Abstract
Purpose
The objective of this study was to develop a novel single opening&closing pulsatile flow in-vitro valve tester for direct measurement of closing volume of the heart valve.
Methods
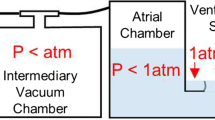
A single opening&closing valve tester was composed of a piston pump, valve mounting chamber, reservoir, measurement and control system. The piston pump was used to drive a valve to open and close with dictated flow which comprised three phases of accelerated, constant, and decelerated flow with six slopes. A high speed camera was used to record valve opening and closing images. Two pressure transducers across the tested valve were used to capture the ending time of valve closing which was verified by the high-speed photography. The closing time was measured and closing volume was calculated with a piston displacement volume during valve closing. A tilting disc valve and porcine mitral valve were tested.
Results
There was a big difference in flowrate between the Transonic flowmeter and piston pump. The heart valve opened and closed under the dictated flow driven by the piston pump. The transvalvular pressure was minor during valve opening and then increased sharply during valve closing. The closing time varied approximately linearly with the slope of the decelerated flow and was comparable between the two methods by the transvalvular pressure and high-speed photography. The closing volumes did not change much with the slope of the decelerated flow and were 7.0 ± 1.0 and 14.0 ± 1.5 mL for the tilting disc valve and mitral valve, respectively.
Conclusion
Pulsatile flow is challenging to the flowmeter. A novel single opening&closing pulsatile flow in-vitro valve tester for the heart valve has successfully been developed and can be used to simulate and evaluate the opening and closing hemodynamics of the heart valve. The tester can be used to measure valve closing volume and time accurately with a standardized testing protocol free from effect of other components such as the resistance, compliance units and auxiliary valve in the continuous pulsatile flow valve tester.









Similar content being viewed by others
References
Amini Khoiy, K., K. T. Asgarian, F. Loth, and R. Amini. Dilation of tricuspid valve annulus immediately after rupture of chordae tendineae in ex-vivo porcine hearts. PLoS ONE 13(11):2018. https://doi.org/10.1371/journal.pone.0206744.
Amini Khoiy, K., D. Biswas, T. N. Decker, K. T. Asgarian, F. Loth, and R. Amini. Surface strains of porcine tricuspid valve septal leaflets measured in ex vivo beating hearts. J. Biomech. Eng. 2016. https://doi.org/10.1115/1.4034621.
Annerel, S., T. Claessens, J. Degroote, P. Segers, and J. Vierendeels. Validation of a numerical FSI simulation of an aortic BMHV by in vitro PIV experiments. Med. Eng. Phys. 36(8):1014–1023, 2014. https://doi.org/10.1016/j.medengphy.2014.05.004.
Arjunon, S., P. H. Ardana, N. Saikrishnan, S. Madhani, B. Foster, A. Glezer, et al. Design of a pulsatile flow facility to evaluate thrombogenic potential of implantable cardiac devices. J. Biomech. Eng. 137(4):2015. https://doi.org/10.1115/1.4029579.
Beldi, G., A. Bosshard, O. M. Hess, U. Althaus, and B. H. Walpoth. Transit time flow measurement: experimental validation and comparison of three different systems. Ann. Thorac. Surg. 70(1):212–217, 2000. https://doi.org/10.1016/s0003-4975(00)01246-7.
Bloodworth, C. H., E. L. Pierce, T. F. Easley, A. Drach, A. H. Khalighi, M. Toma, et al. Ex vivo methods for informing computational models of the mitral valve. Ann. Biomed. Eng. 45(2):496–507, 2016. https://doi.org/10.1007/s10439-016-1734-z.
Chancellor, W. Z., S. A. Schubert, and G. Ailawadi. Transcatheter interventions for functional mitral regurgitation. Ann. Cardiothorac. Surg. 7(6):764–770, 2018. https://doi.org/10.21037/acs.2018.09.01.
Dasi, L. P., D. W. Murphy, A. Glezer, and A. P. Yoganathan. Passive flow control of bileaflet mechanical heart valve leakage flow. J. Biomech. 41(6):1166–1173, 2008. https://doi.org/10.1016/j.jbiomech.2008.01.024.
Easley, T. F., C. H. Bloodworth, V. Bhal, and A. P. Yoganathan. Effects of annular contraction on anterior leaflet strain using an in vitro simulator with a dynamically contracting mitral annulus. J. Biomech. 66:51–56, 2018. https://doi.org/10.1016/j.jbiomech.2017.10.045.
Garg, P., R. J. van der Geest, P. P. Swoboda, S. Crandon, G. J. Fent, J. R. J. Foley, et al. Left ventricular thrombus formation in myocardial infarction is associated with altered left ventricular blood flow energetics. Eur. Heart J. 20(1):108–117, 2019. https://doi.org/10.1093/ehjci/jey121.
Gheorghe, L., B. J. W. M. Rensing, J. A. S. Van der Heyden, F. D. Eefting, M. C. Post, B. Rana, et al. Transcatheter tricuspid valve interventions: an emerging field. Curr. Cardiol. Rep. 2019. https://doi.org/10.1007/s11886-019-1119-7.
