Abstract
A number of genes have been implicated in the pathogenesis of BCC in addition to the Hedgehog pathway, which is known to drive the initiation of this tumour. We performed in-depth analysis of 13 BCC-related genes (CSMD1, CSMD2, DPH3 promoter, PTCH1, SMO, GLI1, NOTCH1, NOTCH2, TP53, ITIH2, DPP10, STEAP4, TERT promoter) in 57 BCC lesions (26 superficial and 31 nodular) from 55 patients and their corresponding blood samples. PTCH1 and TP53 mutations were found in 71.9% and 45.6% of BCCs, respectively. A high mutation rate was also detected in CSMD1 (63.2%), NOTCH1 (43.8%) and DPP10 (35.1%), and frequent non-coding mutations were identified in TERT (57.9%) and DPH3 promoter (49.1%). CSMD1 mutations significantly co-occurred with TP53 changes (p = 0.002). A significant association was observed between the superficial type of BCC and PTCH1 (p = 0.018) and NOTCH1 (p = 0.020) mutations. In addition, PTCH1 mutations were significantly associated with intermittent sun exposure (p = 0.046) and the occurrence of single lesions (p = 0.021), while NOTCH1 mutations were more frequent in BCCs located on the trunk compared to the head/neck and extremities (p = 0.001). In conclusion, we provide further insights into the molecular alterations underlying the tumorigenic mechanism of superficial and nodular BCCs with a view towards novel rationale-based therapeutic strategies.
Similar content being viewed by others
Introduction
Basal cell carcinoma (BCC) is the most common epithelial skin cancer in Caucasian population1, 2, with 2.75 million cases per year estimated by the World Health Organization3. Incidence of BCC is rising of 5% per year in Europe and 2% annually in USA4, 5. BCCs are a heterogeneous group of tumours ranging from thin superficial papules or plaques and nodules, sometimes ulcerated, to the sclerosing/morpheic, basosquamous and infiltrating types4, 6,7,8. The superficial and nodular BCCs are non-aggressive, slow-growing lesions with low risk of recurrence, that account for 80% of BCC lesions, thus representing a growing healthcare issue9, 10.
The aberrant activation of the Hedgehog (Hh) pathway plays a pivotal role in the pathogenesis of BCC. In physiological condition, the Hh signalling is involved in cell type differentiation and proliferation, adult tissue homeostasis and repair with a fundamental mitogenic and morphogenic role9. In the absence of input signals, the twelve-pass transmembrane protein Patched 1 (PTCH1) lies in the cilia where it inhibits the Hh pathway activator G-protein coupled receptor Smoothened (SMO), thus blocking pathway activity. The binding of Hh ligands to PTCH1 results in activation of SMO allowing the release of the glioma-associated transcription factors (GLI) from their negative regulator Suppressor of fused11. The subsequent translocation of activated GLIs into the nucleus initiates the transcription of GLI-targeted genes involved in cell proliferation, cell cycle regulation, apoptosis, angiogenesis and self-renewal12. PTCH1 inactivating mutations have been identified in 70–90% of BCCs, while 10–20% of BCC lesions harbour activating mutations in the SMO gene13. Alterations in the cell cycle regulator TP53 gene are the second most prevalent tumorigenic event found in 44–65% of BCCs14, 15. Exome sequencing-based studies have shown that sporadic BCCs exhibit one of the highest prevalence rates of somatic mutations of all cancers (65 mutations/megabase), involving a number of additional Hh-unrelated genes14,15,16,17. These investigational studies revealed new potential BCC driver genes, although their contribution to the genetic network underlying tumorigenesis and tumour evolution is not yet completely explained.
We examined the molecular alterations across 13 genes, selected on the basis of their potential role in the pathogenesis of superficial and nodular tumour subtypes, in order to provide further insights into the molecular sub-classification of BCC lesions.
Results
Study cohort
Fifty-seven sporadic BCCs of 55 patients (27 males and 28 females; median age at diagnosis: 70 years, range 32–93 years) were included in the study. Demographic characteristics and clinico-pathologic features of patients and BCC lesions are illustrated in Table 1. Thirty-one patients had one BCC, 11 patients two BCCs and 13 patients > 2 BCCs. Anatomical sites of BCC lesions included the head/neck region (15/57, 26.3%), trunk (38/57, 66.7%) and extremities (4/57, 7.0%). Histopathologic examination showed that 26/57 (45.6%) were superficial BCCs and 31/57 (54.4%) nodular, with 47/57 BCCs (82.5%) having no ulceration.
