Abstract
Objective
Eradication of Helicobacter pylori (H. pylori) could not completely prevent the progression of gastric cancer (GC), suggesting that non-H. pylori bacteria may participate in the carcinogenesis of GC. The dysbiosis of microbiota in the stomach of GC has gradually been investigated, while the detailed mechanism that promotes GC in this process has not been elucidated. We aimed to identify a non-H. pylori bacteria that contribute to GC.
Design
GC tissues and adjacent normal tissues were collected to identify bacteria that significantly increased in GC tissues by 16S rRNA gene sequencing and fluorescence in situ hybridization (FISH) analysis. CCK8, wound healing assay, and trans-well assay were performed to analyze the tumor-promoting effect of this bacteria. Next, we detailed the mechanism for tumor-promoting effect of the bacteria by immunofluorescence, RT-qPCR, and western-blotting analysis.
Results
Comparing the microbial community from GC tissues and adjacent normal tissues, we found that Propionibacterium acnes (P. acnes) significantly increased in GC tissues, especially in H. pylori-negative tissues. We further found that the abundance of P. acnes correlated with TNM stages of GC patients. Interestingly, condition medium (CM) from P. acnes-primed macrophages promoted migration of GC cells, while P. acnes only could not. We next proved that P. acnes triggers M2 polarization of macrophages via TLR4/PI3K/Akt signaling.
Conclusions
Together, our finding identified that P. acnes could be a possible agent for the progression of GC besides H. pylori. M2 polarization of macrophages could be promoted by P. acnes via TLR4/PI3K/Akt signaling, thus triggers the progression of GC.
Similar content being viewed by others
Introduction
Gastric cancer (GC) ranks third in terms of cancer-related deaths worldwide [1], which is generally accepted that infection of Helicobacter pylori (H. pylori) was the most common risk factor. However, in addition to H. pylori colonization, there is a large number of non-H. pylori bacteria colonized in the gastric mucosa [2]. Studies demonstrated that only 1–3% of H. pylori-infected individuals will develop GC despite the fact that colonization rates of H. pylori exceed 50% worldwide [3]. Besides, the development of GC could not be completely prevented by eradication of H. pylori [4]. Moreover, though a high prevalence of H. pylori infection existed, like India and Bangladesh, a low incidence of GC was reported [5]. Furthermore, compared with INS-GAS mouse (a model of spontaneous GC) infected with H. pylori and other gastric flora, the onset of tumorigenesis was delayed in mouse infected with H. pylori alone [6], which indicated that H. pylori may not act alone to promote gastric cancer. Several studies also demonstrated that bacteria other than H. pylori also play a significant role in the carcinogenesis and progression of GC in mice [7, 8]. Together, these novel findings highlighted the essential roles of microbes other than H. pylori in the development of GC.
To date, dysbiosis of gastric microbiota was found in many studies, from non-atrophic gastritis (NAG) to intestinal metaplasia (IM), and to GC. They detected that the abundance of Helicobacteria was decreased, while intestinal commensals were increased [9, 10]. Another study demonstrated that Prevotella melaninogenica, Streptococcus anginosus and Propionibacterium acnes were increased in GC tissues after analyzing tissues from 276 patients with GC [11]. However, as much as we know, there are few studies on the mechanism of GC caused by these disordered microbiota.
A strong correlation between microbes and cancer has long been reported, macrophages play an incredible function in it [12]. Besides, previous studies have demonstrated that macrophages, mainly M2 polarized macrophages, play an essential role in the progression of GC [13]. Infiltration of M2 macrophage in GC tissues has been reported to be a valuable prognostic marker [14]. It was generally accepted that M2 macrophages enhanced angiogenesis and created an immunosuppressive microenvironment in tumor, and targeted M2 macrophages in GC could be a potential therapeutic strategy [15].
Therefore, in the current study, we aimed to investigate the dysbiosis of gastric microbiota, identifying a possible bacteria that contribute to GC. We further explored the function of this bacteria in the progression of GC and studied whether this bacteria could promote the progression of GC via favoring M2 polarization.
Materials and methods
Sample collection
Gastric cancer tissues and adjacent normal tissues (at least 5 cm away from the tumor site) were obtained from patients who were diagnosed with gastric cancer and underwent surgical resection in Renmin Hospital of Wuhan University between November 2020 and May 2021 (Wuhan, China), none of these patients receive antibiotics treatment or use proton pump inhibitors within the previous 2 months. Formalin-fixed, paraffin-embedded GC tissues and paired normal tissues were collected from the pathology department of Renmin Hospital of Wuhan University (Wuhan, China) between February 2017 and December 2019. Informed consents were signed by all patients, and this study was approved by the review board of Renmin Hospital of Wuhan University (Wuhan, China).
16S rRNA gene sequencing
Total genomic DNA were extracted from GC tissues and adjacent normal tissues from surgical resections using TIANamp Bacterial DNA Kit (Qiagen, Hilden, Germany). The 16S rRNA gene was amplified using primers 515F 5′-GTGCCAGCMGCCGCGG-3′ and 806R 5′-GGACTACHVGGGTWTCTAAT-3′targeting the V4 hypervariable regions and sequenced using Illumina’s MiSeq PE300 platform (Shanghai Majorbio Bio-pharm Technology Co., Ltd).
Cell culture
Human GC cell lines SGC-7901 and human monocyte THP-1 cell line were purchased from the Center for Type Culture Collection of Wuhan University (Wuhan, China) and cultured in RPMI-1640 medium supplemented with 2 mM L-glutamine and 10% fetal bovine serum (FBS) at 37 °C under 5% CO2. Macrophages were derived from THP-1 cells treated with 100 ng/mL phorbol 12-myristate 13-acetate (PMA) for 24 h, which was purchased from Sigma company (St. Louis, MO, United States) [16].
