Abstract
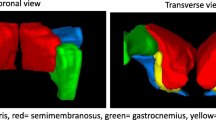
Currently, there is no large animal model of sustained limb ischemia suitable for testing novel angiogenic therapeutics for peripheral artery disease (PAD) such as drugs, genes, materials, or cells. We created a large animal model suitable for efficacy assessment of these therapies by testing 3 swine hind limb ischemia (HLI) variations and quantifying vascular perfusion, muscle histology, and limb function. Ligation of the ipsilateral external and bilateral internal iliac arteries produced sustained gait dysfunction compared to isolated external iliac or unilateral external and internal iliac artery ligations. Hyperemia-dependent muscle perfusion deficits, depressed limb blood pressure, arteriogenesis, muscle atrophy, and microscopic myopathy were quantifiable in ischemic limbs 6 weeks post-ligation. Porcine mesenchymal stromal cells (MSCs) engineered to express a reporter gene were visualized post-administration via positron emission tomography (PET) in vivo. These results establish a preclinical platform enabling better optimization of PAD therapies, including cellular therapeutics, increasing bench-to-bedside translational success.
Graphical abstract

A preclinical platform for porcine studies of peripheral artery disease therapies including (1) a hind limb ischemia model and (2) non-invasive MSC viability and retention assessment via PET






Similar content being viewed by others
Abbreviations
- ABI:
-
Ankle-brachial index
- CT:
-
Computed tomography
- EIA:
-
External iliac artery
- FBS:
-
Fetal bovine serum
- 18F-MFBG:
-
18F-meta-fluorobenzylguanidine
- GH:
-
Growth hormone
- hNET:
-
Human norepinephrine transporter
- IGF-1:
-
Insulin-like growth factor 1
- IIA:
-
Internal iliac artery
- mGFP:
-
mTag green fluorescent protein
- MSC:
-
Mesenchymal stromal cell
- MRI:
-
Magnetic resonance imaging
- PAD:
-
Peripheral artery disease
- PBS:
-
Phosphate-buffered saline
- PET:
-
Positron emission tomography
- TOF MRA:
-
Time-of-flight magnetic resonance angiography
- HLI :
-
Hind limb ischemia
References
Hamburg, N. M., & Creager, M. A. (2017). Pathophysiology of intermittent claudication in peripheral artery disease. Circulation Journal, 81(3), 281–289. https://doi.org/10.1253/circj.CJ-16-1286.
Pipinos, I. I., Judge, A. R., Selsby, J. T., Zhu, Z., Swanson, S. A., Nella, A. A., et al. (2007). The myopathy of peripheral arterial occlusive disease: part 1. Functional and histomorphological changes and evidence for mitochondrial dysfunction. Vascular and Endovascular Surgery, 41(6), 481–489. https://doi.org/10.1177/1538574407311106.
Suzuki, J., Shimamura, M., Suda, H., Wakayama, K., Kumagai, H., Ikeda, Y., et al. (2016). Current therapies and investigational drugs for peripheral arterial disease. Hypertension Research, 39(4), 183–191. https://doi.org/10.1038/hr.2015.134.
Gerhard-Herman, M. D., Gornik, H. L., Barrett, C., Barshes, N. R., Corriere, M. A., Drachman, D. E., et al. (2017). 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation, 135(12), e686–e725. https://doi.org/10.1161/cir.0000000000000470.
Cooke, J. P., & Chen, Z. (2015). A compendium on peripheral arterial disease. Circulation Research, 116(9), 1505–1508. https://doi.org/10.1161/circresaha.115.306403.
Jones, W. S., Dolor, R. J., Hasselblad, V., Vemulapalli, S., Subherwal, S., Schmit, K., et al. (2014). Comparative effectiveness of endovascular and surgical revascularization for patients with peripheral artery disease and critical limb ischemia: systematic review of revascularization in critical limb ischemia. American Heart Journal, 167(4), 489–498.e487. https://doi.org/10.1016/j.ahj.2013.12.012.
Cooke, J. P., & Losordo, D. W. (2015). Modulating the vascular response to limb ischemia: angiogenic and cell therapies. Circulation Research, 116(9), 1561–1578. https://doi.org/10.1161/circresaha.115.303565.
