Abstract
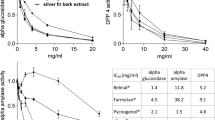
The acacia bark extract derived from Acacia mearnsii De Wild is rich in proanthocyanidins, whose constituent units are robinetinidol, fisetinidol, catechin, and gallocatechin. In this study, we examined the effect of proanthocyanidins on obesity and diabetes using KKAy mice, a type 2 diabetes model. KKAy mice were fed either a low-fat diet, a high-fat diet, or a high-fat diet mixed with an acacia bark extract, a proanthocyanidins fraction, and other fraction for 7 weeks. Monitoring the changes in the body weight revealed that acacia bark extract and proanthocyanidins fraction could prevent excessive weight gain resulting from a high-fat diet. In addition, increases in the fasting blood glucose level due to high-fat diet intake were found to be suppressed by acacia bark extract and proanthocyanidins fraction. Furthermore, proanthocyanidins derived from acacia bark were found to increase the expression of adiponectin in white adipose tissue, which enhances the action of insulin. In addition, acacia bark-derived proanthocyanidins suppressed gluconeogenesis and fatty acid synthesis in the liver, as well as suppressing the decrease in energy production under pathological conditions in skeletal muscle. In addition, acacia bark-derived proanthocyanidins showed AMPK activation and DPP-4 inhibitory action. Therefore, it was suggested that acacia bark-derived proanthocyanidins lowered fasting blood glucose levels through the above mechanism. These results suggest that proanthocyanidins derived from acacia bark are the active ingredients of the anti-obesity and anti-diabetic effects of acacia bark extract.
Graphic abstract

Access this article
We’re sorry, something doesn't seem to be working properly.
Please try refreshing the page. If that doesn't work, please contact support so we can address the problem.








Similar content being viewed by others
References
Ikarashi N, Toda T, Hatakeyama Y, Kusunoki Y, Kon R, Mizukami N, Kaneko M, Ogawa S, Sugiyama K (2018) Anti-hypertensive effects of acacia polyphenol in spontaneously hypertensive rats. Int J Mol Sci. https://doi.org/10.3390/ijms19030700
Xiong J, Grace MH, Esposito D, Komarnytsky S, Wang F, Lila MA (2017) Polyphenols isolated from Acacia mearnsii bark with anti-inflammatory and carbolytic enzyme inhibitory activities. Chin J Nat Med 15:816–824. https://doi.org/10.1016/S1875-5364(18)30015-3
Xiong J, Graceb MH, Esposito D, Wang F, Lila MA (2016) Phytochemical characterization and anti-inflammatory properties of Acacia mearnsii leaves. Nat Prod Commun 11:649–653
Ikarashi N, Toda T, Okaniwa T, Ito K, Ochiai W, Sugiyama K (2011) Anti-obesity and anti-diabetic effects of acacia polyphenol in obese diabetic KKAy mice fed high-fat diet. Evid Based Complement Alternat Med 2011:952031. https://doi.org/10.1093/ecam/nep241
Kusano R, Ogawa S, Matsuo Y, Tanaka T, Yazaki Y, Kouno I (2011) alpha-Amylase and lipase inhibitory activity and structural characterization of acacia bark proanthocyanidins. J Nat Prod 74:119–128. https://doi.org/10.1021/np100372t
Ikarashi N, Takeda R, Ito K, Ochiai W, Sugiyama K (2011) The inhibition of lipase and glucosidase activities by acacia polyphenol. Evid Based Complement Alternat Med 2011:272075. https://doi.org/10.1093/ecam/neq043
Ogawa S, Matsuo Y, Tanaka T, Yazaki Y (2018) Utilization of flavonoid compounds from bark and wood. III. Application in health foods. Molecules. https://doi.org/10.3390/molecules23081860
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419. https://doi.org/10.1007/bf00280883
Sasaki Y, Suzuki W, Shimada T, Iizuka S, Nakamura S, Nagata M, Fujimoto M, Tsuneyama K, Hokao R, Miyamoto K, Aburada M (2009) Dose dependent development of diabetes mellitus and non-alcoholic steatohepatitis in monosodium glutamate-induced obese mice. Life Sci 85:490–498. https://doi.org/10.1016/j.lfs.2009.07.017
Borst SE (2004) The role of TNF-alpha in insulin resistance. Endocrine 23:177–182. https://doi.org/10.1385/ENDO:23:2-3:177
