Abstract
Background
Although lymph node metastasis is a known factor predictive of a poor prognosis after radical surgery for intrahepatic cholangiocarcinoma (ICC), few studies have investigated lymph node dissection (LND) areas for accurate staging. The aim of this study was to identify the optimal LND level for ICC considering lymphatic flow.
Methods
Clinical characteristics and pathologic nodal status (presence of metastasis) for 163 patients were reviewed according to tumor location. In the node-positive (N1) group, the distribution of metastatic nodes was described. The coverage of metastatic nodes according to dissection level was assessed, and the minimum dissection level for accurate ICC staging was estimated accordingly. For validation, the node-negative (N0) group was divided into two subgroups according to the estimated dissection level, and survival outcomes were compared.
Results
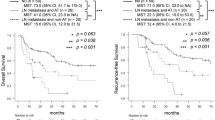
In the N1 group, expanding dissection to stations no. 12 and 8 covered 82.0% (n = 50) of metastatic cases regardless of tumor location. In survival analysis of N0 group, patients who underwent LND covering stations no. 8+12 showed better disease-free survival (DFS) and overall survival (OS), although the differences were not statistically significant (DFS: covering no. 12+8 vs. not covering no. 12+8, 109.0 months [24.2–193.8] vs. 33.0 months [10.3–55.7], p = 0.078; OS: covering no. 12+8 vs. not covering no. 12+8, 180.0 months [21.6–338.4] vs. 73.0 months [42.8–103.2], p = 0.080).
Conclusion
LND including at least stations no. 12 (hepatoduodenal ligament) and 8 (common hepatic artery), regardless of tumor location, is recommended for accurate staging in ICC patients.



Similar content being viewed by others
References
Endo I, Gonen M, Yopp AC, Dalal KM, Zhou Q, Klimstra D, D'Angelica M, DeMatteo RP, Fong Y, Schwartz L, Kemeny N, O'Reilly E, Abou-Alfa GK, Shimada H, Blumgart LH, Jarnagin WR. Intrahepatic cholangiocarcinoma: rising frequency, improved survival, and determinants of outcome after resection. Ann Surg 2008;248(1):84-96.
Mavros MN, Economopoulos KP, Alexiou VG, Pawlik TM. Treatment and Prognosis for Patients With Intrahepatic Cholangiocarcinoma: Systematic Review and Meta-analysis. JAMA Surg 2014;149(6):565-574.
Amin MB, Edge SB, Greene FL, Byrd DR, Brookland RK, Washington MK, Gershenwald JE, Compton CC, Hess KR, Sullivan DC. AJCC Cancer Staging Manual: Springer International Publishing, 2016.
Choi SB, Kim KS, Choi JY, Park SW, Choi JS, Lee WJ, Chung JB. The prognosis and survival outcome of intrahepatic cholangiocarcinoma following surgical resection: association of lymph node metastasis and lymph node dissection with survival. Ann Surg Oncol 2009;16(11):3048-3056.
Shimada K, Sano T, Nara S, Esaki M, Sakamoto Y, Kosuge T, Ojima H. Therapeutic value of lymph node dissection during hepatectomy in patients with intrahepatic cholangiocellular carcinoma with negative lymph node involvement. Surgery 2009;145(4):411-416.
Kim DH, Choi DW, Choi SH, Heo JS, Kow AW. Is there a role for systematic hepatic pedicle lymphadenectomy in intrahepatic cholangiocarcinoma? A review of 17 years of experience in a tertiary institution. Surgery 2015;157(4):666-675.
Weber SM, Ribero D, O'Reilly EM, Kokudo N, Miyazaki M, Pawlik TM. Intrahepatic cholangiocarcinoma: expert consensus statement. HPB (Oxford) 2015;17(8):669-680.
Kim SH, Han DH, Choi GH, Choi JS, Kim KS. Oncologic Impact of Lymph Node Dissection for Intrahepatic Cholangiocarcinoma: a Propensity Score-Matched Study. J Gastrointest Surg 2019;23(3):538-544.
Yoh T, Cauchy F, Le Roy B, Seo S, Taura K, Hobeika C, Dokmak S, Farges O, Gelli M, Sa Cunha A, Adam R, Uemoto S, Soubrane O. Prognostic value of lymphadenectomy for long-term outcomes in node-negative intrahepatic cholangiocarcinoma: A multicenter study. Surgery 2019;166(6):975-982.
Zhang XF, Xue F, Dong DH, Weiss M, Popescu I, Marques HP, Aldrighetti L, Maithel SK, Pulitano C, Bauer TW, Shen F, Poultsides GA, Soubrane O, Martel G, Koerkamp BG, Itaru E, Lv Y, Pawlik TM. Number and Station of Lymph Node Metastasis After Curative-intent Resection of Intrahepatic Cholangiocarcinoma Impact Prognosis. Ann Surg 2020.
