Abstract
Two hot spot mutations (C228T, C250T) in the telomerase reverse transcriptase (TERT) gene are frequently identified in glioblastoma and oligodendroglioma. TERT mutations predicts an aggressive clinical course in isocitrate dehydrogenase (IDH) wild-type astrocytic tumors. Therefore, it is important to accurately detect TERT promoter mutations in glioma. Sanger DNA sequencing is the currently standard method for analyzing TERT mutations. However, PCR amplification in the first step of the sequencing has proven technically difficult because of the high GC content around the TERT mutation. In this report, we described a novel droplet digital PCR (ddPCR) assay to evaluate TERT hot spot mutations in fresh frozen and formalin-fixed paraffin-embedded (FFPE) specimens of glioma and verified the difference in results from the Sanger DNA sequencing results. We obtained the mutant allele fraction for TERT mutations of in a single ddPCR run in all cases, including the micro-dissected FFPE sections. On the contrary, up to twice the DNA sequences were required from fresh frozen tissue to obtain the results, consistent with ddPCR assay. When FFPE specimens were used, more time was required to evaluate TERT mutations through DNA sequencing. DdPCR is an effective and sensitive assay compared to the conventional standard Sanger DNA sequencing.
Similar content being viewed by others
Introduction
Gliomas are the common malignancies among primary brain tumors, and genetic abnormalities related to their development and progression have been studied [1]. Two-point mutations in the promoter region of the telomerase reverse transcriptase (TERT) gene have been identified at high frequencies in adult gliomas [2, 3]. Most commonly, TERT mutations of C228T or C250T increases the TERT promoter activity by generating binding sites for an activating E26 transformation-specific (ETS) transcription factor in the TERT promoter region [4,5,6]. TERT upregulation leads to telomerase activation, and maintains telomere lengthening, which is a critical step in tumorigenesis [4, 7]. The above-mentioned mutations are frequently found in adult glioblastomas (70–84%) and pure oligodendrogliomas (74%) [2, 8]. This indicates that the presence of TERT hot spot mutations is a useful diagnostic biomarker of glioblastoma and oligodendroglioma.
In grade II and III gliomas, Eckel-Passow et al. showed that only TERT-mutated gliomas, without isocitrate dehydrogenase (IDH) mutation and chromosome 1p/19q codeletion, had significantly poor overall survival [9]. The Consortium to Inform Molecular and Practical Approaches to CNS Tumor Taxonomy (cIMPCT-NOW) update 3 indicates that IDH-wild-type diffuse astrocytic gliomas that contain TERT promoter mutation correspond to WHO grade IV and should be referred to as diffuse astrocytic glioma, IDH-wildtype, with molecular features of glioblastoma, WHO grade IV [10]. From the perspective of prognosis, it is important to establish an assay that can accurately detect TERT promoter mutations in patients with glioma.
The TERT promoter region around hot spot mutations is characterized by a high GC nucleotide content (more than 80%), making stable, specific and reproducible PCR amplification difficult [11,12,13,14]. In the next-generation sequencing with high DNA analysis accuracy, a bridge PCR is performed with a dedicated enzyme and reagent. Gene amplification is unstable under high GC content in the analysis region or at the site of repeated sequences. In addition, it is impossible to detect TERT mutation using immunohistochemistry, because an antibody that specifically recognizes the mutant TERT protein has not been developed. Therefore, in many institutions, Sanger DNA sequencing is the standard method for analyzing TERT mutations. However, this assay also has a PCR step and sensitivity limits, and positive true gene mutations cannot be revealed if 15–20% or more of the cells do not have the gene mutation [15]. Thus, a novel detection method with high sensitivity and good reproducibility is required to analyze TERT promoter mutations, which are an important molecular marker in glioma.
The droplet digital PCR (ddPCR) assay has recently attracted attention as a superior method for the detection and absolute quantification of rare mutated and wild type alleles because of its high sensitivity and robust quantitative performance characteristics [16, 17]. Corless BC et al. showed that the ddPCR assay for TERT promoter mutation detected 0.062% and 0.051% mutant allele fractions for the C228T and C250 mutations in TERT-mutated cancer cells, respectively [18]. We performed TERT mutation analysis using an optimized ddPCR assay for fresh frozen and formalin-fixed paraffin-embedded (FFPE) glioma specimens and verified the difference in results obtained from those obtained using the standard analysis method, the Sanger DNA sequencing.