Kadowaki T, Yamauchi T, Kubota N, Hara K, Ueki K, Tobe K (2006) Adiponectin and adiponectin receptors in insulin resistance, diabetes, and the metabolic syndrome. J Clin Invest 116:1784–1792. https://doi.org/10.1172/JCI29126
Guillou H, Martin PG, Pineau T (2008) Transcriptional regulation of hepatic fatty acid metabolism. Subcell Biochem 49:3–47. https://doi.org/10.1007/978-1-4020-8831-5_1
Okumura T, Kohgo Y (2006) Increased expression of PPargamma in fatty liver induced by high fat diet. Nihon Rinsho 64:1056–1061
Tanaka T, Masuzaki H, Ebihara K, Ogawa Y, Yasue S, Yukioka H, Chusho H, Miyanaga F, Miyazawa T, Fujimoto M, Kusakabe T, Kobayashi N, Hayashi T, Hosoda K, Nakao K (2005) Transgenic expression of mutant peroxisome proliferator-activated receptor gamma in liver precipitates fasting-induced steatosis but protects against high-fat diet-induced steatosis in mice. Metabolism 54:1490–1498. https://doi.org/10.1016/j.metabol.2005.05.015
Kim JK, Fillmore JJ, Chen Y, Yu C, Moore IK, Pypaert M, Lutz EP, Kako Y, Velez-Carrasco W, Goldberg IJ, Breslow JL, Shulman GI (2001) Tissue-specific overexpression of lipoprotein lipase causes tissue-specific insulin resistance. Proc Natl Acad Sci USA 98:7522–7527. https://doi.org/10.1073/pnas.121164498
Tanaka T, Yamamoto J, Iwasaki S, Asaba H, Hamura H, Ikeda Y, Watanabe M, Magoori K, Ioka RX, Tachibana K, Watanabe Y, Uchiyama Y, Sumi K, Iguchi H, Ito S, Doi T, Hamakubo T, Naito M, Auwerx J, Yanagisawa M, Kodama T, Sakai J (2003) Activation of peroxisome proliferator-activated receptor delta induces fatty acid beta-oxidation in skeletal muscle and attenuates metabolic syndrome. Proc Natl Acad Sci USA 100:15924–15929. https://doi.org/10.1073/pnas.0306981100
Villarroya F, Iglesias R, Giralt M (2007) PPARs in the control of uncoupling proteins gene expression. PPAR Res 2007:74364. https://doi.org/10.1155/2007/74364
Wang YX, Zhang CL, Yu RT, Cho HK, Nelson MC, Bayuga-Ocampo CR, Ham J, Kang H, Evans RM (2004) Regulation of muscle fiber type and running endurance by PPARdelta. PLoS Biol 2:e294. https://doi.org/10.1371/journal.pbio.0020294
Yoon MJ, Lee GY, Chung JJ, Ahn YH, Hong SH, Kim JB (2006) Adiponectin increases fatty acid oxidation in skeletal muscle cells by sequential activation of AMP-activated protein kinase, p38 mitogen-activated protein kinase, and peroxisome proliferator-activated receptor alpha. Diabetes 55:2562–2570. https://doi.org/10.2337/db05-1322
Inamdar S, Joshi A, Malik S, Boppana R, Ghaskadbi S (2019) Vitexin alleviates non-alcoholic fatty liver disease by activating AMPK in high fat diet fed mice. Biochem Biophys Res Commun 519:106–112. https://doi.org/10.1016/j.bbrc.2019.08.139
Koo SH, Flechner L, Qi L, Zhang X, Screaton RA, Jeffries S, Hedrick S, Xu W, Boussouar F, Brindle P, Takemori H, Montminy M (2005) The CREB coactivator TORC2 is a key regulator of fasting glucose metabolism. Nature 437:1109–1111. https://doi.org/10.1038/nature03967
Leclerc I, Lenzner C, Gourdon L, Vaulont S, Kahn A, Viollet B (2001) Hepatocyte nuclear factor-4alpha involved in type 1 maturity-onset diabetes of the young is a novel target of AMP-activated protein kinase. Diabetes 50:1515–1521. https://doi.org/10.2337/diabetes.50.7.1515
Acknowledgements
We thank Satoshi Kitaoka (Department of clinical pharmacokinetics) for technical assistance. We would like to thank Editage (www.editage.com) for English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Financial interests: W. Ochiai has received research support from Company Acacia-No-Ki Co., Ltd.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kashiwada, M., Nakaishi, S., Usuda, A. et al. Analysis of anti-obesity and anti-diabetic effects of acacia bark-derived proanthocyanidins in type 2 diabetes model KKAy mice. J Nat Med 75, 893–906 (2021). https://doi.org/10.1007/s11418-021-01537-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11418-021-01537-7