ABSTRACT
Purpose
Efforts have been made to standardize laboratory variant interpretation, but clinicians are ultimately tasked with clinical correlation and application of genetic test results in patient care. This study aimed to explore processes clinicians utilize when reviewing and returning genetic test results, and how they impact patient care.
Methods
Medical geneticists, genetic counselors, and nongenetics clinicians from two Midwestern states completed surveys (n = 98) and in-depth interviews (n = 29) on practices of reviewing and returning genetic test results. Retrospective chart review (n = 130) examined discordant interpretations and the impact on care.
Results
Participants reported variable behaviors in both reviewing and returning results based on factors such as confidence, view of role, practice setting, and relationship with the lab. Providers did not report requesting changes to variant classifications from laboratories, but indicated relaying conflicting classifications to patients in some cases. Chart reviews revealed medically impactful differences in interpretation between laboratories and clinicians in 18 (13.8%) records.
Conclusion
Clinician practices for reviewing and integrating genetic test results into patient care vary within and between specialties and impact patient care. Strategies to better incorporate both laboratory and clinician expertise into interpretation of genetic results could result in improved care across providers and settings.
Similar content being viewed by others
INTRODUCTION
The successful implementation of genomic guided precision medicine relies on accurate and consistent variant interpretation, which remains challenging. Significant efforts are being made to standardize the interpretation of genetic variants between clinical laboratories [1,2,3,4]. Beyond the laboratory, clinicians are tasked with clinical correlation and application of genetic test results in patient care, which may include review of variant classifications. Cardiology centers have reported the rate of laboratory–clinic discrepancies in variant classification as 10–18%, with the majority impacting clinical care [5, 6]. Similarly, variant classification discrepancies have been reported in oncology [7]. Incorrect variant classification can harm patients and families. For example, incorrect classification of a KCNQ1 variant for long QT syndrome resulted in unnecessary defibrillator implantation in family members and missed preventive efforts in others [8].
Previous studies examining the impact of clinician variant interpretation on diagnostics are limited, but suggest further integration of phenotypic and molecular data by the medical geneticist, along with additional laboratory testing, led to an increase in the diagnostic rate by 7% [9]. Studies also show genetic counselors taking a role in variant interpretation, and sometimes disagreeing with laboratory classifications, prompting discussions with the laboratory and medical team [10, 11]. Yet little is known about what occurs after these discussions and how this impacts patient care. Furthermore, there is a paucity of information on the processes and behaviors nongenetics clinicians use to review laboratory reports, despite their increasing use of genetic testing and concerns about their genetics knowledge and interpretation of results [12, 13]. Our objective was to better understand the processes genetics and nongenetics clinicians utilize when receiving and returning genetic testing results to patients, the frequency and outcome of clinician disagreements with a laboratory classification, and how this impacts clinical care.
MATERIALS AND METHODS
Study design
We conducted (1) a survey with clinicians exploring practices and resources used when interpreting genetic test results, (2) in-depth interviews with a subset of survey respondents about practices for interpreting and communicating results, and (3) a retrospective chart review assessing the presence and reasons for discordant laboratory to clinician interpretations and their impact on clinical care.
Recruitment
In spring/summer of 2017, survey participants were recruited from clinicians of all specialties at Children’s Mercy Kansas City (CMKC) who had ordered a genetic test in the past year. Genetics specialists (genetic counselors and medical geneticists) throughout Missouri and Kansas, identified by searching public National Society of Genetic Counselors (NSGC) and American College of Medical Genetics and Genomics (ACMG) databases and hospital websites, were also recruited. Survey eligibility was assessed by one question on whether the individual had returned genetic test results to a patient or family in the past year. Participants were invited to indicate interest in a follow-up in-depth interview. Interview participants were compensated $50.
Data collection
The survey and semistructured interview guide are provided as Supplementary material. The REDCap [14, 15] survey assessed how often participants return genetic test results and how often they seek assistance or conduct additional research when results include laboratory variant classifications of pathogenic, likely pathogenic, or a variant of uncertain significance (VUS) on a 5-point Likert-type scale. Finally, participants were asked to identify variant interpretation resources they use from a list. Demographics and specialty information were not collected to protect anonymity.