USFDA (2010). Guidance for industry: cellular therapy for cardiac disease. In U.S. D.o.H.a.H. Services (Ed.). Rockville, .
Waters, R. E., Terjung, R. L., Peters, K. G., & Annex, B. H. (2004). Preclinical models of human peripheral arterial occlusive disease: implications for investigation of therapeutic agents. Journal of Applied Physiology (Bethesda, MD: 1985), 97(2), 773–780. https://doi.org/10.1152/japplphysiol.00107.2004.
Hassanshahi, M., Khabbazi, S., Peymanfar, Y., Hassanshahi, A., Hosseini-Khah, Z., Su, Y. W., et al. (2019). Critical limb ischemia: current and novel therapeutic strategies. Journal of Cellular Physiology. https://doi.org/10.1002/jcp.28141.
Qadura, M., Terenzi, D. C., Verma, S., Al-Omran, M., & Hess, D. A. (2018). Concise review: cell therapy for critical limb ischemia: an integrated review of preclinical and clinical studies. Stem Cells, 36(2), 161–171. https://doi.org/10.1002/stem.2751.
Teraa, M., Sprengers, R. W., Schutgens, R. E., Slaper-Cortenbach, I. C., van der Graaf, Y., Algra, A., et al. (2015). Effect of repetitive intra-arterial infusion of bone marrow mononuclear cells in patients with no-option limb ischemia: the randomized, double-blind, placebo-controlled Rejuvenating Endothelial Progenitor Cells via Transcutaneous Intra-arterial Supplementation (JUVENTAS) trial. Circulation, 131(10), 851–860. https://doi.org/10.1161/circulationaha.114.012913.
Perin, E. C., Murphy, M. P., March, K. L., Bolli, R., Loughran, J., Yang, P. C., et al. (2017). Evaluation of cell therapy on exercise performance and limb perfusion in peripheral artery disease: the CCTRN Patients with Intermittent Claudication Injected with ALDH Bright Cells (PACE) trial. Circulation. https://doi.org/10.1161/circulationaha.116.025707.
Belch, J., Hiatt, W. R., Baumgartner, I., Driver, I. V., Nikol, S., Norgren, L., et al. (2011). Effect of fibroblast growth factor NV1FGF on amputation and death: a randomised placebo-controlled trial of gene therapy in critical limb ischaemia. The Lancet, 377(9781), 1929–1937. https://doi.org/10.1016/S0140-6736(11)60394-2.
Creager, M. A., Olin, J. W., Belch, J. J., Moneta, G. L., Henry, T. D., Rajagopalan, S., et al. (2011). Effect of hypoxia-inducible factor-1alpha gene therapy on walking performance in patients with intermittent claudication. Circulation, 124(16), 1765–1773. https://doi.org/10.1161/circulationaha.110.009407.
Poole, J., Mavromatis, K., Binongo, J. N., Khan, A., Li, Q., Khayata, M., et al. (2013). Effect of progenitor cell mobilization with granulocyte-macrophage colony-stimulating factor in patients with peripheral artery disease: a randomized clinical trial. JAMA, 310(24), 2631–2639. https://doi.org/10.1001/jama.2013.282540.
Yoshida, M., Horimoto, H., Mieno, S., Nomura, Y., Okawa, H., Nakahara, K., et al. (2003). Intra-arterial bone marrow cell transplantation induces angiogenesis in rat hindlimb ischemia. European Surgical Research, 35(2), 86–91. https://doi.org/10.1159/000069401.
Caron, A., Michelet, S., Caron, A., Sordello, S., Ivanov, M. A., Delaere, P., et al. (2004). Human FGF-1 gene transfer promotes the formation of collateral vessels and arterioles in ischemic muscles of hypercholesterolemic hamsters. The Journal of Gene Medicine, 6(9), 1033–1045. https://doi.org/10.1002/jgm.594.
Tompkins, B. A., Balkan, W., Winkler, J., Gyongyosi, M., Goliasch, G., Fernandez-Aviles, F., et al. (2018). Preclinical studies of stem cell rherapy for heart disease. Circulation Research, 122(7), 1006–1020. https://doi.org/10.1161/circresaha.117.312486.
