Abstract
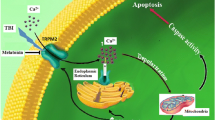
Ischemia/reperfusion (I/R) is among the most frequent neurological problems and early intervention to limit the damage is crucial in decreasing mortality and morbidity. Based on reports regarding beneficial effects of melatonin, we investigated its impact on Na+-K+/Mg2+ ATPase and Ca2+/Mg2+ ATPase activities and ultrastructure of gray and white matter in the rat forebrain I/R model. Adult Wistar-albino rats (n = 78), were randomized into control, ischemia (I), ischemia/reperfusion (I/R), low (I/R + melatonin 400 µg/kg), moderate (I/R + melatonin 1200 µg/kg), and high (I/R + melatonin 2400 µg/kg) dose melatonin. Two-vessel occlusion combined with hypotension (15 min) induced ischemia and reperfusion (75 min) achieved by blood reinfusion were performed. Activities of the membrane-bound enzyme, brain malondialdehyde levels, and brain matter ultrastructure were examined in frontoparietal cortices. Melatonin lowered production of malondialdehyde in a dose-dependently. The enzyme activities attenuated under I and I/R, improved with melatonin treatment. I and I/R severely disturbed gray and white matter morphology. Melatonin, in all applied doses, decreased ultrastructural damages in both gray and white matter. Favorable effects of melatonin can be attributed to its antioxidant properties suggesting that it could be a promising neuroprotective agent against I/R injury being effective both for gray and white matter due to favorable biological properties.




Similar content being viewed by others
Abbreviations
- EEG:
-
electroencephalography
- I/R:
-
ischemia/reperfusion
- MABP:
-
mean arterial blood pressure
- MDA:
-
malondialdehyde
References
Lee, R. H. C., Lee, M. H. H., Wu, C. Y. C., Couto, E. S. A., Possoit, H. E., et al. (2018) Cerebral ischemia and neuroregeneration, Neural Regen. Res., 13, 373-385, https://doi.org/10.4103/1673-5374.228711.
Granger, D. N., and Kvietys, P. R. (2015) Reperfusion injury and reactive oxygen species: the evolution of a concept, Redox Biol., 6, 524-551, https://doi.org/10.1016/j.redox.2015.08.020.
Li, Y., and Yang, G.-Y. (2017) Pathophysiology of ischemic stroke, in Translational Research in Stroke (Lapchak, P. A., and Yang, G.-Y., eds.) 1st Edn., Springer Singapore, pp. 51-75.
Kalogeris, T., Baines, C. P., Krenz, M., and Korthuis, R. J. (2012) Cell biology of ischemia/reperfusion injury, Int. Rev. Cell. Mol. Biol., 298, 229-317, https://doi.org/10.1016/b978-0-12-394309-5.00006-7.
Godinho, J., de Sa-Nakanishi, A. B., Moreira, L. S., de Oliveira, R. M. W., Huzita, C. H., et al. (2018) Ethyl-acetate fraction of Trichilia catigua protects against oxidative stress and neuroinflammation after cerebral ischemia/reperfusion, J. Ethnopharmacol., 221, 109-118, https://doi.org/10.1016/j.jep.2018.04.018.
Phaniendra, A., Jestadi, D. B., and Periyasamy, L. (2015) Free radicals: properties, sources, targets, and their implication in various diseases, Indian J. Clin. Biochem., 30, 11-26, https://doi.org/10.1007/s12291-014-0446-0.
Rodrigo, R., Fernández-Gajardo, R., Gutiérrez, R., Matamala, J. M., Carrasco, R., et al. (2013) Oxidative stress and pathophysiology of ischemic stroke: novel therapeutic opportunities, CNS Neurol. Disord. Drug Targets, 12, 698-714, https://doi.org/10.2174/1871527311312050015.
Weston, R. M., Jones, N. M., Jarrott, B., and Callaway, J. K. (2007) Inflammatory cell infiltration after endothelin-1-induced cerebral ischemia: histochemical and myeloperoxidase correlation with temporal changes in brain injury, J. Cereb. Blood Flow Metab., 27, 100-114, https://doi.org/10.1038/sj.jcbfm.9600324.