In-depth interviews were conducted in person or by phone by trained qualitative interviewers. After collecting experience and specialty, participants were given an example laboratory report (Supplementary material) and asked to walk through the thought and decision-making process they would take from the time they received the report to the time they were ready to discuss it with a patient or family. This was followed by questions about communications with laboratories or genetic specialists, use of resources, experiences with variant reclassification, communicating results to families, and training in interpreting genetic test results.
Analysis
Surveys were exported and analyzed using SPSS [16]. Descriptive statistics were calculated. Frequencies of behaviors in seeking assistance from medical genetics or laboratory personnel or conducting additional research were collapsed to never/rarely, sometimes, and frequently/always, and Chi-squared analyses were used to assess for differences by groups of frequency returning results. Interviews were audiorecorded, transcribed, and coded in Atlas.ti. Interview participants were grouped as genetic counselors (GCs), medical geneticists (MGs), and nongeneticist physicians and nurse practitioners (other providers, OPs). Three study team members (C.B., E.A.H., E.F.) conducted a content analysis beginning with a review of interview summaries and initial inductive coding of 17 transcripts by a minimum of two independent coders. Throughout the process, the coding team met to compare coding and reach consensus on a codebook (Supplementary material) and its application in an iterative process [17]. After refinement of the codebook and agreement on code definitions was ensured, the final 12 interviews were coded by one analyst each with continued discussion to resolve coding questions or discrepancies. In the final stage, C.B., E.A.H., and E.F. reviewed all coded excerpts to synthesize results into themes.
Retrospective chart review
All germline sequencing tests ordered for diagnostic purposes between April 2016 and March 2017 were pulled from one pediatric institution’s molecular genetics laboratory database, including in-house and send-out testing. Separate lists were compiled for those ordered by MGs and OPs. Each list was randomized, and tests were sequentially pulled from the randomized lists for chart review. Those with zero variants reported (n = 73, 25 ordered by MGs, 48 by OPs) or no documentation found of clinician interpretation (n = 10, all ordered by OPs) were removed and replaced with the next sequential test until the sample size was reached to give a > 90% confidence level of detecting a 10% rate of discordance. All electronic medical record (EMR) documentation by the ordering provider and clinic staff from the test order date to the review date was reviewed to identify any reference to the result. Interpretation of the original report, before any follow-up testing, was collected. Data collected included laboratory and clinician overall interpretation of the result, laboratory variant classification, and medical decisions based on the result. Each record was reviewed by two reviewers, and all records were reconciled to agreement by both reviewers.
RESULTS
Survey results
Survey invitations were emailed to 483 CMKC clinicians who had ordered a genetic test over the past year and to 43 genetic counselors and 10 medical geneticists practicing in Missouri and Kansas. A total of 130 survey responses were received; 18 were ineligible because they responded “no” to returning a genetic result in past year, 5 were removed for no response about frequency of returning results, and 9 were removed for no response to all remaining questions. The remaining 98 surveys were used in the analysis (response rate 18.3%). Of respondents, 36% returned genetic results ≥3×/month and 43% <1×/month (Fig. 1a).
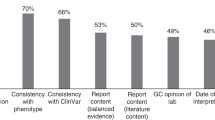
(a) A total of 98 clinicians answered the REDCap survey. When asked how often they return genetic testing results, 36% returned genetic test results ≥3× per month and 43% did so <1× per month. (b) The number of participants who reported using each listed resource and Chi-squared analysis for each assessing for differences in use between groups with differing frequency of returning results.
Even within groups based on frequency of returning results, participants reported variable behaviors of seeking assistance from laboratory or genetic specialists and conducting additional research (Table 1). Clinicians who less frequently returned genetic results were more likely to seek assistance (χ2(2)=19.08, p = 0.001) or conduct additional research (χ2(2)=17.00, p = 0.002) for a pathogenic variant, but no other variability was significantly associated with frequency of returning results. When conducting additional research, those who more frequently returned results used genetics specific resources more often (HGMD, ClinVar, population databases, and UCSC Genome Browser), while use of PubMed and OMIM did not differ by frequency of returning results (Fig. 1b). While we did not collect specialty in the survey, based on the demographics of interview participants (Table 2), we expect all GCs and MGs are included in those returning genetic results ≥3×/month.
