Abstract
Introduction
Carbapenem-resistant Enterobacteriaceae (CRE) has emerged as a global threat to hospitalization patients. Infected pancreatic necrosis (IPN) leads to high risks of CRE infections with increasing mortality. Our study aims to determine the predictors related to 90-day overall mortality of CRE IPN.
Methods
We retrospectively reviewed the drug resistance rates and clinical characteristics of CRE IPN patients from January 1, 2016, to January 1, 2021. Independent predictors of mortality were identified via univariate and multivariate analyses.
Results
During the 5-year period, 75 IPN patients suffered from 135 episodes of CRE infections with mortality up to 50.7%. CRE strains were highly resistant (> 50%) to nine of ten common antibiotics, except tigecycline (18%). The most common pathogen was carbapenem-resistant Klebsiella pneumoniae (84 of 135). Lung was the main site of extrapancreatic infections, followed by bloodstream and biliary tract. The independent predictors of mortality were Sequential Organ Failure Assessment (SOFA) score > 2 (hazard ratio 3.746, 95% confidence interval 1.209–11.609, P = 0.022) and procalcitonin > 6 ng/l (hazard ratio 2.428, 95% confidence interval 1.204–4.895, P = 0.013).
Conclusion
CRE is widespread as a global challenge with a high mortality rate among IPN patients due to limited therapeutic options. Carbapenem-resistant K. pneumoniae is the leading category of CRE which requires more attention in clinical practice. High SOFA score and procalcitonin level represent two independent predictors of mortality in CRE IPN patients. Greater efforts are needed toward timely therapeutic intervention for CRE IPN.
Similar content being viewed by others
Why carry out this study? |
Carbapenem-resistant Enterobacteriaceae-infected pancreatic necrosis is a life-threatening complication of acute pancreatitis. |
This study aimed to investigate the predictors of mortality among this population to improve the clinical outcomes. |
What was learned from the study? |
Carbapenem-resistant Enterobacteriaceae is widespread as a global challenge with a high mortality rate among infected pancreatic necrosis patients due to limited therapeutic options. |
Carbapenem-resistant Klebsiella pneumoniae is the leading category of carbapenem-resistant Enterobacteriaceae which requires more attention in clinical practice. |
High Sequential Organ Failure Assessment score and procalcitonin level represent two independent predictors of mortality. |
Introduction
Acute pancreatitis (AP), one of the most common gastrointestinal diseases, has a varying clinical course with mortality up to 40% [1]. In the past decade, considerable changes in therapy for AP resulted in the reduction of mortality rate [2]. Complicated infections, including pancreatic and extrapancreatic infections, have gradually replaced systemic inflammatory reaction syndromes as the predominant cause of mortality [3]. AP patients have become a particularly vulnerable population and are at high risk of multidrug-resistant (MDR) bacterial infections due to early anti-inflammatory drugs and antimicrobial overuse.
The crisis of MDR bacterial infection is more frequently occurring in developing countries including China where more than half of strains are MDR [4, 5]. Most publications have shown that MDR bacterial infections are significantly associated with increased mortality among AP patients, and gram-negative bacteria have replaced the gram-positive isolates as the dominating bacteria in AP patients [3, 6,7,8,9]. Carbapenems are considered as last option for MDR gram-negative bacterial infections including Enterobacteriaceae. The Guideline of the American College of Gastroenterology supports the use of carbapenems in AP patients for infected pancreatic necrosis (IPN) based on the microbiologic profile and necrotic tissue penetration ability [10]. However, with the indiscriminate use of carbapenems, carbapenem-resistant Enterobacteriaceae (CRE), one of the most dangerous pathogens, has emerged as a serious global threat to hospitalization patients with limited therapeutic options and a high mortality rate [11]. Overused prophylactic antibiotic treatments for ‘suspected’ IPN could result in the acquisition of MDR or carbapenem resistance [1]. Precious studies reported that CRE, as a mainly infectious MDR pathogen, has spread worldwide and influenced the outcome of IPN patients especially in India and China [7, 12,13,14,15,16].