Mutational screening
We analysed the mutational profile of 13 cancer genes (CSMD1, CSMD2, PTCH1, SMO, GLI1, NOTCH1, NOTCH2, TP53, ITIH2, DPP10, STEAP4, DPH3 promoter and TERT promoter) (Supplementary Table S1) in a total of 57 BCCs, including superficial and nodular subtypes. Somatic variants were detected across 7 genes (PTCH1, CSMD1, TP53, NOTCH1, TERT promoter, DPH3 promoter, DPP10), with the 98.2% (56/57) of BCCs showing at least one alteration (Fig. 1). Among all coding somatic mutations, 56% (135/241) were not previously published or reported in online variant databases. In silico prediction of protein functional effect and classification of novel variants are detailed in Supplementary Table S2. As for the 44% (106/241) of already reported variants, 69/106 (65.1%) were classified as pathogenic/likely pathogenic/oncogenic/likely oncogenic, 22/106 (20.8%) were variant of uncertain significance (VUS), and 15/106 (14.1%) were benign/likely benign/polymorphism.
Distribution of somatic variants across the mutated genes. Each row represents a gene and each column corresponds to individual samples. When multiple mutations were present in a gene, only the pathogenetic or probable pathogenetic mutation was considered and shown in the diagram generated with Oncoprinter in cBioPortal tool.
Overall, 81.0% of single-nucleotide variants (SNVs) were C > T changes, consistent with UV-induced mutagenesis.
PTCH1 mutations were found in 41/57 (71.9%) BCCs, with 16/57 (28.1%) lesions carrying more than one PTCH1 variants. Overall, 63 variants in the PTCH1 gene were identified, distributing within the entire coding sequence with no specific hotspot region (Fig. 2a). The most frequent nucleotide change was the C > T transition identified in 18/57(31.6%) tumours, followed by the CC > TT tandem variants in 8/57 (14.0%) and C > A mutations in 3/57 (5.3%) tumours. The majority (27/63, 42.9%) were truncating mutations, including 10 frameshift deletions and/or insertions and 17 nonsense mutations. All the identified truncating variants were included as likely oncogenic for clinical significance and likely loss-of-function for biological effect in the OncoKB database21, 22. In addition, missense mutations accounted for 20.6% (13/63) of PTCH1 variants. Among the identified PTCH1 missense mutations, the p.R195K and p.P568L are known for their pathogenic significance. Finally, 9 splice sites mutations (8/63, 14.3%) were found, 3 of which were not previously published or reported in online variant databases and predicted to be pathogenic based on the dbNSFP v4.1 applied prediction tools (Supplementary Table S2).
Mutational profiles interpreted with protein annotation. The protein figure was generated with MutationMapper in cBioPortal tool. Alterations occurring two and/or more times are specified in the protein domains. (a) PTCH1: the sterol-sensitive and Patched family functional protein domains are represented by green and red boxes, respectively. (b) TP53: the transactivation, DNA-binding and tetramerization domains are represented by green, red and blue boxes, respectively. (c) CSMD1: the CUB and SUSHI domains are represented by green and red boxes, respectively. (d) NOTCH1: the EGF-like domains are represented by green boxes. (e) DPP10: the dipeptidyl peptidase N-terminal domain is represented by green box.
TP53 mutations were found in 26/57 (45.6%) BCCs, with hot spot positions including p.H179, p.S241, p.G245 and p.R280 (Supplementary Table S2)24. Single nucleotide missense variants clustering in the DNA binding domain (95–288 ammino-acid residues) were the most prevalent (15/30, 50.0%), and truncating mutations (all nonsense except for one frameshift deletion) represented 33.3% (10/30) of alterations (Fig. 2b).
In addition, mutations in CSMD1 gene were identified in 36 of 57 (63.2%) BCCs, with missense mutations being the most prevalent (68/85, 80.0%). More than one CSMD1 alterations was found in 22/57 (38.6%) tumours, and 5/57 BCCs (8.8%) harboured more than six CSMD1 somatic mutations. All the identified CSMD1 point mutations were unknown for oncogenic significance. However, the dbNSFP v4.1 tool predicted that 32.9% (28/85) of CSMD1 alterations were deleterious for protein function (Supplementary Table S2), including the most recurrent p.R671C (c.2011C > T) amino-acid change, which was detected in 3/57 (5.3%) BCC lesions (Fig. 2c).
NOTCH1 mutations were found in 25/57 (43.8%) BCCs. In total, we detected 35 NOTCH1 mutations, including truncating (14/35, 40.0%) and missense variants (13/35, 37.1%). Of the 35 identified mutations, 5 (5/35, 14.3%) referred to a COSMIC identifier (Supplementary Table S2) and 16 (16/35, 45.7%) are known oncogenic or predicted oncogenic according to the OncoKB database (Fig. 2d).
