Abstract
Background
Acute biliary pancreatitis (ABP) is often associated with persistent common bile duct (CBD) stones. The best strategy in terms of timing of surgery is still controversial. The aim of the current study is to describe the prevalence of persistent common bile duct (CBD) stones in ABP during the first week of symptoms at a high-volume referral center.
Study Design
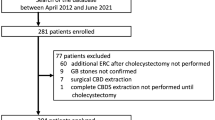
Single-institution retrospective analysis of a prospectively collected database. Patients with diagnosis of ABP who underwent laparoscopic cholecystectomy (LC) between January 2009 and December 2019 were extracted.
Results
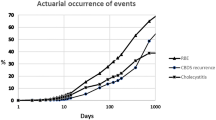
Two hundred thirty-one patients were included. Cholecystectomy was performed laparoscopically in 230 (99.57%) patients. Intraoperative cholangiogram was performed in all patients. Two hundred nine (90%) patients had surgery within the first 7 days. Global prevalence of persistent CBD stones during IOC was 19.91% (95% CI 14.96–25.65). No significant association between timing to surgery and presence of CBD stones was found for the first week since the initial attack (p=0.28). Prevalence of CBD stones was significantly higher after day 7 (p=0.007 and 0.005). Positive findings in preoperative MRCP are significantly related to intraoperative CBD stones (p=0.0001). Mild postoperative complications (CD I/II) were present in 21 patients (9.09%). No difference was found in morbidity between CBD stones group and non-CBD stones group (p=0.48). We observed no severe complications nor mortality.
Conclusions
In patients with mild acute biliary pancreatitis, the prevalence of persistent CBD stones does not change within the first 7 days since the onset of symptoms. This fact may have major clinical relevance when deciding the optimal therapeutic strategy in this population.



Similar content being viewed by others
References
Moody N, Adiamah A, Yanni F, Gomez D. Meta-analysis of randomized clinical trials of early versus delayed cholecystectomy for mild gallstone pancreatitis. Br J Surg 2019;106(11):1442–1451
Colvin SD, Smith EN, Morgan DE, Porter KK. Acute pancreatitis: an update on the revised Atlanta classification. Abdom Radiol 2020;45, 1222–1231
Acosta JM, Ledesma CL. Gallstone migration as a cause of acute pancreatitis. N Engl J Med 1974; 290(9):484–487
Oria A, Alvarez J, Chiappetta L, Spina JC, Hernandez N, Iovaldi M et al. Choledocholithiasis in Acute Gallstone Pancreatitis. Incidence and Clinical Significance. Arch Surg. 1991; Vol 126. pag 566-568
Kelly TR. Gallstone pancreatitis: pathophysiology. Surgery. 1976;80:488-492.
H. Shayan, D Kopac, B Sample. The role of intraoperative cholangiogram in the management of patients recovering from acute biliary pancreatitis. Surg endosc 2007; 21: 1549–1552
Schwesinger WH, Page CP, Sirinek KR, Levine BA, Aust JB. Biliary pancreatitis: operative outcome with a selective approach. Arch Surg 1991; 126: 836–839
Stone HH, Fabian TC, Dunlop WE. Gallstone pancreatitis. Biliary tract pathology in relation to time of operation. Ann Surg 1981;194:305–312.
Liu CL, Lo CM, Fan ST. Acute biliary pancreatitis: diagnosis and management. World J Surg 1997;21:149–154.
Neoptolemos J, Ogunbiyi OA, Wilson P, Carr-Locke DL. Etiology, pathogenesis, natural history and treatment of biliary acute pancreatitis. In Beger HG, Warshaw AL, Büchler MW, Carr-Locke DL, Neoptolemos JP, Russell Ch, Sarr M, eds. The Pancreas, 1st ed. Oxford: Blackwell, 1998, pp 521–547.
Yeung YP, Lo SF, Yip AW. Role of ERCP in the management of predicted mild acute biliary pancreatitis. Asian J Surg 2003;26:197–201.
Barro J, Soetikno RM, Carr-Locke DL. Early endoscopic sphincterotomy in acute pancreatitis: is it indicated, advisable, not indicated, or contraindicated? A proposal for clinical practice. In Dominguez-Numoz JE, ed.Clinical Pancreaotology for practising Gastroenterologists and Surgeons. 1st ed. Oxford: Blackwell, 2005; 113-24.
Unsup Kim, MD, Han-Yu Shen, MD, Bruce Bodner, Timing of Surgery for Acute Gallstone PanCreatitis. Am. J. Surg 1988; 156:393-396
Antonio Navarro-Sánchez. Single-stage laparoscopic management of acute gallstone pancreatitis: outcomes at different timings. Hepatobiliary Pancreat Dis Int June 15,2016; Vol 15,No 3.