Materials and methods
Patients and tissue samples
We studied five fresh frozen samples and four FFPE specimens from nine patients with glioma (Table 1). All samples were obtained by surgical resection or biopsy at our institution. Each case was pathologically diagnosed according to 2016 WHO classification [1].
DNA extraction
Genomic DNA was extracted from fresh frozen tissues using DNeasy Tissue kit (Qiagen, Hilden, Germany) according to the manufacture's protocol. FFPE slides were prepared using Maxwell® RSC DNA FFPE Kit (Promega, Madison, WI, USA) by the instruction's manual. Human glioblastoma cell line A172-derived DNA and human epidermoid skin carcinoma cell line A431-derived DNA were purchased from BioChain (CA, USA) and were used as positive controls for TERT C228T and C250T mutations, respectively [18]. The negative control was genomic DNA obtained from normal human peripheral blood cells (Clontech Takara, Shiga, Japan). Concentrations of extracted DNA were measured using NanoDrop® spectrophotometer ND-1000 (Thermo Fisher Scientific, Waltham, MA, USA).
ddPCR
We used mutation-specific primer/probe combinations (dHsaEXD72405942 and dHsaEXD46675715, Bio-Rad) to separately detect C228T and C250T TERT promoter mutations, according to the protocol by Corless BC et al. [18]. Mutant and wild-type alleles were labeled with FAM and HEX, respectively. The reaction mixtures were as follows: 1 X ddPCR Supermix for Probes (No dUTP, Bio-Rad), 1 X primer/probe mixture, 0.5 M Betamine, 2.5 U CviQI restriction enzyme, 1 mM EDTA, template tumor DNA of 10 ng, and distilled water to a final volume of 20 µL.
Droplets were generated using the Automatic Droplet Generator QX200 (Bio-Rad Laboratories, Hercules, CA, USA). PCR amplifications were performed using the following cycle conditions: 1 cycle of at 95 °C (2.5C/s ramp rate) for 10 min, followed by 50 cycles at 96 °C (2.5C/s ramp rate) for 30 s and 62 °C for 1 min, and 1 cycle at 98 °C (2.5C/s ramp rate) for 10 min. The samples were stored at 4 °C until further processing. Droplets were analyzed using a QX200 Droplet Reader (Bio-Rad Laboratories, Hercules, CA, USA) according to the manufacturer’s instructions. The QuantaSoft analysis software version 1.7 (Bio-Rad Laboratories, Hercules, CA, USA) was used to acquire and analyze data.
Sanger DNA sequencing
A total of 20–100 ng of DNA was used as a template for a single DNA sequencing. PCR amplification of TERT promoter hot spots was performed using forward (5′–TCCCTCGGGTTACCCCACAG–3′) and reverse (5′–AAAGGAAGGGGAGGGGCTG–3′) primers, as reported previously [2]. PCRs were performed in a volume of 25 μL containing 2 μL of template DNA, 0.5 μL of 10 μM of each primer, 10μL of AmpliTaq Gold™ 360 Master-Mix (Thermo Fisher Scientific, Waltham, MA, USA), and 1 μL of dimethyl sulfoxide, and distilled water. Cycling conditions were 95 °C for 10 min for initial denaturation, followed by 35 cycles of denaturation at 95 °C for 30 s, annealing at 56 °C for 30 s, and extension at 72 °C for 40 s, and a final elongation at 72 °C for 7 min. Amplification products were purified and cleaned by agarose gel electrophoresis and gel-extracted with the NucleoSpin® gel and PCR clean-up kit (Macherey–Nagel, Dören, Germany) according to the manufacturer’s protocol. Purified products were subjected to cycle sequencing using the BigDye® Terminator v3.1 cycle sequencing kit (Thermo Fisher Scientific, Waltham, MA, USA), with the forward PCR primer used as a sequencing primer. Purification was then performed using the BigDye® Xterminator Purification Kit (Thermo Fisher Scientific, Waltham, MA, USA). Finally, the DNA sequences were determined using an Applied Biosystems 3500 Genetic Analyzer (Applied Biosystems, CA, USA).
