Abstract
Background
Multiple predictive models of mortality exist for acute-on-chronic liver failure (ACLF) patients that often create confusion during decision-making. We studied the natural history and evaluated the performance of prognostic models in ACLF patients.
Methods
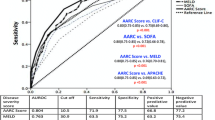
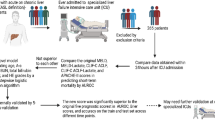
Prospectively collected data of ACLF patients from APASL-ACLF Research Consortium (AARC) was analyzed for 30-day outcomes. The models evaluated at days 0, 4, and 7 of presentation for 30-day mortality were: AARC (model and score), CLIF-C (ACLF score, and OF score), NACSELD-ACLF (model and binary), SOFA, APACHE-II, MELD, MELD-Lactate, and CTP. Evaluation parameters were discrimination (c-indices), calibration [accuracy, sensitivity, specificity, and positive/negative predictive values (PPV/NPV)], Akaike/Bayesian Information Criteria (AIC/BIC), Nagelkerke-R2, relative prediction errors, and odds ratios.
Results
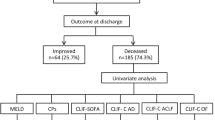
Thirty-day survival of the cohort (n = 2864) was 64.9% and was lowest for final-AARC-grade-III (32.8%) ACLF. Performance parameters of all models were best at day 7 than at day 4 or day 0 (p < 0.05 for C-indices of all models except NACSELD-ACLF). On comparison, day-7 AARC model had the numerically highest c-index 0.872, best accuracy 84.0%, PPV 87.8%, R2 0.609 and lower prediction errors by 10–50%. Day-7 NACSELD-ACLF-binary was the simple model (minimum AIC/BIC 12/17) with the highest odds (8.859) and sensitivity (100%) but with a lower PPV (70%) for mortality. Patients with day-7 AARC score > 12 had the lowest 30-day survival (5.7%).
Conclusions
APASL-ACLF is often a progressive disease, and models assessed up to day 7 of presentation reliably predict 30-day mortality. Day-7 AARC model is a statistically robust tool for classifying risk of death and accurately predicting 30-day outcomes with relatively lower prediction errors. Day-7 AARC score > 12 may be used as a futility criterion in APASL-ACLF patients.



Similar content being viewed by others
Abbreviations
- ACLF:
-
Acute-on-chronic liver failure
- MELD:
-
Model for end-stage liver disease
- APASL:
-
Asian Pacific Association for the Study of the Liver
- AARC:
-
APASL ACLF Research Consortium
- INR:
-
International normalized ratio
- LA:
-
Lactate
- OFs:
-
Organ failures
- CLIF-C:
-
Chronic Liver Failure Consortium
- NACSELD:
-
North American Consortium for the Study of End-Stage Liver Disease
- MELD-Na:
-
Model for end-stage liver disease-sodium
- CTP:
-
Child–Turcotte–Pugh
- SOFA:
-
Sequential organ failure assessment
- APACHE-II:
-
Acute physiology and chronic health evaluation
- C-index:
-
Concordance index
- PPV:
-
Positive predictive value
- AIC:
-
Akaike information criteria
- BIC:
-
Bayesian information criteria
- OR:
-
Odds ratio
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- CANONIC:
-
Chronic liver failure acute-on-chronic liver failure in cirrhosis
References
Jalan R, Perricone G, Moreau R, Arroyo V, Williams R. Acute-on-chronic liver failure: a new disease or an old one hiding in plain sight? Clin Liver Dis (Hoboken) 2020;15:S45–S51
Sarin SK, Choudhury A, Sharma MK, Maiwall R, Al Mahtab M, Rahman S, et al. Acute-on-chronic liver failure: consensus recommendations of the Asian Pacific association for the study of the liver (APASL): an update. Hepatol Int 2019;13:353–390
Choudhury A, Jindal A, Maiwall R, Sharma MK, Sharma BC, Pamecha V, et al. Liver failure determines the outcome in patients of acute-on-chronic liver failure (ACLF): comparison of APASL ACLF research consortium (AARC) and CLIF-SOFA models. Hepatol Int 2017;11:461–471
Moreau R, Jalan R, Gines P, Pavesi M, Angeli P, Cordoba J, et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology 2013;144:1426–1437, 1437.e1421–1429
Jalan R, Pavesi M, Saliba F, Amorós A, Fernandez J, Holland-Fischer P, et al. The CLIF Consortium Acute Decompensation score (CLIF-C ADs) for prognosis of hospitalised cirrhotic patients without acute-on-chronic liver failure. J Hepatol 2015;62:831–840
Drolz A, Horvatits T, Rutter K, Landahl F, Roedl K, Meersseman P, et al. Lactate improves prediction of short-term mortality in critically Ill patients with cirrhosis: a multinational study. Hepatology 2019;69:258–269
Jalan R, Saliba F, Pavesi M, Amoros A, Moreau R, Gines P, et al. Development and validation of a prognostic score to predict mortality in patients with acute-on-chronic liver failure. J Hepatol 2014;61:1038–1047
Bajaj JS, O’Leary JG, Reddy KR, Wong F, Biggins SW, Patton H, et al. survival in infection-related acute-on-chronic liver failure is defined by extrahepatic organ failures. Hepatology 2014;60:250–256
O’Leary JG, Reddy KR, Garcia-Tsao G, Biggins SW, Wong F, Fallon MB, et al. NACSELD acute-on-chronic liver failure (NACSELD-ACLF) score predicts 30-day survival in hospitalized patients with cirrhosis. Hepatology 2018;67:2367–2374
