Abstract
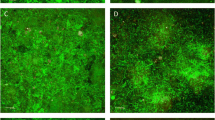
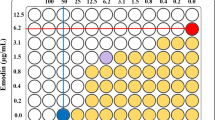
Antibacterial photodynamic therapy (aPDT) has drawn increasing attention as a noninvasive approach to remove bacterial contaminants such as E. faecalis from the tooth surface. In this study, curcumin (CUR) was loaded into ZSM-5 zeolite and the prepared photosensitizers (CUR@ZSM) were characterized by Fourier transform infrared spectroscopy (FT-IR), X-ray diffraction (XRD), scanning electron microscopy (SEM), and ultraviolet–visible spectroscopy (UV–Vis). The loading efficiency, and release behavior of CUR were studied in CUR@ZSM. The antimicrobial and anti-biofilm potential of the photosensitizer were evaluated against E. faecalis via colony forming unit and crystal violet assays, respectively. No significant changes were observed in the size, morphology and crystallinity of the zeolite after CUR loading. CUR@ZSM showed a significant photodynamic inactivation effect through complete bacterial elimination and reduced the biofilm formation ability of E. faecalis up to about 80%. The results revealed that CUR@ZSM could be considered as a new potential photosensitizer for further study against endodontic infections.






Similar content being viewed by others
References
V. Peciuliene, R. Maneliene, E. Balcikonyte, S. Drukteinis, and V. Rutkunas (2008). Microorganisms in root canal infections: a review. Stomatologija 10, 4–9.
J. F. Siqueira Jr. and I. N. Rocas (2009). Diversity of endodontic microbiota revisited. J. Dent. Res. 88, 969–981.
H. H. Hancock, A. Sigurdsson, M. Trope, and J. Moiseiwitsch (2001). Bacteria isolated after unsuccessful endodontic treatment in a North American population. Oral Surg. Oral. Med. Oral Pathol. Oral Radiol. Endodontol. 91, 579–586.
R. M. Love (2001). Enterococcus faecalis—a mechanism for its role in endodontic failure. Int. Endod. J. 34, 399–405.
D. Figdor, R. M. Davies, and G. Sundqvist (2003). Starvation survival, growth and recovery of Enterococcus faecalis in human serum. Oral Microbiol. Immunol. 18, 234–239.
L. Wang, M. Dong, J. Zheng, Q. Song, W. Yin, J. Li, and W. Niu (2011). Relationship of biofilm formation and gelE gene expression in Enterococcus faecalis recovered from root canals in patients requiring endodontic retreatment. J. Endod. 37, 631–636.
L. López-Jiménez, E. Fusté, B. Martínez-Garriga, J. Arnabat-Domínguez, T. Vinuesa, and M. Viñas (2015). Effects of photodynamic therapy on Enterococcus Faecalis biofilms. Lasers Med. Sci. 5, 1519–1526.
L. Tabenski, W. Buchalla, and T. Maisch (2014). Antimicrobial photodynamic therapy for inactivation of biofilms formed by oral key pathogens. Front. Microbiol. 5, 1–17.
W. M. Sharman, C. M. Allen, and J. E. van Lier (1999). Photodynamic therapeutics: basic principles and clinical applications. Drug Discov. Today. 11, 507–517.
M. R. Hamblin and T. Hasan (2004). Photodynamic therapy: a new antimicrobial approach to infectious disease? Photochem. Photobiol. Sci. 3, 436–450.
L. Huang, T. Dai, and M. R. Hamblin (2010). Antimicrobial photodynamic inactivation and photodynamic therapy for infections. Methods Mol. Biol. 635, 155–173.
A. Persadmehr, C. D. Torneck, D. G. Cvitkovitch, V. Pinto, I. Talior, M. Kazembe, S. Shrestha, C. A. McCulloch, and A. Kishen (2014). Bioactive chitosan nanoparticles and photodynamic therapy inhibit collagen degradation in vitro. J. Endod. 40, 703–709.