Bacteria culture and cell infection
Propionibacterium acnes (P. acnes) strain ATCC 6919 was purchased from American Type Culture Collection (ATCC) and cultured on Columbia blood agar plates under anaerobic conditions at 37 °C. Escherichia coli (E. coli) DH5α were cultured in Luria–Bertani broth using an orbital shaker incubator at 37 °C. GC cell lines and THP-1 derived macrophages were then stimulated with live P. acnes (MOI = 30) and E. coli DH5α (MOI = 1000), respectively.
Fluorescence in situ hybridization (FISH) analysis
Sections with 5-μm-thick from GC tissues and paired normal tissues were prepared and hybridized as described in our previous study [17]. The sequence of P. acnes specific 16S rRNA probe was 5′-GCCCCAAGATTACACTTCCG)-3′, and labeled with fluorescein isothiocyanate (FITC) [18]. Five random fields at 200 × magnification were captured from each sample using a microscope (BX53F; Olympus, Tokyo, Japan), and the number of bacteria per field was calculated by an observer blind to sample status.
Immunofluorescence
Immunofluorescence staining was conducted as in our previous study [19]. Paraffin-embedded 5-μm-thick sections were dewaxed and rehydrated. THP-1 derived macrophages on glass coverslips were fixed in 4% paraformaldehyde. Followed by blocking with 10% goat serum and incubated with primary antibodies, slides were then incubated with appropriate secondary antibodies. Subsequently, slides were incubated with DAPI (Beyotime, China) for nuclear counterstain. Fiver random fields at 400 × magnification were obtained from each sample using a microscope (BX53F; Olympus, Tokyo, Japan). The density of positive cells was evaluated and presented as the average number of positive cells per field.
Quantitative real‑time PCR (RT-qPCR)
Trizol reagent (Invitrogen, Carlsbad, CA, USA) was used for total RNA extraction. Reverse transcription was accomplished using a Reverse Transcription kit (Takara, Ohtsu, Japan). Quantitative real-time PCR was carried out using SYBR Green PCR Master Mix (Takara, Ohtsu, Japan) on a Biorad CFX96 Real-Time PCR Detection System. The relative expression values of different genes between samples were determined using the 2−∆∆Cq method. All primer sequences used were presented in Supplementary Table S1.
Cell counting Kit-8 (CCK8) assay
The proliferation of GC cells was evaluated using cell counting kit 8 (Dojundo, Kumamoto, Japan). The cells were seeded in 96-well plates at a density of 5000 cells per well, 3 replicate wells in each group were set. After different treatments, 100 μl 1640 medium supplemented with 10 μl CCK8 were added in each well. The plates were incubated at 37 ℃ for half an hour, and the absorbance at 450 nm was measured. All experiments were performed in triplicate.
Wound healing assay
GC cell lines (1.0 × 106 cells/well) were seeded in 6-well plates, a 200-μL pipette tip was used to create a scratch wound when a confluent monolayer had formed. Next, cells were washed with PBS and treated with P. acnes, E. coli DH5α, and condition medium (CM) from THP-1 derived macrophages and THP-1 derived macrophages treated with P. acnes and E. coli DH5α, respectively. Wound areas were observed and captured under an inverted microscope (Olympus, Tokyo, Japan), and measured by Image J software (National Institutes of Health, Bethesda, MD, United States).
Trans-well assay
GC cell lines were incubated with P. acnes, E. coli DH5α, and PBS for 24 h, respectively. Then cells were washed thrice with PBS and obtained by trypsinization [20]. A total of 2 × 104 cells were seeded in upper compartment of trans-well chambers (8 μm, Corning, USA) in serum-free media. The lower compartment was filled with medium supplemented with10% FBS. For GC cells treated with CMs from THP-1 derived macrophages stimulated with P. acnes and E. coli DH5α, 2 × 104 cells GC cells were seeded in the upper chamber, while the lower chamber filled with 20% CMs [21], respectively. Twenty-four hours later, cells on the lower side of filter were fixed with a fixative solution (acetic acid: methanol = 1:3) for 30 min and stained with 0.1% crystal violet for 15 min. Five random fields at 200 × magnification were obtained using an inverted microscope (Olympus, Tokyo, Japan) and quantified using Image J software (National Institutes of Health, Bethesda, MD, United States).
Western blotting assay
Total protein was extracted from harvested cells by RIPA protein lysate. Proteins were then separated by SDS–PAGE and transferred to polyvinylidene fluoride (PVDF) membranes. After blocking with 5% nonfat milk in TBST buffer, membranes were incubated with primary antibodies at 4 °C for 16 h. Then, membranes were incubated with appropriate HRP-conjugated secondary antibodies at room temperature for 1 h. The quantification of blot was performed using Quantity One 4.5.0 software (Bio-Rad Laboratories, CA).
Luminex liquid suspension chip detection
Luminex liquid suspension chip detection was employed to measure the cytokines in CM, and performed by Wayen Biotechnologies (Shanghai, China). The CM of THP1-derived macrophages challenged with or without P. acnes were measured by the Bio-Plex Pro Human Cytokine Grp I Panel 27-plex kit (#M500KCAF0Y). Briefly, the CM was added in 96-well plates embedded with microbeads and incubated for 30 min, followed by incubated with detection antibody for 30 min. Finally, values of each well were read using the Bio-Plex MAGPIX System (Bio-Rad) after incubating with streptavidin-PE for 10 min.
Statistical analysis
All analyses were performed using GraphPad Prism 8.0 (GraphPad Prism 8.0, GraphPad Software Inc., La Jolla, CA, USA). All data were presented as mean ± SD for quantitative data and proportions for categorical data. Student’s t test and one-way analysis of variance (ANOVA with Bonferroni correction) were applied for parametric variables analyzing, Chi-square test was used for analyzing clinicopathological features in different groups, and Kruskal–Wallis for nonparametric variables. It was considered statistically significant if P values < 0.05.