Ma, Z., Xin, Z., Di, W., Yan, X., Li, X., et al. (2017) Melatonin and mitochondrial function during ischemia/reperfusion injury, Cell. Mol. Life Sci., 74, 3989-3998, https://doi.org/10.1007/s00018-017-2618-6.
Hu, S., Zhu, P., Zhou, H., Zhang, Y., and Chen, Y. (2018) Melatonin-induced protective effects on cardiomyocytes against reperfusion injury partly through modulation of IP3R and SERCA2a via activation of ERK1, Arq. Bras. Cardiol., 110, 44-51, https://doi.org/10.5935/abc.20180008.
Lin, Y. W., Chen, T. Y., Hung, C. Y., Tai, S. H., Huang, S. Y., et al. (2018) Melatonin protects brain against ischemia/reperfusion injury by attenuating endoplasmic reticulum stress, Int. J. Mol. Med., 42, 182-192, https://doi.org/10.3892/ijmm.2018.3607.
Blanco, S., Hernández, R., Franchelli, G., Ramos-Álvarez, M. M., and Peinado, M. (2017) Melatonin influences NO/NOS pathway and reduces oxidative and nitrosative stress in a model of hypoxic-ischemic brain damage, Nitric Oxide, 62, 32-43, https://doi.org/10.1016/j.niox.2016.12.001.
Yawno, T., Mahen, M., Li, J., Fahey, M. C., Jenkin, G., and Miller, S. L. (2017) The beneficial effects of melatonin administration following hypoxia-ischemia in preterm fetal sheep, Front. Cell Neurosci., 11, 296, https://doi.org/10.3389/fncel.2017.00296.
Chakravarty, S., and Rizvi, S. I. (2011) Circadian modulation of sodium-potassium ATPase and sodium – proton exchanger in human erythrocytes: in vitro effect of melatonin, Cell Mol. Biol. (Noisy-le-Grand), 57, 80-86.
Toklu, H. Z., Deniz, M., Yuksel, M., and Keyer-Uysal, M. (2009) The protective effect of melatonin and amlodipine against cerebral ischemia/reperfusion-induced oxidative brain injury in rats, Marmara Med. J., 22, 34-44.
Hoffmann, U., Sheng, H., Ayata, C., and Warner, D. S. (2016) Anesthesia in experimental stroke research, Transl. Stroke Res., 7, 358-367, https://doi.org/10.1007/s12975-016-0491-5.
Smith, M. L., Bendek, G., Dahlgren, N., Rosén, I., Wieloch, T., and Siesjö, B. K. (1984) Models for studying long-term recovery following forebrain ischemia in the rat. 2. A 2-vessel occlusion model, Acta Neurol. Scand., 69, 385-401, https://doi.org/10.1111/j.1600-0404.1984.tb07822.x.
Ildan, F., Oner, A., Polat, S., Isbir, T., Göcer, A. I., et al. (1995) Correlation of alterations on Na+-K+/Mg+2 ATPase activity, lipid peroxidation and ultrastructural findings following experimental spinal cord injury with and without intravenous methylprednisolone treatment, Neurosurg. Rev., 18, 35-44, https://doi.org/10.1007/bf00416476.
Ildan, F., Göçer, A. I., Tuna, M., Polat, S., Kaya, M., et al. (2001) The effects of the pre-treatment of intravenous nimodipine on Na+-K+/Mg+2 ATPase, Ca+2/Mg+2 ATPase, lipid peroxidation and early ultrastructural findings following middle cerebral artery occlusion in the rat, Neurol. Res., 23, 96-104, https://doi.org/10.1179/016164101101198208.
Reading, H. W., and Isbir, T. (1980) The role of cation-activated ATPases in transmitter release from the rat iris, Q. J. Exp. Physiol. Cogn. Med. Sci., 65, 105-116, https://doi.org/10.1113/expphysiol.1980.sp002495.
Peterson, M. E., Daniel, R. M., Danson, M. J., and Eisenthal, R. (2007) The dependence of enzyme activity on temperature: determination and validation of parameters, Biochem. J., 402, 331-337, https://doi.org/10.1042/bj20061143.