Mutations in DPP10 were detected in 35.1% (20/57) of BCCs, with missense variants being the most frequent mutational event (20/30, 66.7%) (Fig. 2e).
Eight TERT promoter mutations were found in 33/57 (57.9%) BCC lesions. The most frequent somatic change was the -146 C > T, which was detected in 19/57 BCCs (33.3%), followed by the -124 C > T transition and the -138/139 CC > TT tandem variation accounting for 8.8% (5/57) and 5.3% (3/57) of BCC lesions, respectively. Supplementary Table S3 illustrates all TERT mutations.
Overall, 9 DPH3 promoter mutations were identified in 49.1% (28/57) of BCCs. The most prevalent variant was the -121C > T transition (19/57, 33.3%), followed by the -122 C > T (4/57, 7.0%), -125 C > T (2/57, 3.5%) and -150 C > T (2/57, 3.5%) (Supplementary Table S3).
Statistical analysis of the mutational profile
We performed pairwise exclusivity and co-occurrence analysis for the 7 identified mutated loci (DPP10, CSMD1, PTCH1, NOTCH1, TP53, TERT promoter, DPH3 promoter) and found significant concurrent variants of TP53 gene with CSMD1 (p = 0.002), PTCH1 (p = 0.011) and DPH3 promoter (p = 0.006) (Fig. 1). However, after Benjamini–Hochberg false discovery rate (FDR) correction, only the association of CSMD1 variants with the TP53 mutation rate remained significant (q = 0.045).
By evaluating the distribution of somatic alterations within 7 different mutated genes across 57 BCC lesions, we identified 43 different combinations. Among them, the two most frequent (4/57; 7.0%) were: 1) concurrent PTCH1 and TERT promoter mutations in a setting of wild type DPP10, CSMD1, NOTCH1, TP53 and DPH3 promoter genes, BCCs, and 2) the coexistence of DPP10, CSMD1, PTCH1, NOTCH1, TP53, TERT promoter and DPH3 promoter mutations. None of these two most frequent combinations were significantly associated with superficial or nodular subtypes (p = 0.117).
Focusing on the analysis of single mutated gene according to the specific BCC subtypes, PTCH1 and NOTCH1 mutations were found significantly associated with superficial BCCs (p = 0.018 and p = 0.020, respectively). In details, PTCH1 variants were 1.6 times (OR = 5.537, 95% CI = 1.367–22.43) and NOTCH1 mutations 2.0 times more frequent (OR = 4.457, 95% CI = 1.304–15.24) in superficial than in nodular BCCs.
The Principal Component Analysis (PCA) multivariate approach confirmed a significant association between PTCH1 mutations and the superficial BCC subtypes that were recognized as genetically similar group for PTCH1 mutations in a separate cluster of the PCA diagram (Fig. 3).
Two-dimensional principal component analysis (PCA) of genetic variations among superficial and nodular subtypes. Each sample was characterized as a distinct dot in a vector space. PTCH1 mutations characterized the superficial BCC types that clustered on the top right of the graph (PTCH1 arrow). Over 47% of the variance in genetic profile data sets were accounted for by the first two components: PC1 (29%) and PC2 (18%).
The analysis of the mutational status according to patients and tumour characteristics revealed that PTCH1 mutations were significantly associated with intermittent sun exposure (p = 0.046), and with the occurrence of single BCC lesions (p = 0.021), and NOTCH1 mutations were more frequent in BCCs arising on the trunk compared to the head/neck and extremities (p = 0.001).
Discussion
Our in-depth analysis was focused on a panel of 13 genes potentially associated to BCC tumorigenesis. We showed a high prevalence of Hh pathway mutations and a high rate of mutations in CSMD1, NOTCH1 and DPP10 genes, and in TERT and DPH3 promoter regions. Interestingly, NOTCH1 and PTCH1 mutations were significantly more frequent in superficial than in nodular BCCs, and CSMD1 mutations occurred along with TP53 changes. PTCH1 alterations were significantly associated with intermittent sun exposure and with the development of a single BCC, while NOTCH1 mutations with location on the trunk.