Laser microdissection
For a mixed anaplastic oligoastrocytoma (Case 9), we used laser microdissection to separately obtain DNA from the oligodendroglial and astrocytic portions. FFPE tissue block was sectioned and mounted on slides covered with polyethylene–naphthalate (PEN)-membrane and left to dry overnight at room temperature. The sections were stained with toluidine blue. Visualization and microdissection were performed using LMD-7000 (Leica Microsystems, Germany). DNA from each portion was extracted using the Maxwell® RSC DNA FFPE Kit as described for DNA extraction, followed by ddPCR and DNA sequence assays.
Fluorescence in situ hybridization (FISH) for chromosomes 1p and 19q statuses
Five-micrometer-thick paraffin sections of tumors were mounted on positively charged slides and baked at 65 °C overnight. The sections were dewaxed with xylene and ethanol, and treated in 10 mM sodium citrate for 10 min at 80 °C, followed by pepsin digestion (4 mg/mL in saline, pH adjusted to 1.5 with HCl) for 35 min at 37 °C. The sections were denatured for 10 min at 75 °C and hybridized overnight at 75 °C with the two-color FISH probe sets of the differential sites (Vysis LSI 1p36/1q25 and 19q13/19p13 FISH probe kit, Abbott, IL, USA and 1p31/1q25.2 and 19q13.12/19p13.2, GSP Lab, Kobe, Japan). The next day, sections were washed in 50% formamide/1X SSC buffer. Nuclei were counterstained with 4′, 6–diamidino–2–phenylindole, and green and red fluorescent signals were enumerated under an Olympus fluorescence microscope BX51 (Olympus Optical, Tokyo, Japan) with appropriate filters. For each hybridization, 100 non-overlapping nuclei were assessed for numbers of green and red signals. An interpretation of deletion was made when more than 50% of the nuclei harbored only one red or one green signal.
Results
ddPCR assay optimization
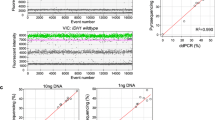
First, we performed a ddPCR assay for DNA from A172 (TERT C228T mutant), A431 (TERT C250T mutant) and peripheral blood cell (TERT wild-type). To evaluate the least detectable fractions of the TERT mutant allele, serial dilutions of mutant TERT DNA from cell lines were mixed with normal peripheral blood cell DNA to generate sample series with mutant fractions ranging from 100 to 0% (100%, 10%, 1%, 0.1%, and 0%). The results were shown as two-dimensional ddPCR plots. Wild-type PCR product fluorescence intensity is presented on the X-axis (HEX) and mutant PCR product fluorescence intensity is presented on the Y-axis (FAM). Next, we set a threshold value of 2000 for the droplet HEX intensity indicating the wild-type and 3000 for the droplet FAM intensity indicating the mutation. This segregated the cluster of droplets with minimal cross-reactivity (< 0.05%, data not shown) and excluded false positives. As shown in Fig. 1, the TERT C228T mutation was present at 48.1% of DNA only from A172 cells and the TERT C250T mutation was present at 33.0% of DNA only from A431 cells, and these mutations were not detected in DNA only from peripheral blood cell. The fraction rate of these mutations obtained through our ddPCR assay was almost equal to that obtained in a previous report [18]. In addition, these control samples were used in all experiments with glioma samples, and the above-mentioned results were reproduced. We could not obtain a detectable mutant fraction from the 0.1% dilution samples of TERT C228T and C250T templates. Therefore, we determined that 1.0% or more of the mutant TERT DNA was detectable in this assay.
Two-dimentional droplet digital PCR (ddPCR) plots showing the C228T and C250T TERT promoter assays. The Y-axis indicates the intensity of the FAM signal (blue) and represents a TERT mutation. The X-axis indicates the intensity of the HEX signal (green) and represents the wild-type. Cross-reactive events for both signals are shown in the upper right corner (brown). The background signals are shown in the bottom-left corner (black). DNA from A172 cells (left panel) and A431 (right panel) were diluted with normal peripheral blood cell DNA to mutant allele fractions of 100%, 10%, 1%, 0.1%, and 0%. The mutation-positive fraction is indicated as a percentage in the upper right corner
Evaluation for TERT promoter mutation using the ddPCR assay in glioma samples
We analyzed TERT promoter mutations in nine glioma samples (five fresh frozen and four FFPE specimens) using our optimized ddPCR assay. We obtained convincing data in a single ddPCR run in all cases (Table 1). Representative cases of TERT promoter mutation are shown in Fig. 2. Case 9 was a dual-genotype mixed anaplastic oligoastrocytoma (Fig. 3A). Genetic codeletion of chromosomes 1p/19q and positive for IDH1 R132H immunohistochemical staining (data not shown) were demonstrated in the oligodendroglial portion but not in the astrocytic portion. According to our ddPCR assay using DNA from micro-dissected tissue section, 31.4% and 0% mutant allele fractions for TERT C228T was observed in the oligodendroglial and astrocytic portions, respectively (Fig. 3B).