Atkinson, A., Gatenby, A. D., and Lowe, A. G. (1973) The determination of inorganic orthophosphate in biological systems, Biochim. Biophys. Acta, 320, 195-204, https://doi.org/10.1016/0304-4165(73)90178-5.
Reading, H. W., and Isbir, T. (1979) Action of lithium on ATPases in the rat iris and visual cortex, Biochem. Pharmacol., 28, 3471-3474, https://doi.org/10.1016/0006-2952(79)90089-3.
Lowry, O. H., Rosebrough, N. J., Farr, A. L., and Randall, R. J. (1951) Protein measurement with the Folin phenol reagent, J. Biol. Chem., 193, 265-275.
Görgülü, A., Palaoğlu, S., Ismailoğlu, O., Tuncel, M., Sürücü, M. T., et al. (2001) Effect of melatonin on cerebral edema in rats, Neurosurgery, 49, 1434-1442, https://doi.org/10.1097/00006123-200112000-00024.
Kaptanoglu, E., Palaoglu, S., Surucu, H. S., Hayran, M., and Beskonakli, E. (2002) Ultrastructural scoring of graded acute spinal cord injury in the rat, J. Neurosurg., 97, 49-56, https://doi.org/10.3171/spi.2002.97.1.0049.
Lee, M. Y., Kuan, Y. H., Chen, H. Y., Chen, T. Y., Chen, S. T., et al. (2007) Intravenous administration of melatonin reduces the intracerebral cellular inflammatory response following transient focal cerebral ischemia in rats, J. Pineal Res., 42, 297-309, https://doi.org/10.1111/j.1600-079X.2007.00420.x.
Ramis, M. R., Esteban, S., Miralles, A., Tan, D. X., and Reiter, R. J. (2015) Protective effects of melatonin and mitochondria-targeted antioxidants against oxidative stress: a review, Curr. Med. Chem., 22, 2690-2711, https://doi.org/10.2174/0929867322666150619104143.
Cervantes, M., Moralí, G., and Letechipía-Vallejo, G. (2008) Melatonin and ischemia-reperfusion injury of the brain, J. Pineal Res., 45, 1-7, https://doi.org/10.1111/j.1600-079X.2007.00551.x.
Gim, S. A., and Koh, P. O. (2015) Melatonin attenuates hepatic ischemia through mitogen-activated protein kinase signaling, J. Surg. Res., 198, 228-236, https://doi.org/10.1016/j.jss.2015.05.043.
Santofimia-Castaño, P., Clea Ruy, D., Garcia-Sanchez, L., Jimenez-Blasco, D., Fernandez-Bermejo, M., et al. (2015) Melatonin induces the expression of Nrf2-regulated antioxidant enzymes via PKC and Ca2+ influx activation in mouse pancreatic acinar cells, Free Radic. Biol. Med., 87, 226-236, https://doi.org/10.1016/j.freeradbiomed.2015.06.033.
Reiter, R. J., Sainz, R. M., Lopez-Burillo, S., Mayo, J. C., Manchester, L. C., and Tan, D. X. (2003) Melatonin ameliorates neurologic damage and neurophysiologic deficits in experimental models of stroke, Ann. N.Y. Acad. Sci., 993, 35-47, https://doi.org/10.1111/j.1749-6632.2003.tb07509.x.
Tütüncüler, F., Eskiocak, S., Başaran, U. N., Ekuklu, G., Ayvaz, S., and Vatansever, U. (2005) The protective role of melatonin in experimental hypoxic brain damage, Pediatr. Int., 47, 434-439, https://doi.org/10.1111/j.1442-200x.2005.02085.x.
Reiter, R. J., Tan, D. X., Leon, J., Kilic, U., and Kilic, E. (2005) When melatonin gets on your nerves: its beneficial actions in experimental models of stroke, Exp. Biol. Med. (Maywood), 230, 104-117, https://doi.org/10.1177/153537020523000205.