In recent years, although a step-up approach has been rapidly accepted and recognized as the preferred method for IPN treatments, both the step-up approach and open necrosectomy have been widely adopted regimens, being chosen based on the disease progress [17]. Shenvi et al. found that markers of inflammation may be helpful to determine the timing and choice of IPN therapeutic intervention [18]. Despite recent clinical research focused on MDR IPN among AP patients, there are still important knowledge gaps and a lack of accurate clinical data among the CRE IPN population [7, 8, 12].
To our knowledge, no literature has been published in this area, and our retrospective cohort study was the first to focus on the clinical manifestations and microbiologic profile among IPN patients complicated with CRE infections. Herein, as the first cohort study investigating CRE IPN among AP patients, our objectives were to: (1) identify the predictor of poor outcomes to improve the survival and prognosis and (2) summarize drug resistance to shed light on the antibiotic therapy.
Methods
Study Design and Setting
A retrospective cohort study enrolled 75 IPN patients who were confirmed to have CRE infections from January 1, 2016, to January 1, 2021, in two tertiary teaching hospitals, Xiangya Hospital, Central South University, a 3500-bed tertiary-care teaching hospital, and Third Xiangya Hospital, Central South University, an 1800-bed tertiary-care teaching hospital, both in Hunan, China. Clinical characteristics included etiology and classification of AP, age, site of infections, sex, length of hospitalization, referral, antibiotic therapy and therapeutic intervention for IPN. Sequential Organ Failure Assessment (SOFA) score and laboratory records were collected and analyzed within the first 24 h after the therapeutic interventions for CRE IPN. The follow-up period for all patients was 90 days after the therapeutic intervention. As Fig. S1 shows, the outcomes were divided into alive and death groups for risk analysis.
Ethics
Informed consents were waived for all the patients because of the retrospective nature. Ethical approvals of this retrospective cohort study were granted by the Institutional Review Board of Xiangya Hospital (no. 202105092) and Third Xiangya Hospital (no. 21048).
Patients and Management Protocol
Patients between 18 and 80 years old were enrolled. Patients without therapeutic intervention of IPN or only positive result of extra-pancreatic infections were excluded. At the initial admission, all patients were assessed and managed via the multi-disciplinary team, including gastroenterology physicians, intensive care unit physicians and pancreatic surgeons, according to the latest international guidelines [19]. Fine-needle aspiration was never used for diagnosis of IPN in either medical center. For the treatment of IPN, the step-up approach, including surgical and endoscopic techniques, was the preferred strategy, but open necrosectomy was also adopted in our cohort based on the patients’ conditions, such as no opportunity for the step-up approach [20]. The antibiotic therapy we recorded in this cohort was the initial regimen after obtaining the microbiology profile of IPN. Carbapenem (high-dose, extended infusion) was considered an effective anti-infective choice for initial therapy. Tigecycline was prescribed as 50 mg every 12 h (100 mg the first time).
Definitions
Diagnosis and classification of AP were done according to the Revised Atlanta Classification [21]. Criteria of etiology were as follows: (1) hypertriglyceridemia: triglycerides > 5.6 mmol/l without other known cause; (2) gallstone: cholelithiasis or choledocholithiasis via contrast-enhanced computerized tomography; (3) alcoholism: regular consumption of alcohol (at least 50 g/day) [22]. The diagnoses of CRE IPN were based on: (1) contrast enhanced computed tomography; (2) positive microbiologic profiles from (peri)pancreatic necrosis obtained by the first therapeutic interventions [6]. Referrals were defined as patients transferred from lower-level hospitals 48 h after the AP occurred. Isolations of CRE were defined as positive specimens obtained from blood, bronchoalveolar fluid, bile and the first drainage of the IPN [11]. For anti-infective therapy, we recorded the antibiotic treatment at the initial choice (3–5 days). If the patient conditions worsened, we changed or combined new antibiotics as soon as possible. Sites of infection were diagnosed according to clinical manifestations and positive microbiologic profiles based the criteria of the Centers for Disease Control [23]. SOFA score was calculated based on the latest recommended guideline to assess the hazard of mortality in the first 24 h after the therapeutic intervention [24].