Representative ddPCR results. A Rt. fronto-temporal oligodendroglioma (Case 3). Left panel: a fluid-attenuated inversion-recovery (FLAIR) MRI image; Right panel: ddPCR result of this case shows 55.8% of C228T TERT mutation. B Glioblastoma in the corpus callosum (Case 4). Left panel: a contrast-enhanced T1-weighted MRI image; Right panel: ddPCR result of this case shows 59.2% of C250T TERT mutation
Mixed anaplastic oligoastrocytoma (Case 9). A Hematoxylin & eosin staining of the tumor specimen (X200). The tumor displayed oligodendroglial (lower right) and astrocytic (upper left) differentiated portions. B DdPCR plots for TERT mutations display the results from the micro-dissected tissue of each area
Comparison of the ddPCR assay and Sanger DNA sequencing
Subsequently, we performed Sanger DNA sequencing using the same DNA that had undergone ddPCR and compared the results for TERT mutation. As mentioned in Introduction, Sanger DNA sequencing is a low-sensitivity method. The sequencing was repeated up to three times if the result of the first sequencing was different from that obtained through the ddPCR assay. When performing the second or third sequencing, we restarted from the PCR step. The comparison results between ddPCR and Sanger DNA sequence are shown on the right side of Table 1. In the case of fresh frozen tissues, DNA sequencing results of the second sequencing were concordant with the results obtained using the ddPCR assay. However, when FFPE specimens were used, more time was required to evaluate TERT mutations through Sanger DNA sequencing. For example, Case 7 was a glioblastoma, IDH-wildtype patient, with a FFPE specimen. The ddPCR assay showed a TERT C250T mutation of 37.8% for this case (Fig. 4A). In the first and second Sanger DNA sequencing, we could not read the nucleotides peaks because of baseline noise and oddly spaced interstitial peaks. Finally satisfactory results were obtained in the third sequencing (Fig. 4B). In Case 9, DNA extracted from the micro-dissected specimens was very small and could not be amplified by PCR at all three times of sequencing step (Table 1).
DdPCR and Sanger DNA sequencing results using FFPE glioblastoma specimens (Case 7). A ddPCR plot for TERT C250T mutation assay. B Sanger DNA sequencing for the same FFPE sample. Left panel: result of the first sequencing was No call; Right panel: The third-time sequencing showed C250T mutation at 146 bp, upstream of the TERT transcriptional start site. Arrow indicates the heterozygous C/T bases at this site
Discussion
Here we showed that the ddPCR assay was able to analyze TERT promoter mutations in DNA obtained from fresh frozen and FFPE glioma specimens with very high sensitivity compared to the traditional Sanger DNA sequencing method. Our ddPCR assay for TERT promoter mutation can detect a mutant allele fraction of 1.0% of mutant TERT DNA. This detection limit is significantly lower than those reported for other mutation detection assays such as next generation sequencing (2%), pyrosequencing (5%), and Sanger DNA sequencing (15–20%) [15, 19]. Our results show the preliminary data obtained from nine glioma samples. A validation study of the ddPCR assay for many cases is necessary and is currently in progress. It took a short time of approximately 2.5 h to analyze the nine glioma DNA samples that we prepared. The cost of the ddPCR assay was 1.2 times higher than that of the Sanger sequencing per sample. However, the costs of both were almost the same if 20 or more samples were assayed simultaneously. Although ddPCR misses genetic alterations other than its targeted mutation, it remains an extremely useful assay for the gene analysis of single nucleotide polymorphisms, for which known mutation sites are known, such as TERT promoter mutations. This assay may also sensitively detect hot spot mutations, such as IDH1/2, H3F3A K27M, and BRAFV600E mutations, in a subset of glioma [1, 20,21,22].