L. N. Dovigo, A. C. Pavarina, J. C. Carmello, A. L. Machado, I. L. Brunetti, and V. S. Bagnato (2011). Susceptibility of clinical isolates of Candida to photodynamic effects of Curcumin. Lasers Surg. Med. 43, 927–934.
N. C. Araujo, C. R. Fontana, M. E. Gerbi, and V. S. Bagnato (2012). Overall-mouth disinfection by photodynamic therapy using Curcumin. Photomed. Laser Surg. 30, 96–101.
Sh. Devaraj, N. Jagannathan, and P. Neelakantan (2016). Antibiofilm efficacy of photoactivated Curcumin, triple and double antibiotic paste, 2% chlorhexidine and calcium hydroxide against Enterococcus faecalis in vitro. Sci. Rep. 6, 24797.
T. A. Dahl, P. Bilski, K. J. Reszka, and C. F. Chignell (1994). Photocytotoxicity of Curcumin. Photochem. Photobiol. 59, 290–294.
K. O. Wikene, A. B. Hegge, E. Bruzell, and H. H. Tonnesen (2015). Formulation and characterization of lyophilized curcumin solid dispersions for antimicrobial photodynamic therapy (aPDT): studies on curcuminand curcuminoids LII. Drug Dev. Ind. Pharm. 41, 969–977.
Q. Q. Yanga, A. K. Farhaa, G. Kima, K. Gula, R.-Y. Ganb, and H. Corkea (2020). Antimicrobial and anticancer applications and related mechanisms of curcumin-mediated photodynamic treatments. Trends Food Sci. Technol. 97, 341–354.
M. Pourhajibagher, N. Chiniforush, A. Monzavi, H. Barikani, M. Monzavi, S. Sobhani, S. Shahabi, and A. Bahador (2018). Inhibitory effects of antimicrobial photodynamic therapy with Curcumin on biofilm-associated gene expression profile of Aggregatibacter actinomycetemcomitans. J. Dent. (Tehran) 15, 169–177.
J. Ma, H. Shi, H. Sun, J. Li, and Y. Bai (2019). Antifungal effect of photodynamic therapy mediated by Curcumin on Candida albicans biofilms in vitro. Photodiagn. Photodyn. Ther. 27, 280–287.
H. Lee, S. Kang, S. Jeong, K. Chung, and B. Kim (2017). Antibacterial photodynamic therapy with Curcumin and Curcuma xanthorrhiza extract against Streptococcus mutans. Photodiagn. Photodyn. Ther. 20, 116–119.
R. Amorim, N. Vilaça, O. Martinho, R. M. Reis, M. Sardo, J. Rocha, M. Fonseca, F. Baltazar, and I. C. Neves (2012). Zeolite structures loading with an anticancer compound as drug delivery systems. J. Phys. Chem. C 116, 25642–25650.
Z. Ahali Abadeh, G. Saviano, P. Ballirano, and G. Santonicalo (2020). Curcumin-loaded Zeolite as anticancer drug carrier: effect of curcumin adsorption on zeolite structure. Pure Appl. Chem. 92, 461–471.
P. Tavolaro, S. Catalano, G. Martino, and A. Tavolaro (2016). Zeolite inorganic scaffolds for novel biomedical application: effect of physicochemical characteristic of zeolite membranes on cell adhesion and viability. Appl. Surf. Sci. 380, 135–140.
P. Tavolaro, G. Martino, S. Andò, and A. Tavolaro (2016). Fabrication and evaluation of novel zeolite membranes to control the neoplastic activity and anti-tumoral drug treatments in human breast cancer cells. Part 1: Synthesis and characterization of Pure Zeolite Membranes and Mixed Matrix Membranes for adhesion and growth of cancer cells. Mater. Sci. Eng. C 69, 894–904.