Results
Dysbiosis of mucosal microbiome was found in gastric cancer tissues
We performed 16S rRNA gene sequencing targeted V4 regions to assay microbial diversity and richness of mucosal samples from GC tissues and adjacent normal tissues. Dysbiosis was found in GC tissues compared with adjacent normal (NC) tissues. Compared with NC tissues, Simpson-estimated microbial diversity in GC tissues was decreased though the difference was not significant (Student’s t test, P = 0.1378, Fig. 1A). At the phylum level, the following bacteria ranked the top five abundance of GC tissues and NC tissues: Proteobacteria (56.47 vs. 51.27%), Firmicutes (20.34 vs. 22.66%), Bacteroidetes (5.41 vs. 6.82%), Actinobacteria (5.97 vs. 5.17%) and Acidobacteria (1.25 vs. 1.62%) (Fig. 1B). Student’s t test was applied to determine the differences of microbiota between GC and NC tissues at the species level (Fig. 1C), we found that Propionibacterium acnes, Novosphingobium, Methylobacterium fujisawaense, Lactobacillus oris, Microbacteriaceae, Comamonas aquatic, Corynebacterium tuberculostearicum, Trichococcus, Eubacterium sulci, Sphigomonadales, Nannochloropsis gaditana were significantly increased in GC tissues (all P value < 0.05, Fig. 1C). These results indicate that dysbiosis of mucosal microbiota occurred in patients with GC.
P. acnes was significantly increased in gastric cancer tissues. A Simpson diversity index was lower in GC tissues than in adjacent normal tissues, though the difference was not significant. B Relative abundance of the main bacteria at phylum level in GC and adjacent normal tissues from GC patients. C Bacterium that increased in GC tissues than adjacent normal tissues at the species level, P. acnes was the most significantly increased bacteria in GC tissues. D Relative abundance of the main bacteria at phylum level in GC and adjacent normal tissues of H. pylori-positive group. E Bacterium that increased in GC tissues than adjacent normal tissues at the species level of H. pylori-positive group. F Relative abundance of the main bacteria at phylum level in GC and adjacent normal tissues of H. pylori-negative group. G Bacterium that increased in GC tissues than adjacent normal tissues at the species level of H. pylori-negative group. H–K P. acnes was detected in tissue samples using fluorescence in situ hybridization (FISH). H, I The abundance of P. acnes significantly increased in GC tissues than adjacent normal tissues. J, K The abundance of P. acnes was higher in GC tissues from TNM III stage patients than that in TNM I and TNM II stage patients. *P < 0.05, **P < 0.01, ***P < 0.001. GC gastric cancer tissue NC adjacent normal tissue
Since several studies had distinguished different microbial communities in GC tissues with and without H. pylori infection, we also measured the effect of H. pylori infection on the microbial community composition in GC and NC tissues (Fig. 1D–G). Overall, the microbial community in H. pylori-positive tissues of GC and NC at phylum level and species level were shown in Fig. 1D and E. Next, the microbial communities in H. pylori-negative group of GC and NC tissues at phylum level were shown in Fig.1F. Besides, the abundance of Propionibacterium acnes, Comamonas aquatica, Enhydrobacter, and Sphingomonadales significantly increased in GC tissues, while Lachnoclostridium decreased (all P value < 0.05, Fig. 1G). These results may suggest that the gastric flora structure were different in tissues with and without H. pylori infection.
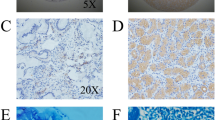
Propionibacterium acnes significantly increased in gastric cancer tissues and correlated with tumor progression
As we focused on the role of non-H. pylori bacteria in the progression of GC, we found that Propionibacterium acnes (P. acnes) significantly increased in GC tissues without considering H. pylori infection (P = 0.005957, Fig. 1C). In addition, P. acnes was also the most significant one among the bacteria that increased in H. pylori-negative GC tissues (P = 0.002321, Fig. 1G). Consequently, we next focused on exploring the role of P. acnes in the development of GC. Next, fluorescence in situ hybridization (FISH) was performed to confirm the distribution and abundance of P. acnes, specific probe targeted 16S rRNA of P. acnes was designed (green) (Fig. 1H–K). We observed a much higher abundance of P. acnes in GC tissues than adjacent normal tissues (P = 0.015, Fig. 1H, I). What’s more, a higher abundance of P. acnes was found in TNM stage III of GC tissues than in TNM stage I and II (all P < 0.0001, Fig. 1J, K). Clinicopathologic features of patients were shown in Supplementary Table S2, no significant differences were observed in patient age, sex, and differentiation among the different stages of GC. These results may indicate that P. acnes correlated with tumor progression of GC.
Macrophages are essential for the tumor-promoting effect of Propionibacterium acnes
To analyze the role of P. acnes in the development of GC, in vitro experiments were performed. E. coli DH5α was used as a bacterial control as described in previous studies [20, 22]. Cholecystokinin octapeptide (CCK8), wound healing assay, and trans-well were performed to analyze whether P. acnes could affect the proliferation and migration of GC cells. However, no significant difference was found among GC cells untreated and treated with P.acnes, E. coli DH5α at 6, 12, and 24 h (all P value > 0.05, Fig. 2A, B, D).