Harding, J., Roberts, R. M., & Mirochnitchenko, O. (2013). Large animal models for stem cell therapy. Stem Cell Research & Therapy, 4(2), 23. https://doi.org/10.1186/scrt171.
Long, C. A., Timmins, L. H., Koutakis, P., Goodchild, T. T., Lefer, D. J., Pipinos, I. I., et al. (2016). An endovascular model of ischemic myopathy from peripheral arterial disease. Journal of Vascular Surgery. https://doi.org/10.1016/j.jvs.2016.07.127.
Burkhardt, G. E., Gifford, S. M., Propper, B., Spencer, J. R., Williams, K., Jones, L., et al. (2011). The impact of ischemic intervals on neuromuscular recovery in a porcine (Sus scrofa) survival model of extremity vascular injury. Journal of Vascular Surgery, 53(1), 165–173. https://doi.org/10.1016/j.jvs.2010.07.012.
Grundmann, S., Hoefer, I., Ulusans, S., Bode, C., Oesterle, S., Tijssen, J. G., et al. (2006). Granulocyte-macrophage colony-stimulating factor stimulates arteriogenesis in a pig model of peripheral artery disease using clinically applicable infusion pumps. Journal of Vascular Surgery, 43(6), 1263–1269. https://doi.org/10.1016/j.jvs.2006.02.049.
Voskuil, M., van Royen, N., Hoefer, I. E., Seidler, R., Guth, B. D., Bode, C., et al. (2003). Modulation of collateral artery growth in a porcine hindlimb ligation model using MCP-1. American Journal of Physiology - Heart and Circulatory Physiology, 284(4), H1422–H1428. https://doi.org/10.1152/ajpheart.00506.2002.
Muhs, A., Lenter, M. C., Seidler, R. W., Zweigerdt, R., Kirchengast, M., Weser, R., et al. (2004). Nonviral monocyte chemoattractant protein-1 gene transfer improves arteriogenesis after femoral artery occlusion. Gene Therapy, 11(23), 1685–1693.
Stacy, M. R., Yu, D. Y., Maxfield, M. W., Jaba, I. M., Jozwik, B. P., Zhuang, Z. W., et al. (2014). Multimodality imaging approach for serial assessment of regional changes in lower extremity arteriogenesis and tissue perfusion in a porcine model of peripheral arterial disease. Circulation. Cardiovascular Imaging, 7(1), 92–99. https://doi.org/10.1161/circimaging.113.000884.
Gao, Y., Aravind, S., Patel, N. S., Fuglestad, M. A., Ungar, J. S., Mietus, C. J., et al. (2020). Collateral development and arteriogenesis in hindlimbs of swine after ligation of arterial inflow. The Journal of Surgical Research, 249, 168–179. https://doi.org/10.1016/j.jss.2019.12.005.
Landázuri, N., Levit, R. D., Joseph, G., Ortega-Legaspi, J. M., Flores, C. A., Weiss, D., et al. (2016). Alginate microencapsulation of human mesenchymal stem cells as a strategy to enhance paracrine-mediated vascular recovery after hindlimb ischaemia. Journal of Tissue Engineering and Regenerative Medicine, 10(3), 222–232. https://doi.org/10.1002/term.1680.
Krueger, T. E. G., Thorek, D. L. J., Denmeade, S. R., Isaacs, J. T., & Brennen, W. N. (2018). Concise review: mesenchymal stem cell-based drug delivery: the good, the bad, the ugly, and the promise. Stem Cells Translational Medicine, 7(9), 651–663. https://doi.org/10.1002/sctm.18-0024.
Gyöngyösi, M., Blanco, J., Marian, T., Trón, L., Petneházy, Ö., Petrasi, Z., et al. (2008). Serial noninvasive in vivo positron emission tomographic tracking of percutaneously intramyocardially injected autologous porcine mesenchymal stem cells modified for transgene reporter gene rxpression. Circulation. Cardiovascular Imaging, 1(2), 94–103. https://doi.org/10.1161/circimaging.108.797449.