In line with previous studies14,15,16,17, 25, 26, 98.2% of BCCs showed at least one alteration among the analysed genes. PTCH1 and TP53 mutations were found in 71.9% and 45.6% of BCCs, respectively, being UV-fingerprint mutations (C > T and CC > TT transitions) the most common. Moreover, multiple PTCH1 and TP53 mutations were found in 28.0% and 17.6% of BCC lesions, respectively. We identified eight PTCH1 splice site mutations including the c.1347 + 1G > A and c.1216-2A > T, which have been recently recognized as novel PTCH1 variants27, probably pathogenic according to Associations for Clinical Genetic Science and American College of Medical Genetics and Genomics criteria28, 29. Notably, a significant association was found between PTCH1 mutations and the superficial BCC type that was further confirmed by the PCA multivariate statistical approach. This is in line with evidences that topical imiquimod, which has been shown to negatively regulate Hh signalling30, is a successful treatment for superficial BCC. Moreover, a clinical trial is investigating the efficacy of topical patidegib, a novel topical Hh inhibitor, to decrease the number of surgically eligible BCC lesions in patients with multiple BCCs (NCT04155190)31. We found no mutations in SMO gene in our BCC samples, in contrast with the 10–20% frequency rate previously described13,14,15,16,17. Notably, this discrepancy might reflect clinical differences in the patient population: in our study only treatment-naïve patients have been included in the analysis while previous study showed a 2.2-fold higher frequency of SMO mutations in vismodegib-resistant compared to treatment-naïve sporadic BCCs (P = 5 × 10 − 2, Fisher’s exact test)14.
In addition to the established BCC-associated genes, we identified high frequency of mutations in CSMD1, NOTCH1, DPP10, TERT promoter and DPH3 promoter genes. CSMD1 gene, encoding an inhibitor of the complement system, is believed to act as a tumour suppressor gene whose functions seems to be inactivated in many cancers32,33,34,35. Consistently with previous data14, 15, we detected CSMD1 somatic mutations in 63.2% of BCCs, thus representing the second most prevalent mutated genes after PTCH1. In addition, 38.6% of BCCs harboured more than one CSMD1 alterations. It is conceivable that, under the selective pressure during cancer development, multiple CSMD1 variants reside in separate subclones within the same tumour population. Notably, we found a significant association of CSMD1 alterations with TP53 mutation rate, which was previously described in mucosal head and neck squamous cell carcinoma33. The increased cellular proliferation driven by TP53 loss, might provide CSMD1 mutant clone to sufficiently expand.
NOTCH signalling pathway in physiological condition plays a critical role in the regulation of cell differentiation, self-renewal and homeostasis primarily controlling the interplay between adjacent cells36, while in cancer can function as either an oncogene or tumour suppressor gene depending on the cell type and context37, 38. Shi et al.39 demonstrated that NOTCH pathway activity is suppressed in BCCs highlighting its tumour suppressor function in human epithelial malignancies. Moreover, NOTCH1 loss-of-function mutations were found to specifically promote tumour persistence in sporadic BCCs suggesting therapeutic restoring of the NOTCH tumour-suppressor function as a potential approach to eradicate persistent tumour cells40. Previous reports found NOTCH1 loss-of-function alterations (missense, truncating or loss of heterozygosity) in 30–50% of BCCs14, 15, 25. In our study, NOTCH1 mutations were found in 43.8% of BCC lesions and were mainly inactivating alterations, which support the tumour-suppressor role of NOTCH1 in BCC tumorigenesis. Interestingly, we found that NOTCH1 mutations were 2-times more frequent in superficial BCCs than in nodular subtypes, suggesting that tumorigenic pathways may differ across BCC subtypes.
The DPP10 gene encodes a trans-membrane protein, which regulates potassium channels activity involved in cell proliferation and apoptosis41. We found mutations of DPP10 gene in 35.1% of BCCs, while a previous study on 12 BCCs showed mutations in 75% of cases15. Such difference in frequency rate might be due to the sample size or different subtypes of BCC lesions analysed.
Noncoding somatic mutations of TERT promoter are emerging to have a crucial pathogenetic role in BCCs. TERT non-coding mutations were previously identified in 39–74% of BCCs and considered to contribute to telomeres length maintenance in cancer26, 42,43,44,45,46,47,48. In addition, TERT promoter mutations in BCCs were associated with shorter telomere and increased transcription of the telomerase reverse transcriptase subunit13, 26. It is thought that the genome instability caused by critically short telomeres promotes telomerase upregulation, thus sustaining cell proliferation and tumorigenesis49. In the present study, TERT promoter mutations were found in 57.9% of tumours although they were mutually exclusive.