Macrophages are essential for the tumor-promoting effect of P. acnes. A Cholecystokinin octapeptide (CCK8) was used to assay the proliferation of SGC-7901. P. acnes or condition medium (CM) from P. acnes-primed macrophages did not affect the proliferation of SGC-7901. B–E Migration of SGC-7901 was investigated by wound healing assay. B, D P. acnes and E. coli DH5α did not affect the migration of SGC-7901 at 6, 12, and 24 h. C, E Migration of SGC-7901 significantly increased after stimulation with CM from P. acnes-primed macrophages at 12 and 24 h. F–J Migration of SGC-7901 was determined by trans-well assay. F, H Compared with the untreated group, the migration of SGC-7901 enhanced after directly stimulated with P. acnes and E. coli DH5α, while no difference was found between GC cells stimulated with P. acnes and E. coli DH5α. G, I Migration of SGC-7901 was determined after stimulation with CM from THP-1 derived macrophage (control), and CM from P. acnes and E. coli DH5α-primed macrophages. CM from P. acnes-primed macrophages greatly promoted migration of SGC-7901. J CM from P. acnes-primed macrophages greatly enhanced migration of SGC-7901 compared to P. acnes alone. ns, no significance; #P < 0.05 compared to untreated group; ##P < 0.01 compared to untreated group; ###P < 0.001 compared to untreated group; ★P < 0.05 compared to control group; ★★★P < 0.001 compared to control group. **P < 0.01. CM condition medium
Previous studies have shown that macrophages play a major role in triggering cancer progression under the situation of alterations in microbiota homeostasis [23, 24]. Therefore, we investigated whether P. acnes could contribute to the progression of GC by influencing macrophages. Next, condition medium (CM) was collected from THP-1 derived macrophages untreated and macrophages treated with P. acnes or E. coli DH5α. Proliferation and migration of GC cells (SGC-7901) were measured after incubating with these CMs. As shown in Fig. 2A, the proliferation of SGC-7901 did not change. Compared with the untreated group, CM from THP-1 derived macrophages with P. acnes stimulation greatly enhanced the migration of GC cells (P = 0.0014, Fig. 2C, E). Besides, CM from THP-1 derived macrophages with P. acnes stimulation greatly promote the migration of GC cells than CM from THP-1 derived macrophages with E. coli DH5α stimulation at 24 h (P = 0.0091, Fig. 2C, E). In addition, the trans-well assay was performed, CM from THP-1 derived macrophages with P. acnes stimulation greatly promote the migration of GC cells, while P. acnes stimulation could not, which were consistent with the above results (Fig. 2F–J).
Propionibacterium acnes promoted M2 polarization of macrophages
We next investigated the cytokines secreted by THP-1 derived macrophages treated with P. acnes by Luminex liquid suspension chip detection. As shown in Fig. 3A, a panel of cytokines was increased in condition medium of THP-1 derived macrophages challenged with P. acnes, when compared with condition medium of THP-1 derived macrophages. Among these increased cytokines, IL-6 and MIP-1β were identified to be the most two enriched cytokines that increased 584 and 508 times than control, respectively. Combined with the fact that IL-6 is a cytokine secreted by M2 macrophages and numerous evidence showed that M2 macrophage favors the progression of GC [13, 25], we next measured whether P. acnes could promote M2 polarization of macrophages. We collected GC samples and determined the infiltration of M2 macrophages (CD206 +) by immunofluorescence. Interestingly, a positive correlation was found between the abundance of P. acnes and numbers of M2 macrophage (r = 0.6359, P = 0.0002, Fig. 3B, C). This result may indicate that M2 macrophages play an essential role in the tumor-promoting effect of P. acnes.
P. acnes promoted M2 polarization of macrophages. A Fold changes of cytokines in condition medium from THP-1 derived macrophage treated with P. acnes (P. acnes) compared with condition medium in THP-1 derived macrophage (Control). B CD206 + (M2) macrophages were measured by immunofluorescence in gastric cancer tissues. Scale bar, 20 μm. C A positive correlation was found between the abundance of M2 macrophages and P. acnes (r = 0.6359, P = 0.0002). D–G Polarization of THP-1 derived macrophages was measured by immunofluorescence. Scale bar, 20 μm. E, F M1 polarized macrophage was defined as CD86 + macrophages, E. coli DH5α mainly promoted M1 polarization of macrophages. D, G M2 polarized macrophage was defined as CD206 + macrophages, P. acnes mainly promoted M2 polarization of macrophages. H Messenger RNA levels of cytokines secreted by M1 and M2 macrophages were measured by RT-qPCR. IL-10 and CCR-2 were significantly increased in THP-1 derived macrophages challenged with P. acnes, while IL-8 decreased. Besides, the mRNA level of iNOS did not change significantly when stimulated with P. acnes. *P < 0.05, **P < 0.01, ***P < 0.001
To assess the effect of P. acnes on the polarization of macrophages, we performed immunofluorescence staining to measure the marker of M1 (CD86 +) and M2 (CD206 +) phenotype macrophages after THP-1 derived macrophages treated with P. acnes and E. coli DH5α (Fig. 3D–G). CD206 + cells were much higher in macrophages stimulated with P. acnes than that in the E. coli DH5α group at 2, 6, 12, and 24 h, while more CD86 + cells were found in macrophages treated with E. coli DH5α (all P values < 0.05, Fig. E, G). Next, the M1 macrophage markers (IL-8, iNOS) and M2 macrophage markers (CCR-2, IL-10) were analyzed by RT-qPCR [21, 26, 27]. Compared with macrophages treated E. coli DH5α, significantly higher levels of CCR-2 and IL-10 were observed in macrophages treated with P. acnes at 6 h and 12 h (all P values < 0.05, Fig. 3H), while lower levels of IL-8 was found in macrophages treated with P. acnes at 12 h (P < 0.001, Fig. 3H). Besides, the mRNA level of iNOS did not significantly different between macrophages treated with P. acnes and E. coli DH5α (P > 0.05, Fig. 3H). These results indicated that the M2 polarization of macrophages was promoted by P. acnes.
Propionibacterium acnes promote M2 polarization of macrophage via TLR4-dependent way
Since toll-like receptor (TLR) signaling is required for anti-pathogen responses in macrophages [28], we next analyzed several expressions of TLRs that reside at the plasma membrane in P. acnes-stimulated macrophages. We only found that TLR4 elevated in a time-dependent manner at mRNA level and peaked at 6 h (P < 0.05, Fig. 4A), while other TLRs did not change significantly (P > 0.05, Fig. 4A).