The Sanger DNA sequencing, used as a standard assay in many institutions for TERT mutation detection, is problematic as shown in this study. Three of the four FFPE samples did not give clear sequencing results, even in two sequencing assays. This may be because that the DNA quantification method used by us did not correctly assess the concentration of FFPE-derived samples. However, DNA damage and base transitions occur more frequently in FFPE samples than in frozen samples [23]. In addition, the high GC content (more than 80%) within the TERT promoter region makes it more difficult for efficient and specific PCR assay to detect TERT mutations [11, 14]. Miki S et al. reported that, since the Sanger DNA sequence has low-sensitivity and is non-quantitative, TERT mutant cells are possibly masked by TERT non-mutant cells, and sequencing results do not reveal positivity for mutation even in fresh frozen samples [24]. However, by increasing the mutation abundance ratio per compartment by compartmentalization with droplets, rare gene mutations can be detected without being buried in the background as long as there is a PCR-amplified gene [16]. As Diplas BH et al. inferred, the true frequency of TERT mutations in gliomas, as determined by ddPCR analysis, may actually be higher than previously reported [25].
As mentioned above, ddPCR is highly sensitive assay that can detect a small fraction of TERT-mutated alleles. TERT mutations were successfully verified using 10 ng DNA as a template in this study. It was possible to analyze a very small amount of DNA microdissectioned from the FFPE section. We found a TERT mutation that was detected only in the oligogenendroglial portion that was composed of mixed glioma. This ddPCR assay can detect TERT mutations with a small amount of tumor DNA template of 1 ng (unpublished data). Therefore, ddPCR can be applied to liquid biopsies using circulating cell-free DNA (ccfDNA). Muralidharan K et al. reported the feasibility of a ddPCR-based TERT promoter mutation assay for ccfDNA from the plasma of glioma patients [26]. According to their results, overall sensitivity and specificity for detecting ccfDNA TERT promoter mutations in plasma compared with those for detecting ccfDNA TERT promoter mutations in matched tumor tissues were 62.5% and 90%, respectively. Cerebrospinal fluid is better than plasma and a more frequent reservoir of tumor DNA in glioma patients [27]. Using ccfDNA obtained from cerebrospinal fluid, detection of TERT mutation may be more accurate in liquid biopsy of glioma.
It is also attractive that ddPCR is a quantitative method. The Consortium to Inform Molecular and Practical Approaches to CNS Tumor Taxonomy (cIMPCT-NOW) update 3 reported that the presence of TERT mutations predicted an aggressive clinical course in IDH wild-type astrocytic tumors with molecular features of glioblastoma, WHO grade IV [10]. Therefore, it would be interesting to determine whether the number of TERT-mutant tumor cells is relevant to clinical parameters, such as tumor growth rate, resistance to treatment, and poor survival. The ddPCR assay is a powerful tools for answering these questions.
In summary, we demonstrated here, the validity of a ddPCR assay for specifically detecting C228T and C250T promoter mutations in the TERT gene. Especially for FFPE sections, ddPCR has been shown to be far superior to the standard analytical method, Sanger DNA sequencing. The ddPCR assay enables highly sensitive analysis of TERT mutations, even using a small amount of micro-dissectioned DNA, and is expected to be applicable to liquid biopsy in glioma. These results suggest that this assay is a potential tool for diagnosing and monitoring patients with glioma and TERT mutations as well as for the development of drugs targeting telomere lengthening.