We also identified DPH3 promoter mutations in 49.1% of BCCs, being the -121 C > T and -122 C > T transitions the most frequent ones. Mutations in the DPH3 promoter were previously described in 42% of BCCs.42 In a recent study, 73/191 (38.2%) BCCs were found to carry DPH3 promoter mutations that were significantly more frequent in BCC patients with a clinical history of cutaneous neoplasms24. However, the effect of DPH3 promoter mutations on transcription of adjacent or distant genes remains currently unclear42. The exclusive identification of mutations at dipirimidinic sites into DPH3 and TERT promoter further highlights the role of UV-induced DNA damage in BCC tumorigenesis.
Additional in vivo studies evaluating the function of the novel variants (56%), of which 22.2% with uncertain significance, are needed to clarify their implications in BCC tumours.
In conclusions, our study provides further insights into the molecular alterations underlying the tumorigenic mechanism of superficial and nodular BCCs showing that additional genes and pathways beyond PTCH1-axis might contribute to BCC development and progression.
Material and methods
Patients and tumour samples
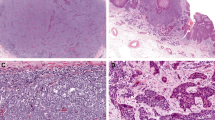
Sporadic BCC tumour tissues and matched blood samples were collected at the Institute of Dermatology, Catholic University—Fondazione Policlinico Universitario A. Gemelli-IRCCS, (Rome, Italy) and at the Dermatologic Clinic of the University of L’Aquila (L’Aquila, Italy) from January 2015 to July 2017 with complete medical records. Examples of superficial and nodular BCC lesion included in our study are reported in Supplementary Fig. S1. Informed consent was obtained from all patients after study approval by the local ethical committee (IRB number:15272/14, Ethical Committee Fondazione Policlinico Universitario A. Gemelli-IRCCS) and the research was performed in accordance with relevant guidelines and regulations stated in the Declaration of Helsinki. Patients and tumours characteristics are illustrated in Table 1. Only superficial and nodular types of BCCs, histologically reviewed by a single histopathologist, were included in the study.
During surgical excision, a 4-mm intra-tumoral punch biopsy specimen was obtained and stored in RNA later solution at -20 °C. DNA was extracted from fresh-frozen tumour samples using Qiagen All Prep-DNA/RNA/miRNA extraction kit (Qiagen, Hilden, Germany) after tissues homogenization in a Precellys24 homogeniser (Bertin instruments, Montigny-le-Bretonneux, France). DNA from whole blood was purified using Qiagen QIAamp Blood Midi Kit (Hilden, Germany) and quantified by Qubit dsDNA HS Assay Kit (ThermoFisher Scientific, Waltham, MA USA) on Qubit 2.0 Fluorometer instrument (Invitrogen, Carlsbad, CA, USA). Genomic DNA at least 10 ng/μL concentrated was subjected to library preparation.
Panel design and library preparation for NGS sequencing
Overall, 12 genes (CSMD1, CSMD2, DPH3 promoter, PTCH1, SMO, GLI1, NOTCH1, NOTCH2, TP53, ITIH2, DPP10, STEAP4) were selected on the basis of a comprehensive literature search and interrogation of different bioinformatics sources like the Catalogue of Somatic Mutations in Cancer (COSMIC) and The Cancer Genome Atlas (TCGA), taking into account the differences in the mutational profile between specific BCC subtypes.The custom gene-panel was designed by using Ion AmpliSeq Designer tool.
Library preparation was performed using the Ion Ampliseq Library kits 2.0 with 20 ng of DNA as input. After clonal amplification on the Ion One Touch2 System and subsequent enrichment on the Ion One Touch ES, libraries were sequenced on the Ion Torrent Ion PGM System (Thermo Fisher Scientific, Waltham, MA USA).
Variant calling analysis
Tumour-germline paired sequencing data were primarily analysed by using IonTorrent Suite Software for base calling and alignment to the hg19 human reference genome from UCSC Genome Browser18. Raw data were then processed for somatic variant calling and annotation by following the VarDict workflow in paired samples (tumour/normal) analysis mode. The allele frequency and mapping quality thresholds were set at 0.05 and 30, respectively. Only the variants recognized as "StrongSomatic" were selected. To reduce the false positive rate during somatic mutation calling, several steps were used in order to retain only the high-quality variants with a minimum depth of total coverage ≥ 300 reads and each variant coverage ≥ 20 reads. Filtered variants were functionally annotated using Annovar software version 2018 Apr 1619.