P. acnes promoted M2 polarization of macrophages via TLR4 dependent signaling. A Toll-like receptors (TLRs) in THP-1 derived macrophages challenged with P. acnes were analyzed by RT-qPCR, in which TLR4 changed obviously. B–D Using immunofluorescence, reduced M2 polarization was found in P. acnes-primed macrophages pretreated with TAK-242 (an inhibitor of TLR4). Scale bar, 20 μm. C Number of CD206 + (M2) macrophages decreased in P. acnes-primed macrophages pretreated with TAK-242. D Number of CD86 + (M1) macrophages increased in P. acnes-primed macrophages pretreated with TAK-242. E Using RT-qPCR, mRNA levels of IL-10 and CCR-2 were found to be reduced in P. acnes-primed macrophages pretreated with TAK-242, while IL-8 significantly increased. F, G Co-localization of TLR4 and CD206 was performed in GC tissues with high and low abundance of P. acnes using immunofluorescence. Higher numbers of M2 macrophages that expressed TLR4 were detected in GC tissues with a high abundance of P. acnes than that in GC tissues with a low abundance of P. acnes. The high abundance of P. acnes was defined as the abundance of P. acnes higher than the median, while the low abundance of P. acnes was defined as the abundance of P. acnes lower than the median. ns, no significance; *P < 0.05, **P < 0.01, ***P < 0.001
We next analyzed macrophage polarization after macrophage pretreated with TLR4 inhibitor (TAK-242) for 1 h and followed by P. acnes treatment by immunofluorescence. Since TLR4 peaked at 6 h at mRNA level, we analyzed the polarization of macrophages at 6 and 12 h (Fig. 4B). The relative abundance of M2 (CD206 +) macrophage was decreased at 12 h in TAK-242 pretreatment group (P = 0.0166, Fig. 4C), while the relative abundance of M1 (CD86 +) macrophage was increased (P = 0.0016, Fig. 4D). What’s more, IL-10 and CCR-2, the cytokine produced by M2 macrophages, was also measured by RT-qPCR, we found that mRNA levels of IL-10 and CCR-2 significantly decreased after TAK-242 pretreatment at 6 and 12 h (all P value < 0.01, Fig. 4E). Besides, IL-8 secreted by M1 macrophages was greatly enhanced after TAK-242 blockade (all P value < 0.01, Fig. 4E). Moreover, co-localization of CD206 and TLR4 was performed using immunofluorescence (Fig. 4F), higher numbers of macrophages that expressed both CD206 and TLR4 were found in GC tissues with the high abundance of P. acnes compared with that with low abundance of P. acnes (P < 0.05, Fig. 4G). These results indicated that P. acnes promoted the M2 polarization of macrophages via TLR4 signaling.
Propionibacterium acnes promote M2 polarization of macrophage via TLR4/PI3K/Akt signaling
Early work identified that PI3K-Akt signaling induced by TLRs contributed to the production of IL-10 [29]. Since we found that IL-10 production, a marker of M2 macrophage, in THP-1 derived macrophages significantly increased after P. acnes stimulation, we wonder whether M2 polarization induced by P. acnes could be regulated by PI3K/Akt signaling. THP-1 derived macrophages were pretreated with LY294002 at 10 μM for 30 min to blockade PI3K, and then stimulated with P. acnes. Immunofluorescence was performed to analyze the polarization of THP-1 derived macrophages treated with P. acnes (Fig. 5A), we found that M2 polarization was attenuated, while M1 polarization was enhanced after PI3K blocking (P < 0.05, P < 0.01, respectively. Figure 5B, C). In addition, IL-10 and CCR-2 production were inhibited at the mRNA level (Fig. 5D). These results indicated that M2 polarization induced by P. acnes could be regulated by PI3K/Akt signaling.
P. acnes promote M2 polarization of macrophages through TLR4/PI3K/Akt signaling. A–C Immunofluorescence was performed to analyze the polarization of P. acnes primed macrophages after PI3K blockade by LY294002. Scale bar, 20 μm. B Number of CD206 + (M2) macrophages decreased at 12 h in P. acnes-primed macrophages pretreated with LY294002. C Number of CD86 + (M1) macrophages increased in P. acnes-primed macrophages pretreated with LY294002. D mRNA levels of IL-10 and CCR-2 were significantly reduced after PI3K blockade. E Expression of TLR4, PI3K, p-Akt, and Akt was analyzed by western blotting assays. F Expression of PI3K and p-Akt increased in THP-1 derived macrophages stimulated with P. acnes. G The expression of PI3K and p-Akt decreased in P. acnes-primed macrophages pretreated with TAK-242. ns no significance; *P < 0.05, **P < 0.01, ***P < 0.001
Since a previous study demonstrated PI3K/Akt signaling could be induced by TLRs [29], we wonder whether PI3K/Akt signaling could be activated by TLR4. As shown in Fig. 5E, the expression of TLR4, PI3K, and p-Akt increased at 24 h, while the expression of Akt did not change (all P value < 0.05, Fig. 5F). After blocking with TAK-242, the inhibitor of TLR4, the expression of PI3K and p-Akt reduced (figure all P value < 0.05, 5E, 5G). Together, these results indicated that M2 polarization could be regulated by TLR4/PI3K/Akt signaling.
Discussion
The pathogenesis of GC has long been investigated. However, the treatment that targeting of H. pylori is still unsatisfactory. It was generally accepted that most bacteria cannot survive in the stomach due to the acid environment. However, many factors, including H. pylori infection and the use of drugs such as proton pump inhibitor, could lead to peptic acid secretion decreased, which contribute to alterations of gastric microbiota [30]. These researches raise an intriguing hypothesis that non-H. pylori bacteria could influence the risk for GC. Subsequently, later studies have shown that non-H. pylori bacteria colonization in the stomach can also stimulate GC risk [31]. In addition, studies have gradually realized that with the progress of GC, the abundance of H. pylori gradually decreased [11]. We also demonstrated that the abundance of H. pylori in GC tissues was lower than that in normal tissues. Therefore, we put forward our hypothesis for the first time that H. pylori may not participate in the whole progression of GC. Non-H. pylori bacteria may participate in the progression of GC after the bacterial disturbance caused by H. pylori. Therefore, in view of different stages, we should probably adopt different treatment measures instead of only targeted H. pylori.