References
Louis DN, Ohgaki H, Wiestler OD et al (2016) WHO classification of tumours of the central nervous system, 4th edn. IARC, Lyon
Arita H, Narita Y, Fukushima S, Tateishi K, Matsushita Y, Yoshida A, Miyakita Y, Ohno M, Collins VP, Kawahara N, Shibui S, Ichimura K (2013) Upregulating mutations in the TERT promoter commonly occur in adult malignant gliomas and are strongly associated with total 1p19q loss. Acta Neuropathol 126:267–276
Killela PJ, Reitman ZJ, Jiao Y, Bettegowda C, Agrawal N, Diaz LA, Friedman AH, Friedman H, Gallia GL, Giovanella BC (2013) TERT promoter mutations occur frequently in gliomas and a subset of tumors derived from cells with low rates of self-renewal. Proc Natl Acad Sci USA 110:6021–6026
Bell RJA, Rube HT, Xavier-Magalhaes A, Costa BM, Mancini A, Song JS, Costello JF (2016) Understanding TERT promoter mutations: a common path to immortality. Mol Cancer Res 14:315–323
Horn S, Figl A, Rachakonda PS, Fischer C, Sucker A, Gast A, Kadel S, Moll I, Nagore E, Hemminki K, Schadendorf D, Kumar R (2013) TERT promoter mutations in familial and sporadic melanoma. Science 339:959–961
Huang FW, Hodis E, Xu MJ, Kryukov GV, Chin L, Garraway LA (2013) Highly recurrent TERT promoter mutations in human melanoma. Science 339:957–959
Castelo-Branco P, Choufani S, Mack S, Gallagher D, Zhang C, Lipman T, Zhukova N, Walker EJ, Martin D, Merino D, Wasserman JD, Elizabeth C, Alon N, Zhang L, Hovestadt V, Kool M, Jones DT, Zadeh G, Croul S, Hawkins C, Hitzler J, Wang JC, Baruchel S, Dirks PB, Malkin D, Pfister S, Taylor MD, Weksberg R, Tabori U (2013) Methylation of the TERT promoter and risk stratifi cation of childhood brain tumours: an integrative genomic and molecular study. Lancet Oncol 14:534–542
Huang DS, Wang Z, He XJ, Diplas BH, Yang R, Killela PJ, Meng Q, Ye ZY, Wang W, Jiang XT, Xu L, He XL, Zhao ZS, Xu WJ, Wang HJ, Ma YY, Xia YJ, Li L, Zhang RX, Jin T, Zhao ZK, Xu J, Yu S, Wu F, Liang J, Wang S, Jiao Y, Yan H, Tao HQ (2015) Recurrent TERT promoter mutations identified in a large-scale study of multiple tumor types are associated with increased TERT expression and telomerase activation. Eur J Cancer 51:969–976
Eckel-Passow JE, Lachance DH, Molinaro AM, Walsh KM, Decker PA, Sicotte H, Pekmezci M, Rice T, Kosel ML, Smirnov IV, Gobinda S, Caron AA et al (2015) Glioma groups based on 1p/19q, IDH, and TERT promoter mutations in tumors. N Engl J Med 372:2499–2508
Brat DJ, Aldape K, Colman H, Holland EC, Louis DN, Jenkins RB, Kleinschmidt-DeMasters B, Perry A, Reifenberger G, Stupp R (2018) cIMPACT-NOW update 3: recommended diagnostic criteria for “diffuse astrocytic glioma, IDH-wildtype, with molecular features of glioblastoma, WHO grade IV.” Acta Neuropathol 136:805–810
Cong YS, Wen J, Bacchetti S (1999) The human telomerase catalytic subunit hTERT: organization of the gene and characterization of the promoter. Hum Mol Genet 8(1):137–142
Kang S, Ohshima K, Shimizu M, Amirhaeri S, Wells RD (1995) Pausing of DNA synthesis in vitro at specific loci in CTG and CGG triplet repeats from human hereditary disease genes. J Biol Chem 270:27014–27021
Motz M, Pääbo S, Kilger C (2000) Improved cycle sequencing of GC-rich templates by a combination of nucleotide analogs. Biotechniques 29:268–270
Frey UH, Bachmann HS, Peters J, Siffert W (2008) PCR-amplification of GC-rich regions: “slowdown PCR. Nat Protoc 3:1312–1317
Tsiatis AC, Norris-Kirby A, Rich RG, Hafez MJ, Gocke CD, Eshleman JR, Murphy KM (2010) Comparison of Sanger sequencing, pyrosequencing, and melting curve analysis for the detection of KRAS mutations: diagnostic and clinical implications. J Mol Diagn 12:425–432
Hinson BJ, Ness KD, Masqelier DA, Belgrader P, Heredia NJ, Makarewicz AJ, Bright IJ, Lucero MY, Hiddessen AL, Legler TC, Kitano TK et al (2011) High- throughput droplet digital PCR system for absolute quantitation of DNA copy number. Anal Chem 83(22):8604–8610