G. Tegl, V. Stagl, A. Mensah, D. Huber, W. Somitsch, S. Grosse-Kracht, and G. M. Guebitz (2018). The chemo enzymatic functionalization of chitosan zeolite particles provides antioxidant and antimicrobial properties. Eng. Life Sci. 18, 334–340.
T. Akbari, M. Pourhajibagher, F. Hosseini, N. Chiniforush, E. Gholibegloo, M. Khoobi, S. Shahabi, and A. Bahador (2017). The effect of indocyanine green loaded on a novel nano-graphene oxide for high performance of photodynamic therapy against Enterococcus faecalis. Photodiagn. Photodyn. Ther. 20, 148–153.
E. Gholibegloo, A. Karbasi, M. Pourhajibagher, N. Chiniforush, A. Ramazani, T. Akbari, A. Bahador, and M. Khoobi (2018). Carnosine-graphene oxide conjugates decorated with hydroxyapatite as promising nanocarrier for ICG loading with enhanced antibacterial effects in photodynamic therapy against Streptococcus Mutans. J. Photochem. Photobiol. B 181, 14–22.
M. M. Yallapu, S. F. Othman, E. T. Curtis, N. A. Bauer, N. Chauhan, D. Kumar, M. S. Jaggi, and C. Chauhan (2012). Curcumin-loaded magnetic nanoparticles for breast cancer therapeutics and imaging applications. Int. J. Nanomed. 7, 1761–1779.
N. Chiniforush, M. Pourhajibagher, S. Parker, S. Shahabi, and A. Bahador (2016). The in vitro effect of antimicrobial photodynamic therapy with indocyanine green on Enterococcus faecalis: influence of a washing vs non-washing procedure. Photodiagn. Photodyn. Ther. 16, 119–123.
A. A. Miles, S. S. Misra, and J. O. Irwin (1938). The estimation of bactericidal power of the blood. J. Hyg. 38, 732–749.
Y. Cheng, L. J. Wang, J. S. Li, Y. C. Yang, and X. Y. Sun (2005). Preparation and characterization of nanosized ZSM-5 zeolites in the absence of organic template. Mater Lett. 59, 3427–3430.
P. Morales-Pacheco, J. Dominguez, L. Bucio, F. Alvarez, U. Sedran, and M. Falco (2011). Synthesis of FAU (Y)-and MFI (ZSM5)-nanosized crystallites for catalytic cracking of 1,3,5-triisopropylbenzene. Catal. Today 166, 25–38.
J. Cejka, H. Van Bekkum, A. Corma, and F. Schueth, Introduction to zeolite molecular sieves, vol. 168 (Elsevier Science, Amsterdam , 2007).
Z. Ahali Abadeh, G. Saviano, P. Ballirano, and M. G. Santonicola (2019) Curcumin-loaded zeolite as anticancer drug carrier: effect of curcumin adsorption on zeolite structure. Pure Appl. Chem., 1–11.
M. Karimi, M. Habibizad, K. Rostamizadeh, M. Khatamian, and B. Divband (2019). Preparation and characterization of nanocomposites based on different zeolite frameworks as carriers for anticancer drug: zeolite Y versus ZSM-5. Polym. Bull. 76, 2233–2252.
Mk. Amosa, M. AlKhatib, M. Jami, D. Jimat, O. Uthman, and S. Muyibi (2014). Morphological synthesis and environmental application of ZSM-5 zeolite crystals from combined low-water and fluoride syntheses routes. Adv. Environ. Biol. 8, 613–625.
A. Ameri, T. Taghizadeh, A. Talebian-Kiakalaieh, H. Forootanfar, S. Mojtabavi, H. Jahandar, S. Tarighi, and M. A. Faramarzi (2021). Bio-removal of phenol by the immobilized laccase on the fabricated parent and hierarchical NaY and ZSM-5 zeolites. J. Taiwan Inst. Chem. Eng. 120, 300–312.