Interview results
Thirty-three survey respondents shared their information to be contacted for an interview and 29 (29.6%) completed an interview. Participants included 16 GCs, 2 MGs, and 11 OPs. Demographics are in Table 2.
Processes for reviewing results
Participants discussed two reasons for conducting additional research: to educate themselves about the result and to investigate variant classification. All participants discussed educating themselves before discussing results with a family in order to integrate results with the patient’s phenotype and reason for testing. GCs and MGs reported investigating variant classification more often than OPs.
All participants discussed contacting the laboratory to aid in understanding of results or ask about utility of follow-up steps, such as familial testing. This was more frequent when the laboratory was internal and/or the participant had a relationship with laboratory representatives. Participants reported generally not asking labs to reclassify variants. Several OPs expressed that they would never consider asking a lab to reclassify as that was not their area of expertise. Some GCs felt that asking a lab to reclassify was not worth their time because laboratories were unlikely to reclassify variants.
Some GCs described offering laboratories additional clinical information or literature to confirm the laboratory had considered all the information or ask if new information might change the classification. Some GCs also discussed the standardized criteria used by the laboratory and felt reclassification should not happen unless it met those criteria.
“So then I was able to take that information back to the lab and say, ‘Hey, you know, we’re concerned because of the history. We’re concerned because we found this variant of unknown significance, now we have additional clinical findings that are confirmatory. You know, can we change the variant classification?’” –Cardiology GC
When interpretations differ
GCs and MGs, and rarely OPs, discussed sometimes thinking a variant’s classification may differ from that in the laboratory report. In these cases, participants reported sticking with the laboratory classification, discussing the contradictions between the laboratory and their assessment with patients, or in some cases, overriding the laboratory’s classification. Often the distinction between these in practice was subtle and interviews suggested several themes impacting how this is handled. Each theme is reported below, and illustrative quotes are given in Table 3.
Trust in a laboratory influenced a clinician’s likelihood of accepting (or not fully rejecting) a laboratory classification that they questioned. Many were from institutions with internal laboratories where they knew the analysts and trusted their processes. Others discussed developing trust in a handful of laboratories and using those labs whenever possible.
Participants’ views of their role also impacted action on a classification they question. Some GCs and MGs spoke of themselves as a unique part of the health-care team that brought the clinical view and direct knowledge of the patient to variant classification. Some GCs spoke of the limitations of their expertise, but of working with MGs who may reclassify variants. Both GCs and MGs discussed the “linking of genotype and phenotype” as an important role of MGs.
Along with most OPs, no GCs practicing in a setting without direct involvement of MGs stated a willingness to change clinical care based on their personal assessment of a variant. Some specifically spoke of perceived limitations in their expertise or that a change in care based on a revised variant classification would only occur when working with a MG. Further, GCs who worked in cardiology and cancer also spoke of returning to the family history to make recommendations, while those in pediatrics relayed more of a focus on finding a causative variant that could guide clinical care.
Use of heuristics and phenotype
The interviews suggested heuristics at work in some instances. Cancer GCs (but not those in other subspecialties) discussed seeing so many VUS reclassified to benign over time that they consider a VUS “benign until proven otherwise." Anchoring also played a role as participants stated that when they had a condition or gene in mind, it may be particularly hard to consider a reported variant in that gene or pathway to be potentially benign.
“If they see a kid and they’re clinically suspicious about something super rare and we get a variant in the gene that causes that super rare something they clinically were suspicious of, it’s hard for us to write that variant off.” –Pediatric + Prenatal GC
Participants across specialties most often referenced assessing the fit of the variant to the patient’s phenotype as a primary action in reviewing variants.