Microbiology
Identification of CRE was performed via the Vitek-2 system (bioMérieux, Marcy L’etoile, France). Drug susceptibility and minimum inhibitory concentration were determined and measured by Kerby-Bauer disk diffusion and agar dilution, respectively. All the antimicrobial reagents were products of Oxoid Ltd. Carbapenem-resistance was defined as acquired nonsusceptibility to meropenem or imipenem (minimal inhibitory concentration ≥ 2 mg/l) [11]. Drug resistances of polymyxin and ceftazidime-avibactam were not described, because our hospitals did not perform the drug resistance tests of these two antibiotics until 2020 and most patients in our cohort did not take this test. Intermediate susceptibility in vitro was considered resistance to the antibiotic.
Statistical Analysis
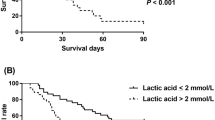
Continuous variables, compared with Student's t-test or Mann–Whitney U-test, were expressed as mean ± standard deviation, and categorical variables were compared with the χ2 test or Fisher exact tests in the univariate analysis. All the variables with P < 0.05 in the univariate analysis were entered into the multivariate Cox regression analysis to determine independent predictors of mortality. Hazard ratio (HR) and 95% confidence interval (CI) were performed to assess the power of predictors. We described the survival distribution among all the independent predictors via Kaplan-Meier curve. P-value < 0.05 (two-tailed) was considered statistically significant, and all the statistical analyses were performed via SPSS 24.0 (IBM SPSS Statistics, IBM Corp., Armonk, NY, US).
Results
Over the 5-year period, 3960 AP patients were admitted: 2693 mild AP, 1069 moderately severe AP and 198 severe AP patients; There were 1.9% AP patients (75 of 3960), in 472 because of pancreatic necrosis, who suffered from CRE IPN with a mortality rate up to 50.7% (38 of 75). Fifty-two patients (69.3%) were male with a mean age of 49.1 ± 12.7 years. Hypertriglyceridemia (n = 27, 36.0%) was the main etiology in this AP cohort, followed by gallstone (n = 25, 33.3%), alcoholism (n = 5, 6.7%) and others (n = 18, 24.0%). Sixty-five patients (86.7%) were referred from other hospitals after 48 h from the onset of AP. Thirty-eight patients (50.7%) received therapeutic interventions with positive specimens of CRE within 30 days from the onset of AP. Sixty patients first had positive results from IPN, and the remaining patients (n = 15) suffered from antecedent extrapancreatic infections before developing IPN. For antibiotic therapy, carbapenem (high dose, extended infusion) or carbapenem combined with tigecycline were the main choices in 28 and 26 patients, respectively. Step-up approach (percutaneous catheter drainage to minimal access retroperitoneal necrosectomy) was the most common therapeutic intervention for IPN. These data were not significantly different between the survival and mortality group.
In the univariate analysis, 54 patients, including 35 deaths, were classified into severe AP, and the remaining 21 patients had moderately severe AP (P < 0.001). According to the microbiologic profile, 33 patients had multisite infections (P = 0.024). SOFA score > 2 (P < 0.001), procalcitonin > 6 ng/l (P < 0.001), bacteremia (P = 0.001) and hemorrhage (P < 0.001) were also significantly associated with mortality (Table 1).
In the multivariate analysis, only SOFA score > 2 (HR 3.746, 95% CI 1.209–11.609, P = 0.022) and procalcitonin > 6 ng/l (HR 2.428, 95% CI 1.204–4.895, P = 0.013) were independent predictors of overall mortality (Table 2). The survival time and Kaplan-Meier curve of patients with independent predictors are described in Fig. 1. For the outcome of patients with SOFA score > 2 versus ≤ 2, the survival rate in the SOFA score > 2 group was significantly lower (29.2% vs. 85.2%, P < 0.001). Compared with the procalcitonin ≤ 6 ng/l group, the survival rate was significantly lower in the procalcitonin > 6 ng/l group (16.7% vs. 64.7%, P < 0.001).