Goode, D., R. Dhaliwal, and H. Mohammadi. Transcatheter mitral valve replacement: state of the art. Cardiovasc. Eng. Technol. 11(3):229–253, 2020. https://doi.org/10.1007/s13239-020-00460-4.
Gupta, T., D. Kolte, S. Khera, K. Goel, P. A. Villablanca, A. Kalra, et al. The changing landscape of aortic valve replacement in the USA. EuroIntervention. 15(11):e968–e974, 2019. https://doi.org/10.4244/EIJ-D-19-00381.
He, Z., Y. Liu, T. Jing, G. Zhang, H. Liu, and H. Wang. Heart valve model with controllable closing volume. J. Drain. Irrig. Mach. Eng. 2019. https://doi.org/10.3969/j.issn.1674-8530.17.0191.
He, Z., K. Zhang, and B. Gao. A novel coaptation plate device for functional mitral regurgitation: an in vitro study. Ann. Biomed. Eng. 42(10):2039–2047, 2014. https://doi.org/10.1007/s10439-014-1065-x.
He, Z., K. Zhang, T. Jing, and Y. Wang. Transapical coaptation plate for functional mitral regurgitation: an in vitro study. Ann. Biomed. Eng. 45(2):487–495, 2017. https://doi.org/10.1007/s10439-016-1726-z.
Hu, Y., L. Shi, S. Parameswaran, S. Smirnov, and Z. He. Left ventricular vortex under mitral valve edge-to-edge repair. Cardiovasc. Eng. Technol. 1(4):235–243, 2010. https://doi.org/10.1007/s13239-010-0022-6.
Jaworek, M., M. Piola, F. Lucherini, G. Gelpi, M. Castagna, G. Lentini, et al. Functional tricuspid regurgitation model in a beating heart platform. ASAIO J. 63(4):438–444, 2017. https://doi.org/10.1097/MAT.0000000000000510.
Jimenez, J. H., J. Forbess, L. R. Croft, L. Small, Z. He, and A. P. Yoganathan. Effects of annular size, transmitral pressure, and mitral flow rate on the edge-to-edge repair: an in vitro study. Ann. Thorac. Surg. 82(4):1362–1368, 2006. https://doi.org/10.1016/j.athoracsur.2006.05.008.
Kolte, D., and S. Elmariah. Current state of transcatheter tricuspid valve repair. Cardiovasc. Diagn. Ther. 10(1):89–97, 2020. https://doi.org/10.21037/cdt.2019.09.11.
Lee, C. S., K. B. Chandran, and L. D. Chen. Cavitation dynamics of mechanical heart valve prostheses. Artif. Organs. 18(10):758–767, 1994. https://doi.org/10.1111/j.1525-1594.1994.tb03315.x.
Leopaldi, A. M., R. Vismara, S. van Tuijl, A. Redaelli, F. N. van de Vosse, G. B. Fiore, et al. A novel passive left heart platform for device testing and research. Med. Eng. Phys. 37(4):361–366, 2015. https://doi.org/10.1016/j.medengphy.2015.01.013.
Li, M., N. A. Hotaling, D. N. Ku, and C. R. Forest. Microfluidic thrombosis under multiple shear rates and antiplatelet therapy doses. PLoS ONE 9(1):2014. https://doi.org/10.1371/journal.pone.0082493.
Luca, A., R. Marchiano, and J. C. Chassaing. Numerical simulation of transit-time ultrasonic flowmeters by a direct approach. IEEE Trans. Ultrason. Ferroelectr. Freq. Control. 63(6):886–897, 2016. https://doi.org/10.1109/TUFFC.2016.2545714.
Luraghi, G., W. Wu, F. De Gaetano, J. F. Rodriguez Matas, G. D. Moggridge, M. Serrani, et al. Evaluation of an aortic valve prosthesis: fluid-structure interaction or structural simulation? J. Biomech. 58:45–51, 2017. https://doi.org/10.1016/j.jbiomech.2017.04.004.
Lynnworth, L. C., and Y. Liu. Ultrasonic flowmeters: half-century progress report, 1955-2005. Ultrasonics. 44(Suppl 1):e1371–e1378, 2006. https://doi.org/10.1016/j.ultras.2006.05.046.
Midha, P. A., V. Raghav, I. Okafor, and A. P. Yoganathan. The effect of valve-in-valve implantation height on sinus flow. Ann. Biomed. Eng. 45(2):405–412, 2016. https://doi.org/10.1007/s10439-016-1642-2.
Muntane-Carol, G., A. Alperi, L. Faroux, E. Bedard, F. Philippon, and J. Rodes-Cabau. Transcatheter tricuspid valve intervention: coaptation devices. Front. Cardiovasc. Med. 7:139, 2020. https://doi.org/10.3389/fcvm.2020.00139.
Nordgaard, H. B., N. Vitale, R. Astudillo, A. Renzulli, P. Romundstad, and R. Haaverstad. Pulsatility index variations using two different transit-time flowmeters in coronary artery bypass surgery. Eur. J. Cardiothorac. Surg. 37(5):1063–1067, 2010. https://doi.org/10.1016/j.ejcts.2009.11.030.
