Abstract
Longitudinal analyses of patient response time courses following doses of therapeutics are currently performed using pharmacokinetic/pharmacodynamic (PK/PD) methodologies, which require considerable human experience and expertise in the modelling of dynamical systems. By utilizing recent advancements in deep learning, we show that the governing differential equations can be learned directly from longitudinal patient data. In particular, we propose a novel neural-PK/PD framework that combines key pharmacological principles with neural ordinary differential equations. We applied it to an analysis of drug concentration and platelet response from a clinical dataset consisting of over 600 patients. We show that the neural-PK/PD model improves on a state-of-the-art model with respect to metrics for temporal prediction. Furthermore, by incorporating key PK/PD concepts into its architecture, the model can generalize and enable the simulations of patient responses to untested dosing regimens. These results demonstrate the potential of neural-PK/PD for automated predictive analytics of patient response time course.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
Source data are provided with this paper. Additional data that support the findings of this study are available from the corresponding author on reasonable request with the approval of Genentech. The raw data that underlies the findings of this study are not publicly available due to reasonable patient privacy concerns.
Code availability
The Wolfram Mathematica code for the neural-PK/PD model is available as Supplementary Software. It can be opened with the Wolfram Player Version 12.1.0 and above, which is freely downloadable from the link https://www.wolfram.com/player/.
References
Meibohm, B. & Derendorf, H. Basic concepts of pharmacokinetic/pharmacodynamic (PK/PD) modelling. Int. J. Clin. Pharmacol. Ther. 35, 401–413 (1997).
Upton, R. N. & Mould, D. R. Basic concepts in population modeling, simulation, and model‐based drug development: part 3—introduction to pharmacodynamic modeling methods. CPT Pharmacometrics Syst. Pharmacol. 3, 1–16 (2014).
Sheiner, L. B. & Ludden, T. M. Population pharmacokinetics/dynamics. Annu. Rev. Pharmacol. Toxicol. 32, 185–209 (1992).
Bonate, P. L. Pharmacokinetic–Pharmacodynamic Modeling and Simulation 20 (Springer, 2011).
Owen, J. S. & Fiedler-Kelly, J. Introduction to Population Pharmacokinetic/Pharmacodynamic Analysis with Nonlinear Mixed Effects Models (John Wiley & Sons, 2014).
Keizer, R. J. et al. Model‐informed precision dosing at the bedside: scientific challenges and opportunities. CPT Pharmacometrics Syst. Pharmacol. 7, 785–787 (2018).
Chen, R. T., Rubanova, Y., Bettencourt, J. & Duvenaud, D. K. Neural ordinary differential equations. In Advances in Neural Information Processing Systems 31 6571–6583 (NeurIPS, 2018)..
Alber, M. et al. Integrating machine learning and multiscale modeling—perspectives, challenges, and opportunities in the biological, biomedical, and behavioral sciences. NPJ Digit. Med. 2, 1–11 (2019).
Rackauckas, C. et al. Universal differential equations for scientific machine learning. Preprint at https://arxiv.org/abs/2001.04385 (2020).
Rubanova, Y., Chen, R. T. & Duvenaud, D. K., 2019. Latent ordinary differential equations for irregularly-sampled time series. In Advances in Neural Information Processing Systems 32 5320–5330 (NeurIPS, 2019).
Paoletti, M. E., Haut, J. M., Plaza, J. & Plaza, A. Neural ordinary differential equations for hyperspectral image classification. IEEE Trans. Geosci. Remote Sens. 58, 1718–1734 (2019).
Long, Z., Lu, Y. & Dong, B. PDE-Net 2.0: learning PDEs from data with a numeric-symbolic hybrid deep network. J. Comput. Phys. 399, 108925 (2019).
Qin, T., Wu, K. & Xiu, D. Data driven governing equations approximation using deep neural networks. J. Comput. Phys. 395, 620–635 (2019).
Zhang, T. et al. ANODEV2: a coupled neural ODE framework. In Advances in Neural Information Processing Systems 32 5151–5161 (NeurIPS, 2019).
De Brouwer, E., Simm, J., Arany, A. & Moreau, Y. GRU-ODE-Bayes: continuous modeling of sporadically-observed time series. In Advances in Neural Information Processing Systems 33 7379–7390 (NeurIPS, 2019).
Kidger, P., Morrill, J., Foster, J. & Lyons, T. Neural controlled differential equations for irregular time series. In Advances in Neural Information Processing Systems (NeurIPS, 2020).
Bender, C. B et al. An integrated PKPD model of trastuzumab emtansine (T-DM1)–induced thrombocytopenia and hepatotoxicity in patients with HER2–positive metastatic breast cancer. Preprint at https://www.page-meeting.org/pdf_assets/6110-PAGE%202016_bbender_FINAL.pdf (2020).
Bender, C. B. Pharmacometric Models for Antibody Drug Conjugates and Taxanes in HER2+ and HER2– Breast Cancer. Doctoral Dissertation, Acta Universitatis Upsaliensis (2016).
Friberg, L. E., Henningsson, A., Maas, H., Nguyen, L. & Karlsson, M. O. Model of chemotherapy-induced myelosuppression with parameter consistency across drugs. J. Clin. Oncol. 20, 4713–4721 (2002).
Zhang, L., Beal, S. L. & Sheiner, L. B. Simultaneous vs. sequential analysis for population PK/PD data I: best-case performance. J. Pharmacokinet. Pharmacodyn. 30, 387–404 (2003).