McEvoy AC, Calapre L, Pereira MR, Giardina T, Robinson C, Khattak MA, Meniawy TM, Pritchard AL, Hayward NK, Amanuel B, Millward M, Ziman M, Gray ES (2017) Sensitive droplet digital PCR method for detection of TERT promoter mutations in cell free DNA from patients with metastatic melanoma. Oncotarget 8(45):78890–78900
Corless BC, Chang GA, Cooper S, Syeda MM, Shao Y, Osman I, Karlin-Neumann G, Polsky D (2019) Development of novel mutation-specific droplet digital PCR assays detecting TERT promoter mutations in tumor and plasma samples. J Mol Diagn 21(2):274–285
Ming-Tseh L, Stacy LM, Michele T, Katie FB, Marija D, Li-Hui T, Guoli C, Srinivasan Y, Hao H, Leslie C, Sarah JW, Christopher DG, James RE (2014) Clinical validation of KRAS, BRAF, and EGFR mutation detection using next-generation sequencing. Am J Clin Pathol 141(6):856–866
Hirano M, Ohka F, Maeda S, Chalise L, Yamamichi A, Aoki K, Kato A, Tanahashi K, Motomura K, Nishimura Y, Hara M, Shinjo K, Kondo Y, Wakabayashi T, Natsume A (2018) A novel high-sensitivity assay to detect a small fraction of mutant IDH1 using droplet digital PCR. Brain Tumor Pathol 35:97–105
Reid AL, Freeman JB, Millward M, Ziman M, Gray ES (2015) Detection of BRAF-V600E and V600K in melanoma circulating tumour cells by droplet digital PCR. Clin Biochem 48:999–1002
Fujioka Y, Hata N, Akagi Y, Kuga D, Hatae R, Sangatsuda Y, Michiwaki Y, Amemiya T, Takigawa K, Funakoshi Y, Sako A, Iwaki T, Lihara K, Mizoguchi M (2021) Molecular diagnosis of diffuse glioma using a chip-based digital PCR system to analyze IDH, TERT, and H3 mutations in the cerebrospinal fluid. J Neurooncol 152:47–54
Williams C, Ponten F, Moberg C, Soderkvist P, Uhlen M, Ponten J, Sitbon G, Lundeberg J (1999) A high frequency of sequence alterations is due to formalin fixation of archival specimens. Am J Pathol 155:1467–1471
Miki S, Satomi K, Ohno M, Matsushita Y, Kitahara M, Miyakita Y, Takahashi M, Matsuda M, Ishikawa E, Matsumura A, Yoshida A, Narita Y, Ichimura K (2020) Highly sensitive detection of TERT promoter mutations in recurrent glioblastomas using digital PCR. Brain Tumor Pathol 37:154–158
Diplas BH, Liu H, Yang R, Hansen LJ, Zachem AL, Zhao F, Bigner DD, McLendon RE, Jiao Y, Waitkus HY, Yan H (2018) Sensitive and rapid detection of TERT promoter and IDH mutations in diffuse gliomas. Neuro Oncol 21:440–450
Muralidharan K, Yekula A, Small JL, Rosh ZS, Kang KM, Wang L, Lau S, Zhang H, Lee H, Bettegowda C, Chicoine MR, Kalkanis SN et al (2021) TERT promoter mutation analysis for blood-based diagnosis and monitoring of gliomas. Clin Cancer Res 27(1):169–178
Miller AM, Shah RH, Pentsova EI, Pourmaleki M, Briggs S, Distefano N, Zheng Y, Skakodub A, Mehta SA, Campos C, Hsieh WY, Selcuklu SD et al (2019) Tracking tumour evolution in glioma through liquid biopsies of cerebrospinal fluid. Nature 565(7741):654–658
Acknowledgements
This work was supported by a Grant-in-Aid for Scientific Research (C) from the Japan Society for the Promotion of Science (JSPS KAKENHI Grant Number 18K09003), 2018-2020. We would like to thank Ms. Kaoru Katsura and Ms. Ayako Kubota for their technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest related to this work.
Ethical approval
All samples were collected and analyzed in accordance with the Declaration of Helsinki (2013). This study was included in Investigation of Brain Tumor Pathogenesis Using Multimodal Neuroimage, which was approved by the Institutional Review Board of Saitama Medical University International Medical Center.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Adachi, Ji., Shirahata, M., Suzuki, T. et al. Droplet digital PCR assay for detecting TERT promoter mutations in patients with glioma. Brain Tumor Pathol 38, 201–209 (2021). https://doi.org/10.1007/s10014-021-00403-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10014-021-00403-4