Aranovich, D, Zilbermints, V, Goldberg, N, Kaminsky, O. Detection of Common Bile Duct Stones in Mild Acute Biliary Pancreatitis Using Magnetic Resonance Cholangiopancreatography. Surgery research and practice, 2018; 5216089.
Schachter P, Peleg T, Cohen O. Interval laparoscopic cholecystectomy in the management of acute biliary pancreatitis. HPB Surg 2000;11:319-323.
Kullman E, Borch K, Lindstrom , Svanvik J, Anderberg B. Management of bile ducts stones in the era of laparoscopic cholecystectomy: appraisal of routine operative cholangiography and endoscopic treatment. Eur J Surg 1996;162: 873–880
Ricci MDF, Castaldini MDG, De Manzoni MDG, Borzellino G, Rodella L, Kind R, Cordiano C. Treatment of gallstone pancreatitis: six-year experience in a single center. World J Surg 2002;26: 85–90
Metcalfe MS, Ong T, Bruening MH, Iswariah H, Wemyss-Holden SA, Maddern GJ. Is laparoscopic intraoperative cholangiogram a matter of routine? Am J Surg 2004;187: 475–481
Uhl W, Muller CA, Krahenbuhl L, Schmid SW, Scholzel S, Buchler MW. Acute gallstone pancreatitis: timing of laparoscopic cholecystectomy in mild and severe disease. Surg Endosc 1999;13: 1070–1076
Giuffrida P, Biagiola D, Cristiano A, Ardiles V, de Santibañes M, Sanchez Claria R, Pekolj J, de Santibañes E, Mazza O. Laparoscopic cholecystectomy in acute mild gallstone pancreatitis: how early is safe? Updates in Surgery 2020; 72:129–135
Aboulian A, Chan T, Yaghoubian A, Kaji AH, Putnam B, Neville A et al. Early cholecystectomy safely decreases hospital stay in patients with mild gallstone pancreatitis: a randomized prospective study. Ann Surg 2010;251(4):615–619
Mueck KM, Wei S, Pedroza C, Bernardi K, Jackson ML, Liang MK, Ko TC, Tyson JE, Kao LS. Gallstone Pancreatitis: Admission Versus Normal Cholecystectomy-a Randomized Trial (Gallstone PANC Trial). Ann Surg. 2019 Sep;270(3):519-527. doi: https://doi.org/10.1097/SLA.0000000000003424.
Baillie J. AGA institute medical position statement on acute pancreatitis. Gastroenterology 2007;132(5):2019–2022
Uhl W, Warshaw A, Imrie C, Bassi C, McKay CJ, Lankisch PG et al. IAP guidelines for the surgical management of acute pancreatitis. Pancreatology 2002;2(6):565–573
Zhong FP, Wang K, Tan XQ, Nie J, Huang WF, Wang XF. The optimal timing of laparoscopic cholecystectomy in patients with mild gallstone pancreatitis: A meta-analysis. Medicine (Baltimore). 2019;98(40):e17429
Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, Tsiotos GG, Vege SS, Group APCW. Classification of acute pancreatitis–2012: revision of the Atlanta classification and definitions by international consensus. Gut 2013;62 (1):102-111.
Balthazar EJ. Acute pancreatitis: assessment of severity with clinical and CT evaluation. Radiology 2002;223(3):603-613.
Pekolj J, Alvarez FA, Palavecino M, Sánchez Clariá R, Mazza O, de Santibañes E. Intraoperative management and repair of bile duct injuries sustained during 10,123 laparoscopic cholecystectomies in a high-volume referral center. J Am Coll Surg. 2013 May;216(5):894-901.
F. A. Alvarez, M. de Santibañes, M. Palavecino, R. Sanchez Claria, O. Mazza, G. Arbues et al. Impact of routine intraoperative cholangiography during laparoscopic cholecystectomy on bile duct injury. BJS 2014; 101: 677–684.
Clavien PA, Barkun J, De Oliveira ML, Vauthey JN, Dindo D, Schulick RD et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 2009;250(2):187–196
Dindo D. The Clavien-Dindo classification of surgical complications. In: Cuesta M, Jaap Bonjer H (eds) Treatment of postoperative complications after digestive surgery. Springer, London, 2014;pp 13–17.
Nikhil Panda. Gallstone Pancreatitis and Choledocholithiasis: Using Imaging and Laboratory Trends to Predict the Likelihood of Persistent Stones at Cholangiography. World J Surg 2018; 42:3143–3149
Bertolín-Bernades R, Mild Acute Biliary Pancreatitis vs Cholelithiasis: Are There Differences in the Rate of Choledocholithiasis? J Gastrointest Surg 2007; 11:875–879
Tang E, Stain SC, Tang G, Froes E, Berne TJ. Timing of laparoscopic surgery in gallstone pancreatitis. Arch Surg 1995;130: 496–500
Frossard JL, Hadengue A, Amouyal G, Choury A, Marty O,Giostra E, et al. Choledocholihiasis: a prospective study of spontaneous common bile duct stone migration. Gastrointest Endosc 2000;51:175–179.