Prediction tools analysis
All the identified cancer genomics variants were evaluated by using the cBioPortal for Cancer Genomics tool20, which includes the OncoKB precision oncology knowledge database21, 22 for investigation of clinical significance, biological effects and treatment implications of specific cancer gene alterations. For in silico prediction of protein functional effect of variants we referred to the dbNSFP v.4.1 database (database of Human Non-synonymous SNVs and their Functional Predictions), which includes SIFT, PolyPhen2 HDIV, PolyPhen2 HVAR, LRT, MutationTaster, MutationAssessor, FATHMM, GERP++, PhyloP and SiPhy pathogenicity scores. This database is included in the American College of Medical Genetics and Genomics (ACMG) classification provided by Varsome, and in the filter-based annotation provided by Annovar. The potential clinical impact of stop-gain splicing variants, frameshift, and in-frame insertions and deletions was estimated with Mutation Taster. Each variant was then matched with its classification in publicly-available databases and datasets like the NCBI ClinVar database, the Human Genome Mutation Database (HGMD), NCBI dbSNP, Catalogue of Somatic Mutation In Cancer (COSMIC), The Cancer Genome Atlas (TCGA), VarSome and 1000 Genomes Project. Variants not previously published or documented in online variant databases were considered as novel.
Detection of TERT promoter mutations by direct sequencing
Mutational status of TERT promoter (between − 286 and − 27 from ATG start site) was screened by Sanger sequencing. PCR was carried out with the designed primers [forward: 5'CCCACGTGCGCAGCAGGAC 3'; reverse: 5'CTCCCAGTGGATTCGCGGGC 3'] by using the following cycling conditions: denaturation at 95 °C for 45 s, annealing at 60 °C for 30 s, extension at 72 °C for 30 s. The amplified products underwent sequencing analysis on the Applied Biosystems™ 3500 Series Genetic Analyzer instrument (Thermo Fisher, Foster City, USA) and the sequencing data were investigated by using Geneious Pro 5.6.5 software mapping to the hg19 human reference genome from NCBI gene database.
Statistical analysis
The relationship between mutations and clinic-pathological features was evaluated using logistic regression analysis with estimation of OR and 95% CI. Semi-quantitative data were analysed by means with Student’s t test or by medians with Mann–Whitney test. P values < 0.05 were considered statistically significant. Computations were performed using the R v3.6.2 statistical package. Mutual exclusivity analysis was performed by using the cBioPortal for Cancer Genomics tool20 that identify patterns of mutual exclusivity or co-occurrence through a Fisher's exact test21. The PCA (Principal Component Analysis) multivariate analysis was performed in order to identify genetic variations among superficial and nodular BCC subgroups. PCA diagram was generated with the prcomp R function and plotted with ggplot223.
Ethics declarations
The study was approved by the local ethical committee (IRB number: 15272/14, Ethical Committee Fondazione Policlinico Universitario A. Gemelli-IRCCS) and the research was performed in accordance with relevant guidelines and regulations stated in the Declaration of Helsinki. The patients in this manuscript have given written informed consent to publication of their case details.
Data availability
The datasets presented in this study can be found at the online NCBI BioProject repository, https://www.ncbi.nlm.nih.gov/Traces/study/?acc=PRJNA731355, accession PRJNA731355.
References
Leiter, U., Keim, U. & Garbe, C. Epidemiology of skin cancer: Update 2019. Adv. Exp. Med. Biol. 1268, 123–139 (2020).
Lomas, A., Leonardi-Bee, J. & Bath-Hextall, F. A systematic review of worldwide incidence of non-melanoma skin cancer. Br. J. Dermatol. 166, 1069–1080 (2012).
World Health Organization. Global Health Observatory. http://who.int/gho/database/en/; 2018 (last accessed 1 September 2020).
Peris, K. et al. Diagnosis and treatment of basal cell carcinoma: European consensus-based interdisciplinary guidelines. Eur. J. Cancer. 118, 10–34 (2019).
Verkouteren, J. A. C., Ramdas, K. H. R., Wakkee, M. & Nijsten, T. Epidemiology of basal cell carcinoma: Scholarly review. Br. J. Dermatol. 177, 359–372 (2017).
Messina, J. et al. Keratinocytic/epidermal tumours: Basal cell carcinoma. In WHO Classification of Skin Tumours 4th edn (eds Elder, D. E. et al.) 26–34 (IARC, Lyon, 2018).
Scrivener, Y., Grosshans, E. & Cribier, B. Variations of basal cell carcinomas according to gender, age, location and histopathological subtype. Br. J. Dermatol. 147, 41–47 (2002).
Soyer, H. P., Rigel, D. & Wurm, E. M. T. Actinic keratosis, basal cell carcinoma and squamous cell carcinoma. In Dermatology (eds Bolognia, J. L. et al.) 1773–1793 (Saunders, Beijing, 2012).