“I’m definitely trying to put together, does the kid actually resemble what we typically think of with this condition? Which is hard because we’re learning how variable things are.” –Pediatric + Cardiology GC
Impact on patient communication and care
When participants questioned variant classification, either they were highly suspicious that a reported VUS was pathogenic or that a reported pathogenic variant was not diagnostic for the patient, most indicated they would transparently discuss this with the patient or family. Many discussed “hedging” on their interpretation, telling patients that their clinical suspicion may or may not be correct and that new information would come with time. Participants also discussed being clear about the fluid nature of variant interpretation, to prepare patients that a classification may change. This was seen as particularly important for patients managed by multiple specialists who may offer differing interpretations.
“I’ll say to parents that we can’t say for certain, but it’s likely connected to our issues. There is a difference between the formal making a call about something and the application in the clinic.” –Pediatric Neurologist
Participants rarely reported overtly stating that they felt the laboratory’s classification was incorrect. Those who did felt that patients and families could understand this distinction, while those who did not were worried about the impact on families.
“We would just present it to the patient as, ‘We trust that this is the cause of this condition in your family. We know it’s a VUS but we’re telling you it’s likely pathogenic.’ You know, and I don’t really feel that patients have trouble understanding that or anything.” –Pediatric + Cancer GC
“I do fear the next 5 years, 10 years is going to be a lot of take backs…I worry what we don’t think about enough is the family perception of what we’re telling them, and who’s telling them.” –Medical Geneticist
Participants sometimes discussed making medical recommendations based on a classification of a variant that differed from the laboratory report, most often in recommending screening tests for other manifestations of a syndrome associated with a gene in which the patient had a variant classified as having uncertain significance, but which they were suspicious of being pathogenic. However, participants clearly discussed being conservative in these recommendations; that while they would feel comfortable recommending screening tests, they would stop short of invasive procedures. Conversely, if the lab called a variant pathogenic and the clinical team disagreed, they felt they still needed to complete any recommended tests to ensure they had not missed a manifestation of the disease that required treatment or that could further support variant pathogenicity.
Participants reported documenting their interpretation of the genetic variant and its use in clinical care with the same transparency in which they explained it to patients. Participants noted that because the laboratory report would not be amended, other providers may see the report without the clinician’s interpretation. A small number also noted that this does not pass along clinician interpretation of the variant to be accessible to other labs and providers when the variant is identified in future patients.
“It would be documented in the clinic notes where we saw the patient. The clinical interpretation of the variant would be documented and that’s where it would say, ‘You know, although this is the lab classification of VUS, we feel, you know, XYZ,’ and it wouldn’t be amended to the actual lab report per se or attached to the actual lab report in any straightforward way.” –Pediatric GC
Chart review results
Our retrospective chart review included 130 sequencing tests (n = 65 ordered by MGs and n = 65 ordered by OPs). Eighteen records (13.8%) had discordant interpretation between the laboratory and clinical team (Table 4). Of the 18, 4 were a change in interpretation in tests ordered by MGs and 14 by OPs. Of the discordant interpretations, 15 (11.5% of reviewed records, 83.3% of discordant) represented a change in interpretation from nondiagnostic or indeterminate to likely diagnostic/diagnostic and 3 (2.3% of reviewed records, 16.7% of discordant) were reported by the laboratory as diagnostic and conveyed as uncertain to the patient (Table 4).
All discordant interpretations impacted recurrence risks and 13 (72.2%) impacted patient care through surveillance, additional testing, or referrals to specialists (Table 4). In the 18 cases where discordant interpretation was documented, 2 (11.1%) were due to a clinical diagnosis of the condition suggested in an indeterminate report and 15 (83.3%) were based on an apparent discordant variant classification from laboratory to clinician, though it is not always clear if this is based on clinician reassessment of the classification or a misunderstanding of the classification. When an explanation was given, phenotypic correlation at the gene level was the most common explanation. References to correlation with a specific variant’s attributes and primary literature were made less frequently.