Tranter SE, Thompson MH. Spontaneous passage of bile duct stones: frequency of occurrence and relation to clinical presentation. Ann R Coll Surg Engl 2003;85:174–177.
Sherman JL et al. Validation and improvement of a proposed scoring system to detect retained common bile duct stones in gallstone pancreatitis. Surgery 2015; 157(6):1073–1079
Barkun AN et al.Useful predictors of bile duct stones in patients undergoing laparoscopic cholecystectomy. McGill gallstone treatment group. Ann Surg 1994;220(1):32–39
Cohen ME et al.Prediction of bile duct stones and complications in gallstone pancreatitis using early laboratory trends. Am J Gastroenterol 2001; 96(12):3305–3311
Freitas ML, Bell RL, Duffy AJ.Choledocholithiasis: evolving standards for diagnosis and management. World J Gastroenterol 2006; 12(20):3162–3167
Cronan JJ. US diagnosis of choledocholithiasis: a reappraisal. Radiology 1986;161(1):133–134
Peng WK et al. Role of liver function tests in predicting common bile duct stones in acute calculous cholecystitis. Br J Surg 2005;92(10):1241–1247
Gurusamy KS, Nagendran M, Davidson BR. Early versus delayed laparoscopic cholecystectomy for acute gallstone pancreatitis. Cochrane Database Syst Rev 2013;9:CD010326.
Fölsch UR, Nitsche R, Lüdtke R, Hilgers RA, Creutzfeldt W. Early ERCP and papillotomy compared with conservative treatment for acute biliary pancreatitis. The German Study Group on Acute Biliary Pancreatitis. N Engl J Med 1997;336:237-242.
Kochar B, Akshintala VS, Afghani E, et al. Incidence, severity, and mortality of post-ERCP pancreatitis: a systematic review by using randomized, controlled trials. Gastroint Endosc 2015;81:143
Bilal M, Kline KT, Trieu JA, Saraireh H, Desai M, Parupudi S, Abougergi, MS. Trends in same-admission cholecystectomy and endoscopic retrograde cholangiopancreatography for acute gallstone pancreatitis: A nationwide analysis across a decade.Pancreatology 2019;19(4), 524–530.
Czerwonko ME, Pekolj J, Uad P, Mazza O, Sanchez-Claria R, Arbues G, de Santibañes E, de Santibañes M, Palavecino M. Laparoscopic Transcystic Common Bile Duct Exploration in the Emergency Is as Effective and Safe as in Elective Setting. J Gastrointest Surg. 2019 Sep;23(9):1848-1855. doi: https://doi.org/10.1007/s11605-018-4029-x.
Author information
Authors and Affiliations
Contributions
Study conception and design: Fratantoni ME, de Santibañes M, and Mazza O
Acquisition of data: Fratantoni ME, Giuffrida P, and Di Menno J
Analysis and interpretation of data: Fratantoni ME, Giuffrida P, Di Menno J, Ardiles V, de Santibañes M, Sanchez Claria R, Palavecino M, de Santibañes E, Pekolj J, and Mazza O
Drafting of manuscript: Fratantoni ME, Giuffrida P, Di Menno J, Ardiles V, de Santibañes M, Sanchez Claria R, Palavecino M, de Santibañes E, Pekolj J, and Mazza O
Critical revision: Fratantoni ME, Giuffrida P, Di Menno J, Ardiles V, de Santibañes M, Sanchez Claria R, Palavecino M, de Santibañes E, Pekolj J, and Mazza O
Corresponding author
Ethics declarations
Ethical Considerations
The study was carried out in full agreement with current National and International regulations: Declaration of Helsinki of the World Medical Association and the Standards of Good Clinical Practices ICH E6. The protocol was approved by the Institutional Review Board (IRB) with number 5381, and all study data was treated with maximum confidentiality anonymously and with restricted access only for authorized personnel for the purposes of the study.
Research Involving Human Participants and/or Animals
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
For this type of study, formal consent is not required.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fratantoni, M.E., Giuffrida, P., Di Menno, J. et al. Prevalence of Persistent Common Bile Duct Stones in Acute Biliary Pancreatitis Remains Stable Within the First Week of Symptoms. J Gastrointest Surg 25, 3178–3187 (2021). https://doi.org/10.1007/s11605-021-05068-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-021-05068-0