Tan, D. X., Manchester, L. C., Terron, M. P., Flores, L. J., and Reiter, R. J. (2007) One molecule, many derivatives: a never-ending interaction of melatonin with reactive oxygen and nitrogen species?, J. Pineal Res., 42, 28-42, https://doi.org/10.1111/j.1600-079X.2006.00407.x.
De Lores Arnaiz, G. R., and Ordieres, M. G. (2014) Brain Na+,K+-ATPase activity in aging and disease, Int. J. Biomed. Sci., 10, 85-102.
Harris, J. J., and Attwell, D. (2012) The energetics of CNS white matter, J. Neurosci., 32, 356-371, https://doi.org/10.1523/jneurosci.3430-11.2012.
Domercq, M., Sánchez-Gómez, M. V., Sherwin, C., Etxebarria, E., Fern, R., and Matute, C. (2007) System xc- and glutamate transporter inhibition mediates microglial toxicity to oligodendrocytes, J. Immunol., 178, 6549-6556, https://doi.org/10.4049/jimmunol.178.10.6549.
Micu, I., Jiang, Q., Coderre, E., Ridsdale, A., Zhang, L., et al. (2006) NMDA receptors mediate calcium accumulation in myelin during chemical ischaemia, Nature, 439, 988-992, https://doi.org/10.1038/nature04474.
Wang, Y., Liu, G., Hong, D., Chen, F., Ji, X., and Cao, G. (2016) White matter injury in ischemic stroke, Prog. Neurobiol., 141, 45-60, https://doi.org/10.1016/j.pneurobio.2016.04.005.
Matute, C., Domercq, M., Pérez-Samartín, A., and Ransom, B. R. (2013) Protecting white matter from stroke injury, Stroke, 44, 1204-1211, https://doi.org/10.1161/strokeaha.112.658328.
Pappas, B. A., Davidson, C. M., Bennett, S. A., de la Torre, J. C., Fortin, T., and Tenniswood, M. P. (1997) Chronic ischemia: memory impairment and neural pathology in the rat, Ann. N.Y. Acad. Sci., 826, 498-501, https://doi.org/10.1111/j.1749-6632.1997.tb48512.x.
Sozmen, E. G., Kolekar, A., Havton, L. A., and Carmichael, S. T. (2009) A white matter stroke model in the mouse: axonal damage, progenitor responses and MRI correlates, J. Neurosci. Methods, 180, 261-272, https://doi.org/10.1016/j.jneumeth.2009.03.017.
Rossi, D. J., Brady, J. D., and Mohr, C. (2007) Astrocyte metabolism and signaling during brain ischemia, Nat. Neurosci., 10, 1377-1386, https://doi.org/10.1038/nn2004.
Nedergaard, M., and Dirnagl, U. (2005) Role of glial cells in cerebral ischemia, Glia, 50, 281-286, https://doi.org/10.1002/glia.20205.
Sekerdag, E., Solaroglu, I., and Gursoy-Ozdemir, Y. (2018) Cell death mechanisms in stroke and novel molecular and cellular treatment options, Curr. Neuropharmacol., 16, 1396-1415, https://doi.org/10.2174/1570159x16666180302115544.
Acknowledgments
The authors are grateful to Prof. Z. Dicle Balkancı, MD, Retired Professor of Physiology, for her critical contributions to the study and to Prof. A. Ergun Karaağaoğlu PhD, Professor of Biostatistics, for his involvement in statistical analysis.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Meltem Tuncer and Bilge Pehlivanoğlu. Ultrastructural analysis was performed by Selçuk Sürücü and Biochemical measurements were carried out by Turgay İsbir. The first draft of the manuscript was written by Meltem Tuncer and Bilge Pehlivanoğlu; all authors commented on the previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
The authors declare no conflict of interest in financial or any other sphere. All applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
Rights and permissions
About this article
Cite this article
Tuncer, M., Pehlivanoglu, B., Sürücü, S.H. et al. Melatonin Improves Reduced Activities of Membrane ATPases and Preserves Ultrastructure of Gray and White Matter in the Rat Brain Ischemia/Reperfusion Model. Biochemistry Moscow 86, 540–550 (2021). https://doi.org/10.1134/S0006297921050035
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S0006297921050035