In total, 135 CRE strains were detected among all 75 AP patients in our cohort (Table 3). Klebsiella pneumoniae (n = 84), Escherichia coli (n = 21) and Klebsiella ozaenae (n = 17) were the main CRE strains. Lung was the main site of extrapancreatic infections, followed by bloodstream and biliary tract. Drug resistance rates of each category and total are shown in Table 4. CRE strains were highly resistant (> 50%) to nine of ten common antibiotic categories, except tigecycline (18%). As the secondary common pathogen, E. coli was less resistant than the total. On the other hand, resistance rates of K. pneumoniae were higher than the total.
Discussion
Over the past decade, CRE has caused life-threatening infections with high mortality and economic burden in the global healthcare systems [11, 25]. AP patients, especially those complicated with IPN, are vulnerable to many potential risk factors associated with acquisition of MDR bacterial or CRE infections, such as overuse of prophylactic antibiotics, longer length of hospitalizations and anti-inflammatory conditions [3, 9, 14]. To date, this is the first cohort study focusing on the predictor of mortality and drug resistance rate among CRE IPN patients.
Mortality of IPN patients with CRE infections (50.7%) in our cohort was much higher than in those with MDR bacterial infections as Ning et al. reported (35.2%), indicating that CRE infections had greater hazards [3]. In line with Li et al., hyperlipidemia (n = 27, 36.0%) was the most common primary etiology among Chinese AP patients complicated with CRE infections in our cohort [9]. Unhealthy lifestyles, such as eating spicy foods and high-fat diets, may be a possible reason contributing to the high proportion of hyperlipidemia in China. However, the difference in the etiologic factors was not statistically significant in our study (P = 0.628).
Antibiotic therapy was used before having a clear microbiologic profile, but duration of antibiotic treatment was often dependent on the potency of infectious source control in the process of IPN treatment [13]. Recent guidelines recommended performing first procedures once walled-off necrosis occurs instead of 4 weeks later, because long-term conservative treatment can increase the risk of MDR bacterial and invasive fungal infections [26]. Furthermore, some IPN patients could die because of severe infections within 4 weeks. In line with Shenvi et al., the timing of the first intervention, whether > or < 30 days, was not associated with mortality in our cohort, and it may be more appropriate to choose the timing based on the respective clinical situations rather than general criteria [18].
Main findings of our study were: SOFA score > 2 and procalcitonin > 6 ng/l at the therapeutic intervention of IPN are first reported as independent predictors of mortality among IPN patients with CRE infections. SOFA score that assesses organ failure can be an indicator of septic shock in critical illness, which has already been validated in AP patients with infections [27, 28]. Higher SOFA score not only represents multi-organ dysfunction, but also objectively indicates the severity of sepsis. However, there is still no report on the relationship between a high SOFA score and outcomes in CRE IPN patients. Our study first provided this important evidence suggesting clinicians should observe the SOFA score at the pre-intervention phase. Yunus et al. proved that procalcitonin is a valuable marker of infection and is positively associated with the degree of infection [29]. Our result also revealed the key role of procalcitonin in the clinical evaluation, which alerts us to monitor procalcitonin and carry out anti-infective therapy in a timely manner. These two independent predictors may be potential clinical markers of IPN, which needs to be verified in a further randomized trial such as the POINTER trial [30].
Consistent with recent guidelines emphasizing early treatment within the first 72 h from onset of AP, Muktesh et al. found that delayed referral (> 7 days) resulted in poor outcomes [1, 31]. The high referral rate (n = 65, 86.7%) in our cohort was not surprising, as our centers are the most famous hospitals in Hunan Province and are preferred by critically ill patients from the surrounding area. Referral, after 48 h of onset, was not associated with the mortality (P = 0.526), which may suggest a 48-h delay could be an acceptable time because of increasing quality of therapy in lower-level hospitals. Most Chinese doctors, including those in our two centers, indiscriminately used antibiotic prophylaxis in the AP patients with ‘suspect’ infections, which may do harm in natural courses and lead to the occurrence of MDR bacterial IPN [13, 32]. Recent guidelines also recommended not preventing IPN with antibiotic prophylaxis, but we could not analyze the impact of antibiotic prophylaxis on IPN because of the high referral rate and lack of important data before admission, which needs to be verified in the future [19].