Gibson, C. M., Ryan, K., Sparano, A., Moynihan, J. L., Rizzo, M., Kelley, M., et al. (1999). Angiographic methods to assess human coronary angiogenesis. American Heart Journal, 137(1), 169–179. https://doi.org/10.1016/S0002-8703(99)70473-4.
Powers, K. M., Schimmel, C., Glenny, R. W., & Bernards, C. M. (1999). Cerebral blood flow determinations using fluorescent microspheres: variations on the sedimentation method validated. Journal of Neuroscience Methods, 87(2), 159–165.
Wen, Y., Murach, K. A., Vechetti Jr., I. J., Fry, C. S., Vickery, C., Peterson, C. A., et al. (2018). MyoVision: software for automated high-content analysis of skeletal muscle immunohistochemistry. Journal of Applied Physiology (Bethesda, MD: 1985), 124(1), 40–51. https://doi.org/10.1152/japplphysiol.00762.2017.
Rotstein, B. H., Stephenson, N. A., Vasdev, N., & Liang, S. H. (2014). Spirocyclic hypervalent iodine(III)-mediated radiofluorination of non-activated and hindered aromatics. Nature Communications, 5, 4365. https://doi.org/10.1038/ncomms5365.
Rotstein, B. H., Wang, L., Liu, R. Y., Patteson, J., Kwan, E. E., Vasdev, N., et al. (2016). Mechanistic studies and radiofluorination of structurally diverse pharmaceuticals with spirocyclic iodonium(III) Ylides. Chemical Science, 7(7), 4407–4417. https://doi.org/10.1039/c6sc00197a.
Moroz, M. A., Zhang, H., Lee, J., Moroz, E., Zurita, J., Shenker, L., et al. (2015). Comparative analysis of T cell imaging with human nuclear reporter genes. Journal of nuclear medicine : official publication, Society of Nuclear Medicine, 56(7), 1055–1060. https://doi.org/10.2967/jnumed.115.159855.
Pandit-Taskar, N., Zanzonico, P., Staton, K. D., Carrasquillo, J. A., Reidy-Lagunes, D., Lyashchenko, S., et al. (2018). Biodistribution and dosimetry of (18)F-meta-fluorobenzylguanidine: a first-in-human PET/CT imaging study of patients with neuroendocrine malignancies. Journal of Nuclear Medicine, 59(1), 147–153. https://doi.org/10.2967/jnumed.117.193169.
Koutakis, P., Myers, S. A., Cluff, K., Ha, D. M., Haynatzki, G., McComb, R. D., et al. (2015). Abnormal myofiber morphology and limb dysfunction in claudication. The Journal of Surgical Research, 196(1), 172–179. https://doi.org/10.1016/j.jss.2015.02.011.
Kakihana, T., Ito, O., Sekiguchi, Y., Ito, D., Goto, H., Akamatsu, D., et al. (2017). Hip flexor muscle dysfunction during walking at self-selected and fast speed in patients with aortoiliac peripheral arterial disease. Journal of Vascular Surgery, 66(2), 523–532. https://doi.org/10.1016/j.jvs.2017.03.421.
Kaiser, E. E., Waters, E. S., Fagan, M. M., Scheulin, K. M., Platt, S. R., Jeon, J. H., et al. (2020). Characterization of tissue and functional deficits in a clinically translational pig model of acute ischemic stroke. Brain Research, 1736, 146778. https://doi.org/10.1016/j.brainres.2020.146778.
Hedayat, A. F., Park, K. H., Kwon, T. G., Woollard, J. R., Jiang, K., Carlson, D. F., et al. (2018). Peripheral vascular atherosclerosis in a novel PCSK9 gain-of-function mutant Ossabaw miniature pig model. Translational Research, 192, 30–45. https://doi.org/10.1016/j.trsl.2017.10.007.
Heinonen, I., Kemppainen, J., Kaskinoro, K., Peltonen, J. E., Borra, R., Lindroos, M. M., et al. (2010). Comparison of exogenous adenosine and voluntary exercise on human skeletal muscle perfusion and perfusion heterogeneity. Journal of Applied Physiology (Bethesda, MD: 1985), 108(2), 378–386. https://doi.org/10.1152/japplphysiol.00745.2009.