In the current study, by comparing microbial community profiling in GC and adjacent normal tissues, we found an overabundance of P. acnes in GC tissues. Moreover, the abundance of P. acnes was positively correlated with M2 macrophages in GC tissues and confirmed that P. acnes could promote M2 polarization of macrophages through TLR4/PI3K/Akt signaling in vitro. Nowadays, the role of non-H. pylori bacterium in the progression of GC has attracted more and more attention of scientists [32, 33]. In our study, we found that the abundance of P. acnes greatly increased in H. pylori-negative GC tissues and had a tumor-promoted effect. Together, our results highlighted for the first time that P. acnes play an essential role in the progression of GC, especially in H. pylori-negative GC.
P. acnes is a kind of gram-positive, anaerobic bacteria, which is widely colonized in human skin [34], while recent studies identified that P. acnes could be present in the stomach [35]. Besides, it was found in mucosal specimens of stomach rather than gastric fluid [36]. A recent study detected that P. acnes promoted lymphocytic gastritis via the NKG2D system and IL-15 activation [37]. Another study detected that the risk of GC increased in individuals with a high relative abundance of P. acnes [38]. In our study, P. acnes was demonstrated to be highly increased in GC tissues compared with adjacent normal tissues. Using 16S rDNA sequencing, P. acnes was also demonstrated to be significantly increased in GC tissues in a previous study [11]. It is important to note that these studies only identified changes of microbes in stomach and in-depth studies on the effects of these organisms have not been performed.
P. acnes had been shown to be associated with prostate cancer [39], indicating that P. acnes may has a potential to promote tumorigenesis. In our study, we found that P. acnes was also related to the progression of GC. Adhesive Flp pili encoded by a gene locus for tight adherence (tad) can facilitate P. acnes colonization in prostate tissue [40]. Therefore, the increased P. acnes in GC may also be favored by this pili. However, this needs to be investigated in future study. Since numerous studies proved that microbiota could promote cancer progression via suppressing anti-tumor immunity [41], we also demonstrated that P. acnes abundance was positively correlated with numbers of M2 macrophages in GC tissues. Clinical and experimental evidence has proved that M2 macrophages have the ability to promote cancer initiation and malignant progression [42]. Next, we proved that macrophages treated with P. acnes presented M2 phenotype in vitro, which indicated that P. acnes favored the progression of GC via promoting M2 polarization of macrophages.
Toll-like receptors (TLRs) are immune sentries that are expressed on many cell types, which could sense pathogen-associated molecular patterns (PAMPs) derived from microbiota [43]. Bacterial ligands from Gram-positive bacteria have been identified that can activate monocytes via TLR2 or TLR4 [44]. A Previous study also demonstrated that imbalance of intestinal bacteria could promote macrophage M2 polarization through activating TLR4 in colon cancer [24]. In our study, we demonstrated that P. acnes could promote M2 polarization of macrophages via a TLR4 dependent way. TLR4 has been found strongly expressed in GC tissues [45], besides, high expression of TLR4 correlated with poor prognosis of GC [46]. We also found that TLR4 was highly expressed in GC tissues by immunofluorescence, co-localization of TLR4 and M2 macrophages showed that TLR4 was highly expressed in most M2 macrophages, which may suggest that TLR4 signaling activation in M2 macrophages may play a prominent role in the progression of GC. Moreover, in colon cancer, the polarization of M2 macrophage has been demonstrated to be promoted by PI3K/Akt pathway [47]. In our study, we also found that M2 polarization could be enhanced through PI3K/Akt pathway, which could be regulated by TLR4 activation.
M2 polarization of macrophages in tumors has been reported in numerous studies, which could be driven by canonical M2 stimuli, such as IL-4, IL-10, and IL-13 [48]. In our study, we found that IL-10 expression at mRNA level was greatly enhanced in macrophages stimulated with P. acnes, while it was decreased after TAK-242 blockade. We may infer that M2 polarization could be driven by self-secreted IL-10, which may contain a positive-feedback loop. However, this hypothesis needs to be proved in future studies.
In conclusion, we demonstrated that P. acnes was abundant in GC tissues and contribute to GC via promoting M2 polarization of macrophages through TLR4/PI3K/Akt signaling. Our finding may suggest that bacteria other than H. pylori also play an essential role in progression of GC. P. acnes, for example, could regulate the tumor microenvironment by enhancing immunosuppression and thus promote the progress of GC. In addition, as for the prevention and treatment of GC, we could take different treatment measures at different stages, so as to enhance the therapeutic effect.
Change history
10 September 2022
A Correction to this paper has been published: https://doi.org/10.1007/s10120-022-01339-0
References
Corso S, Isella C, Bellomo SE, Apicella M, Durando S, Migliore C, et al. A comprehensive PDX gastric cancer collection captures cancer cell intrinsic transcriptional MSI traits. Cancer Res. 2019;79(22):5884–96.
Williams C, McColl KE. Review article: proton pump inhibitors and bacterial overgrowth. Aliment Pharmacol Ther. 2006;23(1):3–10.
Noto JM, Zackular JP, Varga MG, Delgado A, Romero-Gallo J, Scholz MB, et al. Modification of the gastric mucosal microbiota by a strain-specific Helicobacter pylori Oncoprotein and Carcinogenic histologic phenotype. MBio. 2019;10(3):e00955.