Kim SH, Han DH, Choi GH, Choi JS, Kim KS. Recommended Minimal Number of Harvested Lymph Nodes for Intrahepatic Cholangiocarcinoma. J Gastrointest Surg 2020.
Benson A, Abrams T, Ben-Josef E. NCCN clinical practice guidelines in oncology: hepatobiliary cancers, Version 1.2019. Journal of the National Comprehensive Cancer Network 2019.
Miyazaki M, Ohtsuka M, Miyakawa S, Nagino M, Yamamoto M, Kokudo N, Sano K, Endo I, Unno M, Chijiiwa K, Horiguchi A, Kinoshita H, Oka M, Kubota K, Sugiyama M, Uemoto S, Shimada M, Suzuki Y, Inui K, Tazuma S, Furuse J, Yanagisawa A, Nakanuma Y, Kijima H, Takada T. Classification of biliary tract cancers established by the Japanese Society of Hepato-Biliary-Pancreatic Surgery: 3(rd) English edition. J Hepatobiliary Pancreat Sci 2015;22(3):181-196.
Tsuji T, Hiraoka T, Kanemitsu K, Takamori H, Tanabe D, Tashiro S. Lymphatic spreading pattern of intrahepatic cholangiocarcinoma. Surgery 2001;129(4):401-407.
Bartsch F, Heinrich S, Roth W, Lang H. [Lymphadenectomy in oncological visceral surgery-Part 1 : Hepatobiliary tumors and pancreatic cancer]. Chirurg 2019;90(5):423-438.
Sahara K, Tsilimigras DI, Merath K, Bagante F, Guglielmi A, Aldrighetti L, Weiss M, Bauer TW, Alexandrescu S, Poultsides GA, Maithel SK, Marques HP, Martel G, Pulitano C, Shen F, Soubrane O, Koerkamp BG, Matsuyama R, Endo I, Pawlik TM. Therapeutic Index Associated with Lymphadenectomy Among Patients with Intrahepatic Cholangiocarcinoma: Which Patients Benefit the Most from Nodal Evaluation? Ann Surg Oncol 2019;26(9):2959-2968.
Zhou R, Lu D, Li W, Tan W, Zhu S, Chen X, Min J, Shang C, Chen Y. Is lymph node dissection necessary for resectable intrahepatic cholangiocarcinoma? A systematic review and meta-analysis. HPB (Oxford) 2019;21(7):784-792.
Navarro JG, Lee JH, Kang I, Rho SY, Choi GH, Han DH, Kim KS, Choi JS. Prognostic significance of and risk prediction model for lymph node metastasis in resectable intrahepatic cholangiocarcinoma: do all require lymph node dissection? HPB (Oxford) 2020.
Trutmann M, Sasse D. The lymphatics of the liver. Anatomy and embryology 1994;190(3):201-209.
Morine Y, Shimada M. The value of systematic lymph node dissection for intrahepatic cholangiocarcinoma from the viewpoint of liver lymphatics. J Gastroenterol 2015;50(9):913-927.
Yong TL, Houli N, Christophi C. Anatomy of hepatic lymphatics and its implications in hepatic malignancies. ANZ J Surg 2016;86(11):868-873.
Ohtani O, Ohtani Y. Lymph circulation in the liver. Anat Rec (Hoboken) 2008;291(6):643-652.
Okami J, Dono K, Sakon M, Tsujie M, Hayashi N, Fujiwara Y, Nagano H, Umeshita K, Nakamori S, Monden M. Patterns of regional lymph node involvement in intrahepatic cholangiocarcinoma of the left lobe. J Gastrointest Surg 2003;7(7):850-856.
Nakayama T, Tsuchikawa T, Shichinohe T, Nakamura T, Ebihara Y, Hirano S. Pathological confirmation of para-aortic lymph node status as a potential criterion for the selection of intrahepatic cholangiocarcinoma patients for radical resection with regional lymph node dissection. World J Surg 2014;38(7):1763-1768.
Acknowledgements
The authors thank Medical Illustration & Design, part of the Medical Research Support Services of Yonsei University College of Medicine, for all artistic support related to this work.
Author information
Authors and Affiliations
Contributions
Sung Hyun Kim: design of the work, analysis of data, and drafting the work. Dai Hoon Han: acquisition of data and agreement to be accountable for all aspects of the work. Gi Hong Choi: acquisition of data and agreement to be accountable for all aspects of the work. Jin Sub Choi: acquisition of data and agreement to be accountable for all aspects of the work. Kyung Sik Kim: critical revision and final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, S.H., Han, D.H., Choi, G.H. et al. Extent of Lymph Node Dissection for Accurate Staging in Intrahepatic Cholangiocarcinoma. J Gastrointest Surg 26, 70–76 (2022). https://doi.org/10.1007/s11605-021-05039-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-021-05039-5