Lu, D. et al. Population pharmacokinetics of trastuzumab emtansine (T-DM1), a HER2-targeted antibody–drug conjugate, in patients with HER2-positive metastatic breast cancer: clinical implications of the effect of covariates. Cancer Chemother. Pharmacol. 74, 399–410 (2014).
Chen, S. C. et al. Population pharmacokinetics and exposure–response of trastuzumab emtansine in advanced breast cancer previously treated with ≥2 HER2‐targeted regimens. Br. J. Clin. Pharmacol. 83, 2767–2777 (2017).
Fogel, A. L. & Kvedar, J. C. Artificial intelligence powers digital medicine. NPJ Digit. Med. 1, 1–4 (2018).
Kelly, C. J., Karthikesalingam, A., Suleyman, M., Corrado, G. & King, D. Key challenges for delivering clinical impact with artificial intelligence. BMC Med. 17, 195 (2019).
Nagendran, M. et al. Artificial intelligence versus clinicians: systematic review of design, reporting standards, and claims of deep learning studies. BMJ 368, m689 (2020).
Chen, H., Engkvist, O., Wang, Y., Olivecrona, M. & Blaschke, T. The rise of deep learning in drug discovery. Drug Discovery Today 23, 1241–1250 (2018).
Koch, G. et al. Pharmacometrics and machine learning partner to advance clinical data analysis. Clin. Pharmacol. Ther. 107, 926–933 (2020).
Corrigan, B. W. Artificial intelligence and machine learning: will clinical pharmacologists be needed in the next decade? The John Henry question. Clin. Pharmacol. Ther. 107, 697–699 (2020).
James, G., Witten, D., Hastie, T. & Tibshirani, R. An Introduction to Statistical Learning 112 (Springer, 2013).
Géron, A. Hands-on Machine Learning with Scikit-Learn, Keras, and TensorFlow: Concepts, Tools, and Techniques to Build Intelligent Systems (O’Reilly Media, 2019).
Cho, K. et al. Learning phrase representations using RNN encoder–decoder for statistical machine translation. Preprint at https://arxiv.org/abs/1406.1078078 (2014).
Iserles, A. A First Course in the Numerical Analysis of Differential Equations (Cambridge Univ. Press, 2009).
Goodfellow, I., Bengio, Y. & Courville, A. Deep Learning (MIT Press, 2016).
Mathematica v.12.1 (Wolfram Research, 2020); https://www.wolfram.com/mathematica
Beal, S. L., Sheiner, L. B., Boeckmann, A. J. & Bauer, R. J. NONMEM 7.4.3 Users Guides (1989 –2018) (ICON Development Solutions, 2018).
Schuster, M. & Paliwal, K. K. Bidirectional recurrent neural networks. IEEE Trans. Signal Process. 45, 2673–2681 (1997).
Klambauer, G., Unterthiner, T., Mayr, A. & Hochreiter, S. Self-normalizing neural networks. In Advances in Neural Information Processing Systems Vol. 30, 971–980 (NIPS, 2017).
Acknowledgements
We would like to thank D. Lu, L. Brooks, G. Liu, K. Liu, K. Deng and A. Joshi for their discussions and helping to make this work possible.
Author information
Authors and Affiliations
Contributions
J.L. conceived the study. J.L. and J.Y.J. designed the study. J.L., B.B., J.Y.J. and Y.G. performed data analysis. J.L., B.B., J.Y.J. and Y.G. wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
J.L., B.B., J.Y.J. are employees of Genentech and own stock in Roche. The work was performed when Y.G. served as a consultant to Genentech. The remaining authors declare no competing interests.
Additional information
Peer review information Nature Machine Intelligence thanks Jorrit Enserink, Jing Tang and Giovanni Di Veroli for their contribution to the peer review of this work.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
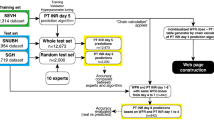
Extended Data Fig. 1 Supplementary Figure 1.
a, The neural-PK schematic diagram. b, Detailed views into the ‘PKODE’ sub-module, which shows an implementation of the forward Euler step that explicitly incorporates the dosing data via the network port ‘Dose’. The network shown in (b) is a recurrent network, which unfolds in time whereby successive ‘NewPKState’ is fed into ‘PrevPK’. The ‘Δt*’ is a layer that multiplies the output of ‘PKVF’ by the constant step size ∆t. The numbers in grey denote the dimension of the arrays involved in the computational graph.
Supplementary information
Supplementary Software
A ZIP file containing a README, and a Mathematica notebook containing model code.
Source data
Source Data Fig. 2
Pharmacokinetic data versus time.
Source Data Fig. 3
Pharmacodynamic (platelet) data versus time.
Source Data Fig. 4
Predicted platelet count from pop-PK/PD and neural-PK/PD models versus data.
Source Data Fig. 5
Platelet count data for Q3W patients.
Rights and permissions
About this article
Cite this article
Lu, J., Bender, B., Jin, J.Y. et al. Deep learning prediction of patient response time course from early data via neural-pharmacokinetic/pharmacodynamic modelling. Nat Mach Intell 3, 696–704 (2021). https://doi.org/10.1038/s42256-021-00357-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s42256-021-00357-4
This article is cited by
-
Low-dimensional neural ODEs and their application in pharmacokinetics
Journal of Pharmacokinetics and Pharmacodynamics (2024)
-
Explainable deep learning for tumor dynamic modeling and overall survival prediction using Neural-ODE
npj Systems Biology and Applications (2023)
-
Towards adequate and automated antibiotic dosing
Intensive Care Medicine (2023)