DISCUSSION
Our study indicates wide variability in the practices of clinicians interpreting and returning genetic test results, ultimately impacting diagnoses and medical care. In particular, our survey data reveal that a majority of clinicians, across specialties, perform additional research before returning genetic testing results. This corroborates previous findings of GCs and MGs actively researching variants and the perceived value of the genetic specialist’s role in variant interpretation and correlation of results with the patient phenotype [8,9,10,11, 18]. However, our study extends this activity to OPs, and reveals a qualitative distinction in researching a result to educate oneself and to investigate a variant’s classification; the latter ascribed to by MGs, only some GCs, and a small subset of OPs. The interview finding that OPs more commonly discussed researching a result to educate oneself before communicating the result may also explain why those in the survey who less frequently return results report conducting research on pathogenic variants more often.
Our interview data also help to explain the variability in behaviors for investigating variants seen in the survey, even among clinicians with similar frequencies of returning results, by revealing that clinician behaviors around variant interpretation vary by individual factors such as view of role, confidence in skills, use of heuristics, relationship with the laboratory, and practice setting (i.e., working with a MG). Wain et al. [11] also identified lack of knowledge as a barrier to performing variant interpretation and found differences by genetic counselor specialty, but did not relate these differences back to working with a MG. Furthermore, our interviews indicate these factors also impact OPs’ behaviors and extend their impact beyond variant investigation activities to the actions taken when a clinician disagrees with a laboratory classification. This novel finding highlights that when a laboratory–clinician discrepancy exists in variant classification, whether that is communicated to the family and its impact on patient care may differ based on individual clinician factors.
Our interviews also demonstrate that clinicians frequently discussed a focus on the fit of a variant to the patient’s phenotype. This was also the most frequent reference for change in variant classification in the chart review. Indeed, clinicians are tasked with correlating genetic test results with patient phenotype. However, when phenotype is considered both in laboratory criteria and as a focus of clinician variant interpretation there is a risk of overemphasizing phenotype within the scope of other interpretation criteria. While the use of phenotype to support variant claims is included in laboratory variant classifications (ACMG/AMP criteria PP4) [1], PP4 has been shown to be the most inconsistently applied criterion across laboratories [2]. Phenotypic correlation is further complicated in rare disease where the phenotypic spectrum of disease is unknown. This may create a tension between variant classification and clinical correlation, and additional studies reviewing how phenotype is being applied by clinicians may be useful in addressing the integration of phenotype in interpretation.
Another novel and important finding is that most OPs interviewed indicated that they did not investigate a variant’s classification and would never alter a laboratory’s classification of a variant. Yet, our case review revealed that apparent variant classification discrepancies occurred three times more frequently with OPs than with MGs. This increased frequency of reclassifications and some possible misinterpretations in our chart review, accompanied by previous data suggesting misinterpretation of genetic data by nongeneticists [19,20,21], is concerning. While this may be addressed through continuing education, Donohue et al. [21] identified complex reasons for misinterpretation of results by nongenetics, including unclear laboratory reports or poor communication between laboratories and clinicians. This suggests more frequent and open discussions between clinicians and laboratory personnel or institutional teams available to consult on both the phenotypic and genotypic data in a patient may be helpful. Ways to address this finding are particularly important given the paucity of genetics providers and continued increases in ordering of genetic tests by nongenetic providers. It is also worth noting the potential legal ramifications of variant reclassification and return of results, as legal liability in genomic testing has not been well established [22].
Ultimately, this study identified several factors that introduce variability into the process of clinician variant interpretation, while laboratory variant interpretation guidelines have sought to limit variability [1]. It also demonstrates the ramifications of laboratory–clinician discrepant variant classifications. GCs and MGs report making conservative recommendations for screening based on reclassifications, but our chart review reveals additional impacts from recurrence risks to additional testing. Still, evidence suggests that multidisciplinary specialty centers may obtain lower rates of disagreement about variant interpretation among themselves than found among laboratories for the same variants, supporting the value of clinician input [6]. This begs the question of how laboratory and clinician expertise can be best combined to optimize variant interpretation in the diverse settings in which genetic tests are ordered and reported. Our data reveal a frequent lack of direct communication between clinicians and labs when a clinician disagrees with a variant’s classification, which can impact both that patient’s care and evaluation of that variant in future patients. The submission of variant classifications by clinicians into ClinVar [23] offers one way to make clinician interpretations available as data. However, there may also be an opportunity for laboratories’ CLIA-required clinical consultants to facilitate discussions between labs and their clients and to document clinician classifications and their evidence to have available for future variant classifications. For institutions with clinical laboratories, consultation with transdisciplinary teams for variant review when questions arise may facilitate ideal incorporation of both the clinical and molecular team’s expertise [24]. While the roles of the laboratory and clinician are distinct, these steps could limit discrepant variant classifications by better incorporating the knowledge base of both the clinician and laboratory up front and ensuring the knowledge and perceptions of each are shared with the other.