T. M. Kolev, E. A. Velcheva, B. A. Stamboliyska, and M. Spiteller (2005). DFT and experimental studies of the structure and vibrational spectra of Curcumin. Int. J. Quantum Chem. 102, 1069–1079.
X. Li, Q. Yang, J. Ouyang, H. Yang, and S. Chang (2016). Chitosan modified halloysite nanotubes as emerging porous microspheres for drug carrier. Appl. Clay Sci. 126, 306–312.
D. Preisig, D. Haid, F. J. O. Varum, R. Bravo, R. Alles, J. Huwyler, and M. Puchkov (2014). Drug loading into porous calcium carbonate microparticles by solvent evaporation. Eur. J. Pharm. Biopharm. 87, 548–558.
L. A. Silva, A. B. Novaes Jr., R. R. de Oliveira, P. Nelson-Filho, M. Santamaria Jr., and R. A. Silva (2012). Antimicrobial photodynamic therapy for the treatment of teeth with apical periodontitis: a histopathological evaluation. J. Endod. 38, 360–366.
G. Pileggi, J. C. Wataha, M. Girard, I. Grad, J. Schrenzel, N. Lange, and S. Bouillaguet (2013). Blue light-mediated inactivation of Enterococcus faecalis in vitro. Photodiagn. Photodyn. Ther. 10, 134–140.
P. Neelakantan, C. Q. Cheng, V. Ravichandran, T. Maoa, P. Sriraman, S. Sridharan, Ch. Subbarao, S. Sharma, and A. Kishen (2015). Photoactivation of curcumin and sodium hypochlorite to enhance antibiofilm efficacy in root canal dentin. Photodiagn. Photodyn. Ther. 12, 108–114.
M. Pourhajibagher, N. Chiniforush, S. Shahabi, R. Ghorbanzadeh, and A. Bahador (2016). Sub-lethal doses of photodynamic therapy affect biofilm formation ability and metabolic activity of Enterococcus faecalis. Photodiagn. Photodyn. Ther. 15, 159–166.
A. B. Hegge, T. Andersen, J. E. Melvik, E. Bruzell, S. Kristensen, and H. H. Tonnesen (2011). Formulation and bacterial phototoxicity of Curcumin loaded alginate foams for wound treatment applications: studies on Curcumin and curcuminoides XLII. J. Pharm. Sci. 100, 174–185.
A. B. Hegge, T. T. Nielson, K. L. Larsen, E. Bruzell, and H. H. Tonnesen (2012). Impact of curcumin supersaturation in antibacterial photodynamic therapy-effect of cyclodextrin type and amount: studies on Curcumin and curcuminoides XLV. J. Pharm. Sci. 101, 1524–1537.
M. Smolinska, G. Cik, F. Sersen, M. Caplovicova, A. Takacova, and M. Kopanica (2015). The hybrid Methylene blue–Zeolite system: a higher efficient photocatalyst for photoinactivation of pathogenic microorganisms. Int. J. Environ. Sci. Technol. 12, 61–72.
Y. Kohno, Y. Shibata, N. Oyaizu, K. Yoda, M. Shibata, and R. Matsushima (2008). Stabilization of flavylium dye by incorporation into the pore of protonated zeolites. Microporous Mesoporous Mater. 114, 373–379.
H. Kariminezhad, M. Habibi, and N. Mirzababay (2015). Nanosized ZSM-5 will improve photodynamic therapy using Methylene blue. J. Photochem. Photobiol. B 148, 107–112.
Acknowledgements
This work was supported by a grant from the Research Council of Tehran University of Medical Sciences (Grant Number: 42907).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors of this manuscript do not have any financial conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ghaedi, A., Torshabi, M., Chahrogh, A.R. et al. Enhanced Photodynamic Suppression of Enterococcus faecalis Using Curcumin-Loaded Zeolite. J Clust Sci 33, 1543–1551 (2022). https://doi.org/10.1007/s10876-021-02085-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10876-021-02085-6