Abstract
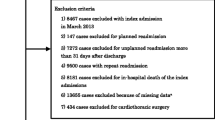
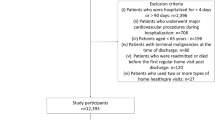
The relationship between the socioeconomic status, including the health insurance status, and prognosis of heart failure (HF) has been recognized as an important concept for stratifying the risk in HF patients and is gaining increasing attention worldwide even in countries with a universal healthcare system. However, the impact of the Japanese health insurance status on outcomes among patients admitted for acute HF has not been fully clarified. We enrolled 771 patients admitted for acute HF between January 2018 and December 2019 and collected data on the in-hospital mortality, length of the hospital stay, and cardiac events, defined as cardiovascular death and readmission for HF within 1 year after discharge. Patients were divided into two groups according to their insurance status, i.e., public assistance (n = 87) vs. other insurance (n = 684). The public assistance group was significantly younger and had a higher rate of diabetes, smoking, ischemic and hypertensive heart disease, and low estimated glomerular filtration rate (all P < 0.05). Pharmacological/invasive heart failure therapy, in-hospital mortality, and the 90-day cardiac event rate after discharge did not differ between the groups. However, the public assistance group had a significantly higher 1-year cardiac event rate than the other insurance groups (P = 0.025). After adjusting for covariates, public assistance was independently associated with the 1-year cardiac event rate (HR: 2.15, 95% CI: 1.42–3.26, P < 0.001). Acute HF patients covered by public assistance received the same quality of medical care, including invasive therapy. As a result, no health disparities were found in terms of the in-hospital mortality and 90-day cardiac event rate, unlike overseas surveys. Nevertheless, HF patients with public assistance had a higher risk for the long-term prognosis than those with other insurance. Comprehensive HF management is required post-discharge.

Similar content being viewed by others
References
Schultz WM, Kelli HM, Lisko JC, Varghese T, Shen J, Sandesara P, Quyyumi AA, Taylor HA, Gulati M, Harold JG, Mieres JH, Ferdinand KC, Mensah GA, Sperling LS (2018) Socioeconomic status and cardiovascular outcomes: challenges and interventions. Circulation 137(20):2166–2178
Verma AK, Schulte PJ, Bittner V, Keteyian SJ, Fleg JL, Piña IL, Swank AM, Fitz-Gerald M, Ellis SJ, Kraus WE, Whellan DJ, O’Connor CM, Mentz RJ (2017) Socioeconomic and partner status in chronic heart failure: relationship to exercise capacity, quality of life, and clinical outcomes. Am Heart J 183:54–61
Philbin EF, Dec GW, Jenkins PL, DiSalvo TG (2001) Socioeconomic status as an independent risk factor for hospital readmission for heart failure. Am J Cardiol 87(12):1367–1371
Tromp J, Bamadhaj S, Cleland JGF, Angermann CE, Dahlstrom U, Ouwerkerk W, Tay WT, Dickstein K, Ertl G, Hassanein M, Perrone SV, Ghadanfar M, Schweizer A, Obergfell A, Lam CSP, Filippatos G, Collins SP (2020) Post-discharge prognosis of patients admitted to hospital for heart failure by world region, and national level of income and income disparity (REPORT-HF): a cohort study. Lancet Glob Health 8(3):e411–e422
Schjødt I, Johnsen SP, Strömberg A, Kristensen NR, Løgstrup BB (2019) Socioeconomic factors and clinical outcomes among patients with heart failure in a universal health care system. JACC Heart Fail 7(9):746–755
Sulo G, Igland J, Øverland S, Sulo E, Kinge JM, Roth GA, Tell GS (2020) Socioeconomic gradients in mortality following HF hospitalization in a country with universal health care coverage. JACC Heart Fail 8(11):917–927
Danchin N, Neumann A, Tuppin P, De Peretti C, Weill A, Ricordeau P, Allemand H (2011) Impact of free universal medical coverage on medical care and outcomes in low-income patients hospitalized for acute myocardial infarction: an analysis from the FrenchNational Health Insurance system. Circ Cardiovasc Qual Outcomes 4(6):619–625
Watanabe S, Usui M (2020) Clinical features of ST-segment elevation myocardial infarction in patients receiving welfare public assistance in urban area of Japan. J Cardiol 77(4):404–407
Dickman SL, Himmelstein DU, Woolhandler S (2017) Inequality and the health-care system in the USA. Lancet 389(10077):1431–1441
Foraker RE, Rose KM, Suchindran CM, Chang PP, McNeill AM, Rosamond WD (2011) Socioeconomic status, Medicaid coverage, clinical comorbidity, and rehospitalization or death after an incident heart failure hospitalization: Atherosclerosis Risk in Communities cohort (1987 to 2004). Circ Heart Fail 4(3):308–316