This study is limited in that it was conducted in a single geographic region, with all OP interviews and the chart review conducted at one pediatric institution and GC and MG interviews conducted with clinicians practicing within two states. Therefore, participants may not represent practices at other institutions or geographical areas, though some data corroborate findings from studies with wider geographic distributions. Data were also collected in 2016 and 2017 and practices may have changed since that time. Additionally, our interview data where most OPs said they would not alter a variant classification contradict the findings of our chart review, suggesting possible bias in the sample or responses of OPs interviewed. Given the response rate of 18.3% for our survey, there may also be unknown biases in those who responded. Since demographics and specialty information were not collected, these cannot be used to assess survey respondent characteristics. Finally, chart review cannot account for information that may have been communicated about a result that was not documented in the EMR and reviewer perceptions of clinician interpretations in the chart review were not validated.
In summary, our study of the practices of clinician interpretation and return of genetic test results indicates wide variability, ultimately impacting overall diagnostic rates and medical care. While additional studies are needed to fully elucidate practice differences between clinical role and subspecialties, this study provides important information about sources of variability in the interpretation and use of genetic testing information. We suggest increased and documented communication between clinicians returning test results and the laboratories issuing the reports to facilitate appropriate use of each group’s expertise and transparent discussions about differences in variant interpretation.
Data availability
De-identified data are available by individual request.
References
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405–24.
Amendola LM, Jarvik GP, Leo MC, McLaughlin HM, Akkari Y, Amaral MD, et al. Performance of ACMG-AMP variant-interpretation guidelines among nine laboratories in the Clinical Sequencing Exploratory Research Consortium. Am J Hum Genet. 2016;99:247.
Abou Tayoun AN, Pesaran T, DiStefano MT, Oza A, Rehm HL, Biesecker LG, et al. Recommendations for interpreting the loss of function PVS1 ACMG/AMP variant criterion. Hum Mutat. 2018;39:1517–24.
ClinGen. Variant pathogenicity curation documents. https://clinicalgenome.org/curation-activities/variant-pathogenicity/documents. Accessed 1 February 2021.
Bland A, Harrington EA, Dunn K, Pariani M, Platt J, Grove ME, et al. Clinically impactful differences in variant interpretation between clinicians and testing laboratories: a single-center experience. Genet Med. 2018;20:369–73.
Furqan A, Arscott P, Girolami F, Cirino AL, Michels M, Day SM, et al. Care in specialized centers and data sharing increase agreement in hypertrophic cardiomyopathy genetic test interpretation. Circ Cardiovasc Genet. 2017;10:e001700.
Zirkelbach E, Hashmi S, Ramdaney A, Dunnington L, Ashfaq M, Nugent EK, et al. Managing variant interpretation discrepancies in hereditary cancer: clinical practice, concerns, and desired resources. J Genet Couns. 2018;27:761–9.
Ackerman JP, Bartos DC, Kapplinger JD, Tester DJ, Delisle BP, Ackerman MJ. The promise and peril of precision medicine: phenotyping still matters most. Mayo Clin Proc. 2016;S0025-6196:30463.
Baldridge D, Heeley J, Vineyard M, Manwaring L, Toler TL, Fassi E, et al. The Exome Clinic and the role of medical genetics expertise in the interpretation of exome sequencing results. Genet Med. 2017;19:1040–8.