Armstrong, R. B., Delp, M. D., Goljan, E. F., & Laughlin, M. H. (1987). Distribution of blood flow in muscles of miniature swine during exercise. Journal of Applied Physiology (Bethesda, MD: 1985), 62(3), 1285–1298. https://doi.org/10.1152/jappl.1987.62.3.1285.
Varu, V. N., Hogg, M. E., & Kibbe, M. R. (2010). Critical limb ischemia. Journal of Vascular Surgery, 51(1), 230–241. https://doi.org/10.1016/j.jvs.2009.08.073.
Kościński, K., Kozłowska-Rajewicz, A., Górecki, M. T., Kamyczek, M., & Różycki, M. (2009). Month-of-birth effect on further body size in a pig model. HOMO, 60(2), 159–183. https://doi.org/10.1016/j.jchb.2008.02.003.
Dubreuil, P., Pelletier, G., Petitclerc, D., Lapierre, H., Couture, Y., Brazeau, P., et al. (1987). Influence of age and sex on basal secretion of growth hormone (GH) and on GH-induced release by porcine GH-releasing factor pGRF(1–29NH2) in growing pigs. Domestic Animal Endocrinology, 4(4), 299–307. https://doi.org/10.1016/0739-7240(87)90026-9.
Caicedo, D., Devesa, P., Alvarez, C. V., & Devesa, J. (2020). Why should growth hormone (GH) be considered a promising therapeutic agent for arteriogenesis? Insights from the GHAS trial. Cells, 9(4). https://doi.org/10.3390/cells9040807.
Erman, A., Wabitsch, M., & Goodyer, C. G. (2011). Human growth hormone receptor (GHR) expression in obesity: II. Regulation of the human GHR gene by obesity-related factors. International Journal of Obesity, 35(12), 1520–1529. https://doi.org/10.1038/ijo.2011.10.
van der Bogt, K. E., Hellingman, A. A., Lijkwan, M. A., Bos, E. J., de Vries, M. R., van Rappard, J. R., et al. (2012). Molecular imaging of bone marrow mononuclear cell survival and homing in murine peripheral artery disease. JACC: Cardiovascular Imaging, 5(1), 46–55. https://doi.org/10.1016/j.jcmg.2011.07.011.
Acknowledgements
We thank T3 Labs for swine experiment organization and technical expertise.
Funding
These data were generated with support of the Aronov Foundation, the Emory University Center for Systems Imaging Pilot Funding, the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH) under Award Numbers UL1TR002378 and TL1TR002382 (J.N.D), and R01HL140223 (R.D.L.). Experiments were performed in part using the Microscopy in Medicine Core (NIH grant P01HL095070) and the Emory Integrated Genomics Core (subsidized by the Emory University School of Medicine and additionally supported by NIH Award Number UL1TR002378). The content is solely the responsibility of the authors and does not necessarily represent the views of NIH.
Author information
Authors and Affiliations
Contributions
Conceptualization: JND and RDL. Formal analysis: JND, SCG, and NHK. Funding acquisition: JND and RDL. Investigation: JND, SCG, NHK, LW, RJV, and JNO. Methodology: JND, RJV, SHL, MMG, JNO, and RDL. Project administration: MMG and RDL. Resources: LW, SHL, and MMG. Supervision: RDL. Visualization: JND and JNO. Writing—original draft preparation: JND. Writing—review and editing: JND, SCG, NHK, LW, RJV, MMG, JNO, and RDL.
Corresponding author
Ethics declarations
Ethical Approval
No human studies were performed. All institutional and national guidelines for laboratory animal care and use were followed and approved by institutional committees at T3 Labs and Emory University for swine and rat studies, respectively.
Competing interests
The authors declare no conflicts of interest.
Additional information
Associate Editor Nicola Smart oversaw the review of this article
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(PDF 493 kb)
Rights and permissions
About this article
Cite this article
Deppen, J.N., Ginn, S.C., Kim, N.H. et al. A Swine Hind Limb Ischemia Model Useful for Testing Peripheral Artery Disease Therapeutics. J. of Cardiovasc. Trans. Res. 14, 1186–1197 (2021). https://doi.org/10.1007/s12265-021-10134-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-021-10134-8