Ikegami N, Yoo BK, Hashimoto H, Matsumoto M, Ogata H, Babazono A, Watanabe R, Shibuya K, Yang BM, Reich MR, Kobayashi Y (2011) Japanese universal health coverage: evolution, achievements, and challenges. Lancet 378(9796):1106–1115
Fujiwara Y, Yonemori K, Shibata T, Okita N, Ushirozawa N (2015) Japanese universal health care faces a crisis in cancer treatment. Lancet Oncol 16(3):251–252
Takenaka Y, Yasui T, Enomoto K, Miyabe H, Morizane N, Ashida N, Shimizu K, Hirose M, Yamamoto Y, Uno A (2016) Health insurance status and survival among patients with head and neck cancer in Japan. Int J Clin Oncol 21(3):517–522
McKee PA, Castelli WP, McNamara PM, Kannel WB (1971) The natural history of congestive heart failure: the Framingham study. N Engl J Med 285(26):1441–1446
Lu MLR, Davila CD, Shah M, Wheeler DS, Ziccardi MR, Banerji S, Figueredo VM (2016) Marital status and living condition as predictors of mortality and readmissions among African Americans with heart failure. Int J Cardiol 222:313–318
Curtis LH, Greiner MA, Hammill BG, Kramer JM, Whellan DJ, Schulman KA, Hernandez AF (2008) Early and long-term outcomes of heart failure in elderly persons, 2001–2005. Arch Intern Med 168(22):2481–2488
Eapen ZJ, McCoy LA, Fonarow GC, Yancy CW, Miranda ML, Peterson ED, Califf RM, Hernandez AF (2015) Utility of socioeconomic status in predicting 30-day outcomes after heart failure hospitalization. Circ Heart Fail 8(3):473–480
Hung CL, Chao TF, Su CH, Liao JN, Sung KT, Yeh HI, Chiang CE (2021) Income level and outcomes in patients with heart failure with universal health coverage. Heart 107(3):208–216
Dewan P, Rørth R, Jhund PS, Ferreira JP, Zannad F, Shen L, Køber L, Abraham WT, Desai AS, Dickstein K, Packer M, Rouleau JL, Solomon SD, Swedberg K, Zile MR, McMurray JJV, PARADIGM-HF and ATMOSPHERE Investigators (2019) Income inequality and outcomes in heart failure: a global between-country analysis. JACC Heart Fail 7(4):336–346
Hlatky MA, Hamad R (2019) Disentangling the effects of socioeconomic factors on outcomes among patients with heart failure. JACC Heart Fail 7(9):756–758
Cainzos-Achirica M, Capdevila C, Vela E, Cleries M, Bilal U, Garcia-Altes A, Enjuanes C, Garay A, Yun S, Farre N, Corbella X, Comin-Colet J (2019) Individual income, mortality and healthcare resource use in patients with chronic heart failure living in a universal healthcare system: a population-based study in Catalonia, Spain. Int J Cardiol 277:250–257
Rørth R, Fosbøl EL, Mogensen UM, Kragholm K, Numé AK, Gislason GH, Jhund PS, Petrie MC, McMurray JJV, Torp-Pedersen C, Køber L, Kristensen SL (2018) Employment status at time of first hospitalization for heart failure is associated with a higher risk of death and rehospitalization for heart failure. Eur J Heart Fail 20(2):240–247
Otani A, Sakakura K, Yamamoto K, Taniguchi Y, Ito M, Ibe T, Wada H, Momomura SI, Fujita H (2019) Comparison of mid-term clinical outcomes after acute myocardial infarction in diabetic men between living alone and living together. Heart Vessels 34(8):1288–1296
Jaarsma T (2005) Inter-professional team approach to patients with heart failure. Heart 91(6):832–838
Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, de Ferranti SD, Floyd J, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Mackey RH, Matsushita K, Mozaffarian D, Mussolino ME, Nasir K, Neumar RW, Palaniappan L, Pandey DK, Thiagarajan RR, Reeves MJ, Ritchey M, Rodriguez CJ, Roth GA, Rosamond WD, Sasson C, Towfighi A, Tsao CW, Turner MB, Virani SS, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P (2017) Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation 135(10):e146–e603
Yasui H, Michihata N, Matsui H, Fushimi K, Iwase S, Yoshiuchi K, Sakata Y, Yasunaga H (2021) Association between ambulance use and hospitalization costs among heart failure patients. Heart Vessels 36(5):654–658
Acknowledgements
The authors sincerely thank all physicians and medical staff of the Division of Cardiology at Nihon University Itabashi Hospital.
Funding
This research received no grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
D.K. has received research funding from Daiichi-Sankyo. Y.O. has received lecture fees from Bayer Yakuhin and Daiichi-Sankyo; research funding from Bayer Yakuhin and Bristol-Myers Squibb; and scholarship grants from Bayer Yakuhin, Daiichi-Sankyo, and Johnson & Johnson.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fujito, H., Kitano, D., Saito, Y. et al. Association between the health insurance status and clinical outcomes among patients with acute heart failure in Japan. Heart Vessels 37, 83–90 (2022). https://doi.org/10.1007/s00380-021-01895-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-021-01895-y