Cameron, M. C. et al. Basal cell carcinoma epidemiology; pathophysiology; clinical and histological subtypes; and disease associations. J. Am. Acad. Dermatol. 80, 303–317 (2019).
Marzuka, A. G. & Book, S. E. Basal cell carcinoma: Pathogenesis, epidemiology, clinical features, diagnosis, histopathology, and management. Yale J. Biol. Med. 88, 167–179 (2015).
Kuonen, F. et al. Loss of primary cilia drives switching from hedgehog to Ras/MAPK pathway in resistant basal cell carcinoma. J. Invest. Dermatol. 139, 1439–1448 (2019).
Hanna, A. & Shevde, L. A. Hedgehog signaling: Modulation of cancer properties and tumor mircroenvironment. Mol. Cancer. 15, 24 (2016).
Pellegrini, C. et al. Understanding the molecular genetics of basal cell carcinoma. Int. J. Mol. Sci. 18, 2485 (2017).
Bonilla, X. et al. Genomic analysis identifies new drivers and progression pathways in skin basal cell carcinoma. Nat. Genet. 48, 398–406 (2016).
Jayaraman, S. S., Rayhan, D. J., Hazany, S. & Kolodney, M. S. Mutational landscape of basal cell carcinomas by whole-exome sequencing. J. Invest. Dermatol. 134, 213–220 (2014).
Atwood, S. X. et al. Rolling the genetic dice: Neutral and deleterious smoothened mutations in drug-resistant basal cell carcinoma. J. Invest. Dermatol. 135, 2138–2141 (2015).
Sharpe, H. J. et al. Genomic analysis of smoothened inhibitor resistance in basal cell carcinoma. Cancer Cell 27, 327–341 (2015).
Genome Browser University of California Santa Cruz. Genomics Institute. https://genome.ucsc.edu/; (last accessed 1 September 2020).
Yang, H. & Wang, K. Genomic variant annotation and prioritization with ANNOVAR and wANNOVAR. Nat. Protoc. 10, 1556–1566 (2015).
cBioPortal for cancer genomics. https://www.cbioportal.org/; (last accessed 1 September 2020).
Cerami, E. et al. The cBio cancer genomics portal: An open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2, 401–404 (2012).
Gao, J. et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci. Signal. 6, l1 (2013).
Wickham, H., Navarro, D. & Pedersen, T. L. ggplot2: Elegant Graphics for Data Analysis (Springer, New York, 2016).
Baugh, E. H., Ke, H., Levine, A. J., Bonneau, R. A. & Chan, C. S. Why are there hotspot mutations in the TP53 gene in human cancers?. Cell Death Differ. 25, 154–160 (2018).
Goodman, A. M. et al. Genomic landscape of advanced basal cell carcinoma: Implications for precision treatment with targeted and immune therapies. Oncoimmunology 7, e1404217 (2018).
Maturo, M. G. et al. Coding and noncoding somatic mutations in candidate genes in basal cell carcinoma. Sci. Rep. 10, 8005 (2020).
Reinders, M. G. et al. New mutations and an updated database for the patched-1 (PTCH1) gene. Mol. Genet. Genomic Med. 6, 409–15 (2018).
Richards, S. et al. Standards and guidelines for the interpretation of sequence variants: A joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 17, 405–423 (2015).
Wallis, Y.P.S., et al. Practice guidelines for the evaluation of pathogenicity and the reporting of sequence variants in clinical molecular medicine. (Association for Clinical Genetic Science (ACGS), Dutch Society of Clinical Laboratory Specialists (VKGL), 2013).
Wolff, F. et al. Imiquimod directly inhibits Hedgehog signalling by stimulating adenosine receptor/protein kinase A-mediated GLI phosphorylation. Oncogene 32, 5574–5581 (2013).
NIH U.S. National Library of Medicine ClinicalTrials.gov. https://www.clinicaltrials.gov/; (last accessed 1 September 2020).
Hogan, L. E. et al. Integrated genomic analysis of relapsed childhood acute lymphoblastic leukemia reveals therapeutic strategies. Blood 118, 5218–5226 (2011).
Jung, A. R., Eun, Y. G., Lee, Y. C., Noh, J. K. & Kwon, K. H. Clinical significance of cub and sushi multiple domains 1 inactivation in head and neck squamous cell carcinoma. Int. J. Mol. Sci. 19, 3996 (2018).
Kamal, M. et al. Loss of CSMD1 expression is associated with high tumour grade and poor survival in invasive ductal breast carcinoma. Breast Cancer Res. Treat. 121, 555–563 (2010).