Sarmast N, Ogola GO, Kouznetsova M, Leise M, Bahirwani R, Maiwall R, et al. Model for end-stage liver disease-lactate and prediction of inpatient mortality in patients with chronic liver disease. Hepatology 2020;72:1747–1757
Kumar R, Krishnamoorthy TL, Tan HK, Lui HF, Chow WC. Change in model for end-stage liver disease score at two weeks, as an indicator of mortality or liver transplantation at 60 days in acute-on-chronic liver failure. Gastroenterol Rep (Oxf) 2015;3:122–127
Huo TI, Lin HC, Wu JC, Lee FY, Hou MC, Lee PC, et al. Proposal of a modified Child–Turcotte–Pugh scoring system and comparison with the model for end-stage liver disease for outcome prediction in patients with cirrhosis. Liver Transpl 2006;12:65–71
Duseja A, Choudhary NS, Gupta S, Dhiman RK, Chawla Y. APACHE II score is superior to SOFA, CTP and MELD in predicting the short-term mortality in patients with acute-on-chronic liver failure (ACLF). J Dig Dis 2013;14:484–490
Wlodzimirow KA, Eslami S, Abu-Hanna A, Nieuwoudt M, Chamuleau RA. A systematic review on prognostic indicators of acute on chronic liver failure and their predictive value for mortality. Liver Int 2013;33:40–52
Mahmud N, Kaplan DE, Taddei TH, Goldberg DS. Incidence and mortality of acute-on-chronic liver failure using two definitions in patients with compensated cirrhosis. Hepatology 2019;69:2150–2163
Wiesner R, Edwards E, Freeman R, Harper A, Kim R, Kamath P, et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology 2003;124:91–96
Bajaj JS, O’Leary JG, Reddy KR, Wong F, Olson JC, Subramanian RM, et al. Second infections independently increase mortality in hospitalized patients with cirrhosis: the North American consortium for the study of end-stage liver disease (NACSELD) experience. Hepatology 2012;56:2328–2335
Karvellas CJ, Garcia-Lopez E, Fernandez J, Saliba F, Sy E, Jalan R, et al. Dynamic prognostication in critically Ill cirrhotic patients with multiorgan failure in ICUs in Europe and North America: a multicenter analysis. Crit Care Med 2018;46:1783–1791
Rosenblatt R, Shen N, Tafesh Z, Cohen-Mekelburg S, Crawford CV, Kumar S, et al. The North American Consortium for the study of end-stage liver disease-acute-on-chronic liver failure score accurately predicts survival: an external validation using a national cohort. Liver Transpl 2020;26:187–195
Cárdenas A, Solà E, Rodríguez E, Barreto R, Graupera I, Pavesi M, et al. Hyponatremia influences the outcome of patients with acute-on-chronic liver failure: an analysis of the CANONIC study. Crit Care 2014;18:700
Pencina MJ, D’Agostino RB Sr, D’Agostino RB Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med 2008;27:157–172
Kuha J. AIC and BIC: comparisons of assumptions and performance. Sociol Methods Res 2004;33:188–229
Nagelkerke NJD. A note on a general definition of the coefficient of determination. Biometrika 1991;78:691–692
Norton EC, Dowd BE. Log odds and the interpretation of logit models. Health Serv Res 2018;53:859–878
Gustot T, Fernandez J, Garcia E, Morando F, Caraceni P, Alessandria C, et al. Clinical course of acute-on-chronic liver failure syndrome and effects on prognosis. Hepatology 2015;62:243–252
Shi Y, Yang Y, Hu Y, Wu W, Yang Q, Zheng M, et al. Acute-on-chronic liver failure precipitated by hepatic injury is distinct from that precipitated by extrahepatic insults. Hepatology 2015;62:232–242
Jeppesen JB, Mortensen C, Bendtsen F, Moller S. Lactate metabolism in chronic liver disease. Scand J Clin Lab Investig 2013;73:293–299
Puskarich MA, Trzeciak S, Shapiro NI, Albers AB, Heffner AC, Kline JA. Whole blood lactate kinetics in patients undergoing quantitative resuscitation for severe sepsis and septic shock. Chest 2013;143:1548–1553
Harrell FE Jr, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 1996;15:361–387
Choudhury A, Kumar M, Sharma BC, Maiwall R, Pamecha V, Moreau R, et al. Systemic inflammatory response syndrome in acute-on-chronic liver failure: relevance of ‘golden window’: a prospective study. J Gastroenterol Hepatol 2017;32:1989–1997
Acknowledgements
This work was presented as an oral presentation at the 29th Asian Pacific Association for the Study of the Liver (APASL) 2020 in Bali, Indonesia.
Funding
None.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants or legally acceptable representative of the participant included in the study.
Ethical approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Declaration of Helsinki 1975, as revised in 2008. The AARC registry for ACLF was approved by the Institutional Ethical Review board at the nodal centre i.e. ILBS New Delhi (vide letter no F/25/5/64/AC2013/912) and all the participating centers also had necessary approval from respective ethical board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Verma, N., Dhiman, R.K., Singh, V. et al. Comparative accuracy of prognostic models for short-term mortality in acute-on-chronic liver failure patients: CAP-ACLF. Hepatol Int 15, 753–765 (2021). https://doi.org/10.1007/s12072-021-10175-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-021-10175-w