In our study, carbapenem-resistant K. pneumoniae (CRKP) was the leading pathogen of CRE strains in line with a previous study focused on the bacterial category [8]. Bacterial colonization and translocation may be the main reasons for attribution of CRKP. In line with a previous study, drug resistance rates of CRKP were more serious than total CRE strains with limited antibiotic choices, which may alert physicians to pay more attention to the emergency hazard of CRKP [4]. Although only tigecycline kept a low resistance rate, we should also use these antibiotics with a microbiologic profile cautiously to preclude the occurrence of drug resistance according to our previous study [11]. Similar to Montravers et al., there was no significant difference between different antibiotic therapies in our cohort, indicating that anti-infective therapy was not related to mortality with a high risk of drug resistance [32]. In line with a previous study, carbapenem (high dose, extended infusion), piperacillin and quinolone may be recommended as anti-infective therapies for CRE IPN according to microbiology results because of effective penetration [13]. Recent guidelines recommended combination therapy as an effective choice for CRE intra-abdominal infection, but there is still no evidence for combination therapy focusing on efficacy and safety in CRE IPN, which was also not fully confirmed in our retrospective cohort [33]. Data on polymyxin, as the most effective antibiotic for CRE infections, was not available because only six patients in our cohort underwent the polymyxin-resistance test. This needs to be verified in the future. In the era of increasing drug resistance, the next step should be not only creating novel antibiotics, but also defining the resistance mechanisms and preventing infections.
There were several limitations in our study. First, the power of risk analysis for the influence of both antibiotic therapy and therapeutic intervention for IPN on outcomes (no statistical significance) was limited because of the small sample size. In addition, most patients suffered from co-infections and major complications, and we could only analyze the overall mortality but not exclude these patients from CRE-infection-related mortality because of the limited sample size. Second, our findings were derived from two large tertiary hospitals in China which may not be generalized to areas with lower prevalence of CRE infections. Third, we decided to exclude the ‘suspect’ IPN patients with positive extrapancreatic results instead of therapeutic intervention to obtain the positive (peri)pancreatic result, which may lead to a bias in the evaluation of extrapancreatic infections. Fourth, novel molecular technology or diagnostic method need to be used for underlying mechanisms and rapid diagnosis of infections in the future. Finally, some important variables, such as specific radiologic signs, persistent bacteremia and septic shock, were lacking because of the retrospective nature. According to the above limitations, our findings should be interpreted cautiously. This 5-year Chinese bi-centric cohort study may be beneficial because of its universally adopted findings but requires more validation in the future.
Conclusion
CRE is widespread as a global challenge with a high mortality rate among IPN patients due to limited antimicrobial therapy. CRKP is the leading category of CRE with a high drug resistance rate which requires more attention in clinical practice. High SOFA score and procalcitonin level represent two independent predictors of mortality in CRE IPN patients.
References
Boxhoorn L, Voermans RP, Bouwense SA, Bruno MJ, Verdonk RC, Boermeester MA, et al. Acute pancreatitis. The Lancet. 2020;396(10252):726–34.
van Brunschot S, Hollemans RA, Bakker OJ, Besselink MG, Baron TH, Beger HG, et al. Minimally invasive and endoscopic versus open necrosectomy for necrotising pancreatitis: a pooled analysis of individual data for 1980 patients. Gut. 2018;67(4):gutjnl-2016-13341.
Ning C, Huang G, Shen D, Bonsu AAFK, Ji L, Lin C, et al. Adverse clinical outcomes associated with multidrug-resistant organisms in patients with infected pancreatic necrosis. Pancreatology. 2019;19(7):935–40.