Reuter C, Grove ME, Orland K, Spoonamore K, Caleshu C. Clinical cardiovascular genetic counselors take a leading role in team-based variant classification. J Genet Couns. 2018;27:751–60.
Wain KE, Azzariti DR, Goldstein JL, Johnson AK, Krautscheid P, Lepore B, et al. Variant interpretation is a component of clinical practice among genetic counselors in multiple specialties. Genet Med. 2020;22:785–92.
Biesecker LG, Biesecker BB. An approach to pediatric exome and genome sequencing. Curr Opin Pediatr. 2014;26:639–45.
Mazzola SE, O’Connor B, Yashar BM. Primary care physicians’ understanding and utilization of pediatric exome sequencing results. J Genet Couns. 2019;28:1130–8.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208.
IBM Corp. SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp. 2016.
Saldana J. The coding manual for qualitative researchers. 3rd edition. Thousand Oaks, CA: SAGE Publications; 2015.
Biesecker LG, Nussbaum RL, Rehm HL. Distinguishing variant pathogenicity from genetic diagnosis: how to know whether a variant causes a condition. JAMA. 2018;320:1929–30.
Helm BM, Ayers MD, Kean AC. All along the watchtower: a case of long QT syndrome misdiagnosis secondary to genetic testing misinterpretation. J Genet Couns. 2018;27:1515–22.
Macklin SK, Jackson JL, Atwal PS, Hines SL. Physician interpretation of variants of uncertain significance. Fam Cancer. 2018;18:121–6.
Donohue KE, Gooch C, Katz A, Wakelee J, Slavotinek A, Korf BR. Pitfalls and challenges in genetic test interpretation: an exploration of genetic professionals experience with interpretation of results. Clin Genet. 2021;99:638–49.
Marchant G, Barnes M, Evans JP, LeRoy B, Wolf SM. LawSeq Liability Task Force. From genetics to genomics: facing the liability implications in clinical care. J Law Med Ethics. 2020;48:11–43.
Wain KE, Palen E, Savatt JM, Shuman D, Finucane B, Seeley A, et al. The value of genomic variant ClinVar submissions from clinical providers: beyond the addition of novel variants. Hum Mutat. 2018;39:1660–67.
Segal MM. Genome interpretation: clinical correlation is recommended. Appl Transl Genom. 2015;6:26–27.
Acknowledgements
We thank the participants in the survey and interviews for sharing their behaviors and experiences. This work was funded by a Chairman’s Award from Children’s Mercy Hospital and by Genomic Answers for Kids.
Author information
Authors and Affiliations
Contributions
Conceptualization: C.B., E.A.H., L.W., K.G., E.F. Data curation: C.B., E.A.H., E.F. Formal analysis: C.B., E.A.H., E.F. Funding acquisition: T.P., E.F. Investigation: C.B., E.A.H., E.F. Methodology: C.B., E.A.H., L.W., I.T., C.S., K.G., E.F. Project administration: C.B., E.A.H., E.F. Supervision: T.P., K.G., E.F. Visualization: C.B., E.F. Writing—original draft: C.B., E.F. Writing—review and editing: C.B., E.A.H., I.T., C.S., K.G., E.F.
Corresponding author
Ethics declarations
ETHICS DECLARATION
All studies were approved by the Children’s Mercy Institutional Review Board (IRB) (#17080496 and #1701332). Informed consent was obtained from all survey and interview participants as required by the IRB, with a waiver of documentation of informed consent. Data for the chart review were collected with a waiver of consent and HIPAA authorization granted by the IRB. Data collected in the survey were de-identified. Data collected in the interviews and chart review were de-identified for analysis, but links to identifiers were maintained.
Competing interests
E.F. is on a Clinical Expert Panel for Whole Genome Sequencing for Illumina, Inc., etc. The other authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Berrios, C., Hurley, E.A., Willig, L. et al. Challenges in genetic testing: clinician variant interpretation processes and the impact on clinical care. Genet Med 23, 2289–2299 (2021). https://doi.org/10.1038/s41436-021-01267-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41436-021-01267-x