Wong BC, Lam SK, Wong WM, Chen JS, Zheng TT, Feng RE, et al. Helicobacter pylori eradication to prevent gastric cancer in a high-risk region of China: a randomized controlled trial. JAMA. 2004;291(2):187–94.
Miwa H, Go MF, Sato N. H. pylori and gastric cancer: the Asian enigma. Am J Gastroenterol. 2002;97(5):1106–12.
Lee CW, Rickman B, Rogers AB, Ge Z, Wang TC, Fox JG. Helicobacter pylori eradication prevents progression of gastric cancer in hypergastrinemic INS-GAS mice. Cancer Res. 2008;68(9):3540–8.
Lofgren JL, Whary MT, Ge Z, Muthupalani S, Taylor NS, Mobley M, et al. Lack of commensal flora in Helicobacter pylori-infected INS-GAS mice reduces gastritis and delays intraepithelial neoplasia. Gastroenterology. 2011;140(1):210–20.
Lertpiriyapong K, Whary MT, Muthupalani S, Lofgren JL, Gamazon ER, Feng Y, et al. Gastric colonisation with a restricted commensal microbiota replicates the promotion of neoplastic lesions by diverse intestinal microbiota in the Helicobacter pylori INS-GAS mouse model of gastric carcinogenesis. Gut. 2014;63(1):54–63.
Aviles-Jimenez F, Vazquez-Jimenez F, Medrano-Guzman R, Mantilla A, Torres J. Stomach microbiota composition varies between patients with non-atrophic gastritis and patients with intestinal type of gastric cancer. Sci Rep. 2014;4:4202.
Ferreira RM, Pereira-Marques J, Pinto-Ribeiro I, Costa JL, Carneiro F, Machado JC, et al. Gastric microbial community profiling reveals a dysbiotic cancer-associated microbiota. Gut. 2018;67(2):226–36.
Liu X, Shao L, Liu X, Ji F, Mei Y, Cheng Y, et al. Alterations of gastric mucosal microbiota across different stomach microhabitats in a cohort of 276 patients with gastric cancer. EBioMedicine. 2019;40:336–48.
Liu L, Liang L, Liang H, Wang M, Lu B, Xue M, et al. Fusobacterium nucleatum Aggravates the Progression of Colitis by Regulating M1 Macrophage Polarization via AKT2 Pathway. Front Immunol. 2019;10:1324.
Zhou Z, Xia G, Xiang Z, Liu M, Wei Z, Yan J, et al. A C-X-C Chemokine Receptor Type 2-Dominated Cross-talk between Tumor Cells and Macrophages Drives Gastric Cancer Metastasis. Clin Cancer Res. 2019;25(11):3317–28.
Huang X, Pan Y, Ma J, Kang Z, Xu X, Zhu Y, et al. Prognostic significance of the infiltration of CD163(+) macrophages combined with CD66b(+) neutrophils in gastric cancer. Cancer Med. 2018;7(5):1731–41.
Gambardella V, Castillo J, Tarazona N, Gimeno-Valiente F, Martinez-Ciarpaglini C, Cabeza-Segura M, et al. The role of tumor-associated macrophages in gastric cancer development and their potential as a therapeutic target. Cancer Treat Rev. 2020;86:102015.
Yoon J, Um HN, Jang J, Bae YA, Park WJ, Kim HJ, et al. Eosinophil activation by toll-like receptor 4 Ligands regulates Macrophage polarization. Front Cell Dev Biol. 2019;7:329.
Yu J, Chen Y, Fu X, Zhou X, Peng Y, Shi L, et al. Invasive Fusobacterium nucleatum may play a role in the carcinogenesis of proximal colon cancer through the serrated neoplasia pathway. Int J Cancer. 2016;139(6):1318–26.
Capoor MN, Ruzicka F, Schmitz JE, James GA, Machackova T, Jancalek R, et al. Propionibacterium acnes biofilm is present in intervertebral discs of patients undergoing microdiscectomy. PLoS One. 2017;12(4):e0174518.
Chen T, Li Q, Wu J, Wu Y, Peng W, Li H, et al. Fusobacterium nucleatum promotes M2 polarization of macrophages in the microenvironment of colorectal tumours via a TLR4-dependent mechanism. Cancer Immunol Immunother. 2018;67(10):1635–46.
Yang Y, Weng W, Peng J, Hong L, Yang L, Toiyama Y, et al. Fusobacterium nucleatum increases proliferation of colorectal cancer cells and tumor development in mice by activating toll-like receptor 4 signaling to nuclear factor-kappaB, and up-regulating expression of MicroRNA-21. Gastroenterology. 2017;152(4):851-866 e24.
Li W, Zhang X, Wu F, Zhou Y, Bao Z, Li H, et al. Gastric cancer-derived mesenchymal stromal cells trigger M2 macrophage polarization that promotes metastasis and EMT in gastric cancer. Cell Death Dis. 2019;10(12):918.
Toller IM, Neelsen KJ, Steger M, Hartung ML, Hottiger MO, Stucki M, et al. Carcinogenic bacterial pathogen Helicobacter pylori triggers DNA double-strand breaks and a DNA damage response in its host cells. Proc Natl Acad Sci U S A. 2011;108(36):14944–9.
Yang Y, Li L, Xu C, Wang Y, Wang Z, Chen M et al. Cross-talk between the gut microbiota and monocyte-like macrophages mediates an inflammatory response to promote colitis-associated tumourigenesis. Gut. 2020 https://doi.org/10.1136/gutjnl-2020-320777
Li R, Zhou R, Wang H, Li W, Pan M, Yao X, et al. Gut microbiota-stimulated cathepsin K secretion mediates TLR4-dependent M2 macrophage polarization and promotes tumor metastasis in colorectal cancer. Cell Death Differ. 2019;26(11):2447–63.