Wu D, Huang X, Jia C, Liu J, Wan Q. Clinical manifestation, distribution, and drug resistance of pathogens among abdominal solid organ transplant recipients with Klebsiella pneumoniae infections. Transpl Proc. 2020;52(1):289–94.
Fernandes G, Sridhar D. World bank and the global financing facility. BMJ 2017;358:j3395.
Jiang X, Shi J, Wang X, Hu Y, Cui Y. The impacts of infectious complications on outcomes in acute pancreatitis: a retrospective study. Mil Med Res. 2020;7(1):38.
Moka P, Goswami P, Kapil A, Xess I, Sreenivas V, Saraya A. Impact of antibiotic-resistant bacterial and fungal infections in outcome of acute pancreatitis. Pancreas. 2018;47(4):489–94.
Tian H, Chen L, Wu X, Li F, Ma Y, Cai Y, et al. Infectious complications in severe acute pancreatitis: pathogens, drug resistance, and status of nosocomial infection in a university-affiliated teaching hospital. Dig Dis Sci. 2020;65(7):2079–88.
Li X, Li L, Liu L, Hu Y, Zhao S, Sun J, et al. Risk factors of multidrug resistant pathogens induced infection in severe acute pancreatitis. Shock. 2020;53(3):293–8.
Tenner S, Baillie J, DeWitt J, Vege SS. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013;108(9):1400–15.
Wu D, Chen C, Liu T, Jia Y, Wan Q, Peng J. Epidemiology, susceptibility, and risk factors associated with mortality in carbapenem-resistant gram-negative bacterial infections among abdominal solid organ transplant recipients: a retrospective cohort study. Infect Dis Ther. 2021;10(1):559–73.
Fan N, Hu Y, Shen H, Liu S, Zhao G, Sun L, et al. Compositional and drug-resistance profiling of pathogens in patients with severe acute pancreatitis: a retrospective study. BMC Gastroenterol. 2020;20(1):405.
Wolbrink DRJ, Kolwijck E, Ten Oever J, Horvath KD, Bouwense SAW, Schouten JA. Management of infected pancreatic necrosis in the intensive care unit: a narrative review. Clin Microbiol Infect. 2020;26(1):18–25.
Lu J, Cao F, Ding Y, Wu Y, Guo Y, Li F. Timing, distribution, and microbiology of infectious complications after necrotizing pancreatitis. World J Gastroenterol. 2019;25(34):5162–73.
Garret C, Canet E, Corvec S, Boutoille D, Peron M, Archambeaud I, et al. Impact of prior antibiotics on infected pancreatic necrosis microbiology in ICU patients: a retrospective cohort study. Ann Intensive Care. 2020;10(1):82.
Jain S, Mahapatra SJ, Gupta S, Shalimar, Garg PK. Infected pancreatic necrosis due to multidrug-resistant organisms and persistent organ failure predict mortality in acute pancreatitis. Clin Transl Gastroenterol. 2018;9(10):190.
Husu HL, Kuronen JA, Leppäniemi AK, Mentula PJ. Open necrosectomy in acute pancreatitis–obsolete or still useful? World J Emerg Surg. 2020;15(1):21.
Shenvi S, Gupta R, Kang M, Khullar M, Rana SS, Singh R, et al. Timing of surgical intervention in patients of infected necrotizing pancreatitis not responding to percutaneous catheter drainage. Pancreatology. 2016;16(5):778–87.
Crockett SD, Wani S, Gardner TB, Falck-Ytter Y, Barkun AN, Crockett S, et al. American gastroenterological association institute guideline on initial management of acute pancreatitis. Gastroenterology. 2018;154(4):1096–101.
van Brunschot S, van Grinsven J, van Santvoort HC, Bakker OJ, Besselink MG, Boermeester MA, et al. Endoscopic or surgical step-up approach for infected necrotising pancreatitis: a multicentre randomised trial. The Lancet. 2018;391(10115):51–8.
Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, et al. Classification of acute pancreatitis—2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2012;62(1):102–11.