Wood, L. D. et al. The genomic landscapes of human breast and colorectal cancers. Science 318, 1108–1113 (2007).
Moore, G., Annett, S., McClements, L. & Robson, T. Top notch targeting strategies in cancer: A detailed overview of recent insights and current perspectives. Cells 9, 1503 (2020).
Chappell, W. H. et al. Increased protein expression of the PTEN tumor suppressor in the presence of constitutively active Notch 1. Cell Cycle 4, 1389–1395 (2005).
Nicolas, M. et al. Notch1 functions as a tumor suppressor in mouse skin. Nat. Genet. 33, 416–421 (2003).
Shi, F.-T. et al. Notch signalling is significantly suppressed in basal cell carcinomas and activation induces basal cell carcinoma cell apoptosis. Mol. Med. Rep. 15, 1441–1454 (2017).
Eberl, M. et al. Tumor architecture and notch signaling modulate drug response in basal cell carcinoma. Cancer Cell 33, 229–243 (2018).
Qi, S. Y., Riviere, P. J., Trojnar, J., Junien, J. L. & Akinsanya, K. O. Cloning and characterization of dipeptidyl peptidase 10, a new member of an emerging subgroup of serine proteases. Biochem. J. 373, 179–189 (2003).
Denisova, E. et al. Frequent DPH3 promoter mutations in skin cancers. Oncotarget 6, 35922–35930 (2015).
Griewank, K. G. et al. TERT promoter mutations are frequent in cutaneous basal cell carcinoma and squamous cell carcinoma. PLoS One 8, e80354 (2013).
Killela, P. J. et al. TERT promoter mutations occur frequently in gliomas and a subset of tumors derived from cells with low rates of self-renewal. Proc. Natl. Acad. Sci. USA 110, 6021–6026 (2013).
Pópulo, H. et al. TERT promoter mutations in skin cancer: The effects of sun exposure and X-irradiation. J Invest Dermatol 134, 2251–2257 (2014).
Rachakonda, P. S. et al. TERT promoter mutations in bladder cancer affect patient survival and disease recurrence through modification by a common polymorphism. Proc. Natl. Acad. Sci. USA 110, 17426–17431 (2013).
Scott, G. A., Laughlin, T. S. & Rothberg, P. G. Mutations of the TERT promoter are common in basal cell carcinoma and squamous cell carcinoma. Mod. Pathol. 27, 516–523 (2014).
Xing, M. et al. BRAF V600E and TERT promoter mutations cooperatively identify the most aggressive papillary thyroid cancer with highest recurrence. J. Clin. Oncol. 32, 2718–2726 (2014).
Chiba, K. et al. Mutations in the promoter of the telomerase gene TERT contribute to tumorigenesis by a two-step mechanism. Science 357, 1416–1420 (2017).
Author information
Authors and Affiliations
Contributions
Prof. K.P., Prof. M.C.F, C.P. and L.D.N. designed the project. L.D.N., C.P. and M.G.M. performed data curation and analysis. S.D.S. performed bioinformatic analysis. P.D. and G.P. performed the statistical analysis. Prof. K.P., L.D.N., C.P. wrote the original draft. A.D.S. performed histopathologic revision of the BCC subtypes. A.D.S., B.F., L.D.R., F.R., T.R. performed case examination, tumour/blood samples collection and supervised clinical data collection. Prof. K.P., Prof. M.C.F., V.C. and Prof. G.T. reviewed and edited the manuscript. All the authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
Dr. K. Peris reports grants and personal fees from Abbvie, personal fees from Almirall, personal fees from Lilly, grants and personal fees from Galderma, personal fees from Leo Pharma, personal fees from Novartis, personal fees from Pierre Fabre, from Sanofi, personal fees from Sun Pharma, personal fees from Janssen, outside the submitted work. Dr. L. Di Nardo, C. Pellegrini, A. Di Stefani, F. Ricci, B. Fossati, L. Del Regno, C. Carbone, G. Piro, V. Corbo, P. Delfino, S. De Summa, M.G. Maturo, T. Rocco, G. Tortora, M.C. Fargnoli report none conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Di Nardo, L., Pellegrini, C., Di Stefani, A. et al. Molecular alterations in basal cell carcinoma subtypes. Sci Rep 11, 13206 (2021). https://doi.org/10.1038/s41598-021-92592-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-92592-3
This article is cited by
-
Histopathological Pattern of Head and Neck Recurrent BCC After Previous Cryotherapy
Indian Journal of Otolaryngology and Head & Neck Surgery (2023)
-
Basal cell carcinoma of the scalp shows distinct features from the face in Asians
Scientific Reports (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.