Peruzzo, P., F. M. Susin, A. Colli, and G. Burriesci. In vitro assessment of pacing as therapy for aortic regurgitation. Open Heart. 6(1):2019. https://doi.org/10.1136/openhrt-2018-000976.
Piatti, F., F. Sturla, G. Marom, J. Sheriff, T. E. Claiborne, M. J. Slepian, et al. Hemodynamic and thrombogenic analysis of a trileaflet polymeric valve using a fluid–structure interaction approach. J. Biomech. 48(13):3641–3649, 2015. https://doi.org/10.1016/j.jbiomech.2015.08.009.
Pierce, E. L., K. Kohli, B. Ncho, V. Sadri, C. H. Bloodworth, F. E. Mangan, et al. Novel in vitro test systems and insights for transcatheter mitral valve design, Part II: radial expansion forces. Ann. Biomed. Eng. 47(2):392–402, 2018. https://doi.org/10.1007/s10439-018-02139-3.
Schmidt, R. F., and G. Thews. Human Physiology (2nd completely rev. ed.). Berlin: Springer, 1989.
Seemann, F., E. Heiberg, M. Carlsson, R. A. Gonzales, L. A. Baldassarre, M. Qiu, et al. Valvular imaging in the era of feature-tracking: A slice-following cardiac MR sequence to measure mitral flow. J. Magn. Reson. Imaging. 51(5):1412–1421, 2020. https://doi.org/10.1002/jmri.26971.
Sodhani, D., S. Reese, A. Aksenov, S. Soğanci, S. Jockenhövel, P. Mela, et al. Fluid-structure interaction simulation of artificial textile reinforced aortic heart valve: validation with an in-vitro test. J. Biomech. 78:52–69, 2018. https://doi.org/10.1016/j.jbiomech.2018.07.018.
Vismara, R., A. M. Leopaldi, M. Piola, C. Asselta, M. Lemma, C. Antona, et al. In vitro assessment of mitral valve function in cyclically pressurized porcine hearts. Med. Eng. Phys. 38(4):346–353, 2016. https://doi.org/10.1016/j.medengphy.2016.01.007.
Vismara, R., A. Pavesi, E. Votta, M. Taramasso, F. Maisano, and G. B. Fiore. A pulsatile simulator for the in vitro analysis of the mitral valve with tri-axial papillary muscle displacement. Int. J. Artif. Organs. 34(4):383–391, 2011. https://doi.org/10.5301/IJAO.2011.7729.
Warnock, J. N., S. Konduri, Z. He, and A. P. Yoganathan. Design of a sterile organ culture system for the ex vivo study of aortic heart valves. J. Biomech. Eng. 127(5):857–861, 2005.
Wu, C., N. Saikrishnan, A. J. Chalekian, R. Fraser, O. Ieropoli, S. M. Retta, et al. In-vitro pulsatile flow testing of prosthetic heart valves: a round-robin study by the ISO Cardiac Valves Working Group. Cardiovasc. Eng. Technol. 10(3):397–422, 2019. https://doi.org/10.1007/s13239-019-00422-5.
Yoganathan, A. P., Z. He, and Jones S. Casey. Fluid mechanics of heart valves. Annu. Rev. Biomed. Eng. 6(1):331–362, 2004. https://doi.org/10.1146/annurev.bioeng.6.040803.140111.
Zapanta, C. M., D. R. Stinebring, D. S. Sneckenberger, S. Deutsch, D. B. Geselowitz, J. M. Tarbell, et al. In vivo observation of cavitation on prosthetic heart valves. ASAIO J. 42(5):M550–M555, 1996. https://doi.org/10.1097/00002480-199609000-00047.
Zhang, R., X. Liu, S. Chen, S. Parameswaran, and Z. He. Mechanistic study of ventricular hook anchor for heart valve replacement or repair. Med. Novel Technol. Dev. 5:2020. https://doi.org/10.1016/j.medntd.2020.100033.
Zhang, G., H. Wang, T. Jing, and Z. He. Research of mitral valve model in the 0d left ventricular circulation system. Chin. J. Biomed. Eng. 36(03):300–307, 2017. https://doi.org/10.3969/j.issn.0258-8021.2017.03.006.
Author Contributions
HW contributed to conceptualization, performed the experiment, data analyses and wrote the manuscript; ZC performed the experiment; ZZ performed the analysis with constructive discussions; ZH contributed to the conception of the study.
Data Availability
The datasets used or analyzed during the current study are available from the corresponding author on reasonable request.
Conflict of interest
Hao Wang is the inventor of the single opening&closing tester. The other authors do not have conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Ajit P. Yoganathan oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, H., Cui, Z., Zhou, Z. et al. A Single-opening&closing Valve Tester for Direct Measurement of Closing Volume of the Heart Valve. Cardiovasc Eng Tech 13, 80–89 (2022). https://doi.org/10.1007/s13239-021-00560-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-021-00560-9