Wang YC, Wu YS, Hung CY, Wang SA, Young MJ, Hsu TI, et al. USP24 induces IL-6 in tumor-associated microenvironment by stabilizing p300 and beta-TrCP and promotes cancer malignancy. Nat Commun. 2018;9(1):3996.
Wu J, Li K, Peng W, Li H, Li Q, Wang X, et al. Autoinducer-2 of Fusobacterium nucleatum promotes macrophage M1 polarization via TNFSF9/IL-1beta signaling. Int Immunopharmacol. 2019;74:105724.
Lumeng CN, Bodzin JL, Saltiel AR. Obesity induces a phenotypic switch in adipose tissue macrophage polarization. J Clin Invest. 2007;117(1):175–84.
El Kasmi KC, Qualls JE, Pesce JT, Smith AM, Thompson RW, Henao-Tamayo M, et al. Toll-like receptor-induced arginase 1 in macrophages thwarts effective immunity against intracellular pathogens. Nat Immunol. 2008;9(12):1399–406.
Antoniv TT, Ivashkiv LB. Interleukin-10-induced gene expression and suppressive function are selectively modulated by the PI3K-Akt-GSK3 pathway. Immunology. 2011;132(4):567–77.
Li Q, Yu H. The role of non-H. pylori bacteria in the development of gastric cancer. Am J Cancer Res. 2020;10(8):2271–81.
Li J, Perez Perez GI. Is there a role for the non-H. pylori bacteria in the risk of developing gastric cancer? Int J Mol Sci. 2018;19(5):1353.
Schulz C, Schutte K, Mayerle J, Malfertheiner P. The role of the gastric bacterial microbiome in gastric cancer: Helicobacter pylori and beyond. Therap Adv Gastroenterol. 2019;12:1756284819894062.
Brawner KM, Morrow CD, Smith PD. Gastric microbiome and gastric cancer. Cancer J. 2014;20(3):211–6.
Capoor MN, Birkenmaier C, Wang JC, McDowell A, Ahmed FS, Bruggemann H, et al. A review of microscopy-based evidence for the association of Propionibacterium acnes biofilms in degenerative disc disease and other diseased human tissue. Eur Spine J. 2019;28(12):2951–71.
Delgado S, Cabrera-Rubio R, Mira A, Suarez A, Mayo B. Microbiological survey of the human gastric ecosystem using culturing and pyrosequencing methods. Microb Ecol. 2013;65(3):763–72.
von Rosenvinge EC, Song Y, White JR, Maddox C, Blanchard T, Fricke WF. Immune status, antibiotic medication and pH are associated with changes in the stomach fluid microbiota. ISME J. 2013;7(7):1354–66.
Montalban-Arques A, Wurm P, Trajanoski S, Schauer S, Kienesberger S, Halwachs B, et al. Propionibacterium acnes overabundance and natural killer group 2 member D system activation in corpus-dominant lymphocytic gastritis. J Pathol. 2016;240(4):425–36.
Gunathilake MN, Lee J, Choi IJ, Kim YI, Ahn Y, Park C, et al. Association between the relative abundance of gastric microbiota and the risk of gastric cancer: a case-control study. Sci Rep. 2019;9(1):13589.
Davidsson S, Carlsson J, Mölling P, Gashi N, Andrén O, Andersson S-O, et al. Prevalence of Flp pili-encoding plasmids in Cutibacterium acnes isolates obtained from prostatic tissue. Front Microbiol. 2017;8:2241.
Davidsson S, Carlsson J, Molling P, Gashi N, Andren O, Andersson SO, et al. Prevalence of Flp Pili-encoding plasmids in Cutibacterium acnes isolates obtained from prostatic tissue. Front Microbiol. 2017;8:2241.
Wu J, Li Q, Fu X. Fusobacterium nucleatum contributes to the Carcinogenesis of colorectal cancer by inducing inflammation and suppressing host immunity. Transl Oncol. 2019;12(6):846–51.
Qian BZ, Pollard JW. Macrophage diversity enhances tumor progression and metastasis. Cell. 2010;141(1):39–51.
Lim KH, Staudt LM. Toll-like receptor signaling. Cold Spring Harb Perspect Biol. 2013;5(1):a011247.
Takeuchi O, Hoshino K, Kawai T, Sanjo H, Takada H, Ogawa T, et al. Differential roles of TLR2 and TLR4 in recognition of gram-negative and gram-positive bacterial cell wall components. Immunity. 1999;11(4):443–51.
Schmausser B, Andrulis M, Endrich S, Muller-Hermelink HK, Eck M. Toll-like receptors TLR4, TLR5 and TLR9 on gastric carcinoma cells: an implication for interaction with Helicobacter pylori. Int J Med Microbiol. 2005;295(3):179–85.
He B, Xu T, Pan B, Pan Y, Wang X, Dong J, et al. Polymorphisms of TGFBR1, TLR4 are associated with prognosis of gastric cancer in a Chinese population. Cancer Cell Int. 2018;18:191.
Lian G, Chen S, Ouyang M, Li F, Chen L, Yang J. Colon cancer cell secretes EGF to promote M2 polarization of TAM through EGFR/PI3K/AKT/mTOR pathway. Technol Cancer Res Treat. 2019;18:1533033819849068.
Wang N, Liang H, Zen K. Molecular mechanisms that influence the macrophage m1–m2 polarization balance. Front Immunol. 2014;5:614.
Acknowledgements
This study was supported by the National Natural Science Foundation of China (grant number 81672387).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no conflict of interest.
Ethical approval
All participants were given informed consent before sample collection. All procedures were approved by the review board of Renmin Hospital of Wuhan University (Wuhan, China) (No.WDRY2020-K221).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, Q., Wu, W., Gong, D. et al. Propionibacterium acnes overabundance in gastric cancer promote M2 polarization of macrophages via a TLR4/PI3K/Akt signaling. Gastric Cancer 24, 1242–1253 (2021). https://doi.org/10.1007/s10120-021-01202-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-021-01202-8