extended-duration venous thromboembolism prophylaxis in acutely ill medical patients with recently reduced mobility: a randomized trial. Ann Intern Med 2010; 153(1):8-18.
Prandoni P, Lensing AW, Prins MH, et al. Residual venous thrombosis as a predictive factor of recurrent venous thromboembolism. Ann Intern Med 2002; 137(12):955-60.
Tan M, Mos IC, Klok FA, et al. Residual venous thrombosis as predictive factor for recurrent venous thromboembolism in patients with proximal deep vein thrombosis: a systematic review. Br J Haematol 2011; 153(2):168-78.
Ye F, Stalvey C, Khuddus MA, et al. A systematic review of mobility/immobility in thromboembolism risk assessment models for hospitalized patients. J Thromb Thrombolysis 2017; 44(1):94-103.
Toledano TH, Kondal D, Kahn SR, et al. The occurrence of venous thromboembolism in cancer patients following major surgery. Thromb Res 2013; 131(1):e1-5.
Prandoni P, Falanga A, Piccioli A. Cancer and venous thromboembolism. Lancet Oncol 2005; 6(6):401-10.
Abdol Razak NB, Jones G, Bhandari M, et al. Cancer-Associated Thrombosis: An Overview of Mechanisms, Risk Factors, and Treatment. Cancers (Basel) 2018; 10(10).
Heit JA. Epidemiology of venous thromboembolism. Nat Rev Cardiol 2015; 12(8):464-74.
Sud R, Khorana AA. Cancer-associated thrombosis: risk factors, candidate biomarkers and a risk model. Thromb Res 2009; 123 Suppl 4:S18-21.
Mahajan A, Brunson A, White R, et al. The Epidemiology of Cancer-Associated Venous Thromboembolism: An Update. Semin Thromb Hemost 2019; 45(4):321-325.
Hutten BA, Prins MH, Gent M, et al. Incidence of recurrent thromboembolic and bleeding complications among patients with venous thromboembolism in relation to both malignancy and achieved international normalized ratio: a retrospective analysis. J Clin Oncol 2000; 18(17):3078-83.
Prandoni P, Lensing AW, Piccioli A, et al. Recurrent venous thromboembolism and bleeding complications during anticoagulant treatment in patients with cancer and venous thrombosis. Blood 2002; 100(10):3484-8.
Key NS, Khorana AA, Kuderer NM, et al. Venous Thromboembolism Prophylaxis and Treatment in Patients With Cancer: ASCO Clinical Practice Guideline Update. J Clin Oncol 2020; 38(5):496-520.
Nathan H, Pawlik TM. Limitations of claims and registry data in surgical oncology research. Ann Surg Oncol 2008; 15(2):415-23.
Ay C, Pabinger I, Cohen AT. Cancer-associated venous thromboembolism: Burden, mechanisms, and management. Thromb Haemost 2017; 117(2):219-230.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
The study was approved by the Institutional Review Board at the Ohio State University Wexner Medical Center.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Paro, A., Dalmacy, D., Hyer, J.M. et al. Impact of Perioperative Thromboembolic Complications on Future Long-term Risk of Venous Thromboembolism among Medicare Beneficiaries Undergoing Complex Gastrointestinal Surgery. J Gastrointest Surg 25, 3064–3073 (2021). https://doi.org/10.1007/s11605-021-05080-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-021-05080-4