Mosztbacher D, Hanák L, Farkas N, Szentesi A, Mikó A, Bajor J, et al. Hypertriglyceridemia-induced acute pancreatitis: a prospective, multicenter, international cohort analysis of 716 acute pancreatitis cases. Pancreatology. 2020;20(4):608–16.
Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care–associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36(5):309–32.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315(8):801.
Segagni Lusignani L, Presterl E, Zatorska B, Van den Nest M, Diab-Elschahawi M. Infection control and risk factors for acquisition of carbapenemase-producing. A 5 year (2011–2016) case-control study. Antimicrob Resist Infect Control. 2020;9(1):18.
Working Group IAP/APA Acute Pancreatitis Guidelines. IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology. 2013;13(4):e1–e15.
Rasch S, Pichlmeier E, Phillip V, Mayr U, Schmid RM, Huber W, et al. Prediction of outcome in acute pancreatitis by the qSOFA and the new ERAP score. Dig Dis Sci. 2021. https://doi.org/10.1007/s10620-021-06945-z.
Seymour CW, Liu VX, Iwashyna TJ, Brunkhorst FM, Rea TD, Scherag A, et al. Assessment of clinical criteria for sepsis. JAMA. 2016;315(8):762.
Yunus I, Fasih A, Wang Y. The use of procalcitonin in the determination of severity of sepsis, patient outcomes and infection characteristics. PLoS ONE. 2018;13(11): e0206527.
van Grinsven J, van Dijk SM, Dijkgraaf MG, Boermeester MA, Bollen TL, Bruno MJ, et al. Postponed or immediate drainage of infected necrotizing pancreatitis (POINTER trial): study protocol for a randomized controlled trial. Trials. 2019;20(1):239.
Muktesh G, Samanta J, Kumar Singh A, Gupta P, Sinha SK, Kumar H, et al. Delayed referral increases the need for surgery and intervention in patients with acute pancreatitis. ANZ J Surg. 2020;90(10):2015–9.
Montravers P, Kantor E, Constantin J, Lefrant J, Lescot T, Nesseler N, et al. Epidemiology and prognosis of anti-infective therapy in the ICU setting during acute pancreatitis: a cohort study. Crit Care. 2019;23(1):393.
Mazuski JE, Tessier JM, May AK, Sawyer RG, Nadler EP, Rosengart MR, et al. The surgical infection society revised guidelines on the management of intra-abdominal infection. Surg Infect. 2017;18(1):1–76.
Acknowledgements
We thank Prof. Junxia Yan and Tubao Yang for their help in verifying the statistical analysis in our study.
Funding
This work and the journal’s rapid service fee were supported by Fundamental Research Funds for the Central Universities of Central South University (2021zzts0347), Hunan Provincial Innovation Foundation for Postgraduates and the National Natural Science Foundation of China (grant no. 81670589).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole and have given their approval for this version to be published.
Author Contributions
Jie Peng conceived and designed the study; Di Wu, Junjie Ding, Yan Jia, Huanmiao Liu, Zimeng Guo and Jie Xiao collected and cleaned the data; Di Wu analyzed the data, interpreted the results and wrote the first draft of the manuscript; Junjie Ding, Yan Jia, Huanmiao Liu, Zimeng Guo and Jie Xiao interpreted the results; all authors critically revised the manuscript and gave final approval for publication.
Disclosures
Di Wu, Jie Xiao, Junjie Ding, Yan Jia, Zimeng Guo, Huanmiao Liu and Jie Peng have nothing to disclose.
Compliance with Ethics Guidelines
Informed consents were waived for all patients because of the retrospective nature. Ethical approval of this retrospective cohort study was granted by the Institutional Review Board of Xiangya Hospital (no. 202105092) and Third Xiangya Hospital (no. 21048).
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wu, D., Xiao, J., Ding, J. et al. Predictors of Mortality and Drug Resistance Among Carbapenem-Resistant Enterobacteriaceae-Infected Pancreatic Necrosis Patients. Infect Dis Ther 10, 1665–1676 (2021). https://doi.org/10.1007/s40121-021-00489-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-021-00489-5